The experimental study design was conducted in the Department of Physiology, at Mahatma Gandhi Medical College and Research Institute Pondicherry, during 2013 – 2014. Approval from Institutional Human Ethics Committee was obtained. Volunteers were recruited by simple random sampling method from various institutes of Sri Balaji Vidyapeeth University. Informed written consent was taken from all the participants. Brief procedure and demonstration was done to all the volunteers.
A mercury manometer is constructed and improvised with the help of authors of previous studies [10–12]. The volunteers were asked to do the tests with mouth pieces of various internal diameters to demonstrate the difference in readings which could be a reason for inability to standardize and fix normal values for regional ethnic population group.
In our apparatus we used Ryle’s tube so that other workers can easily follow the design with similar calibrations.
Materials and Methods
The subjects were made familiarized with laboratory settings, instrument and procedure for two days. By third day, the volunteers were asked to assemble at the lab 3 hours after a light breakfast.
Technique: The subjects were requested to perform the maneuver in sitting (chair / stool) with spine erect. The manometer was placed by their side, appropriate to their height. Nose clips were not used because it has been considered extraneous [13].
Maximum Inspiratory pressure
By using mercury manometer: They were instructed to breathe normally at their tidal respiration for 5 times, the 5th time; to breathe out fully (to their expiratory reserve volume). From that level, they were motivated to breathe in hard to their full limit (to their Inspiratory reserve volume) in the mouth piece. A technician was instructed to stand by the side of volunteers to ensure that they should not use cheek muscles while performing the procedure. The volunteers were requested to breathe in deeply and hold in there for minimum of 3 seconds. The maximum level they had sustained while inspiring deeply was noted. Trials were taken by the subjects till 3 readings that differ less than 2 mm Hg was obtained. The highest among the 3 reading was considered as the maximum Inspiratory pressure of the subject. The subjects were made to do the procedure many times till the difference is less than 2 mm Hg. This is mainly to avoid the error due to oscillations of mercury column. Mercury column has static inertia which makes the column to oscillate if disturbed. By asking the subject to hold in for 3 seconds, the maximum height attained by the mercury column while oscillating is been made out. Similar technical descriptions were ensured while recording maximum expiratory pressure also.
Recording with different sized mouth pieces: Similar procedure was repeated with all 3 different sizes of mouth piece. (20 ml, 10 ml, 2.5 ml) syringes with internal diameter of 2 cm, 1.5 cm, and 1 respectively.
Maximum expiratory pressure
By using mercury manometer: The volunteers were instructed to breathe normally at their tidal respiration for 5 times. By the 5th time, they were requested to breathe in fully (to their Inspiratory reserve volume). From that level, they were motivated to breathe out hard to their full limit (to their expiratory reserve volume) in the mouth piece. They were asked to keep the fingers of their other hand over the cheeks so that they don’t use their cheek muscles for blowing. The same had been verified by a technician. They were asked to breathe out deeply and hold in for minimum of 3 seconds. The maximum level they had sustained while expiring deeply was noted. Trials were taken by the subjects till 3 readings that differ less than 2 mm Hg was obtained. The highest among the 3 reading is considered as the maximum expiratory pressure of the subject.
By using sphygmomanometer: The same procedure and technique was repeated with sphygmomanometer.
Recording with different sized mouth pieces: Similar procedure was repeated with all 3 different sizes of mouth piece. (20 ml, 10 ml, 2.5 ml) syringes with internal diameter of 2 cm, 1.5 cm, and 1 respectively.
Statistical Analysis
Data were expressed as Mean±SD, along with confidence intervals. The standard deviations, standard error of mean, margin of error were calculated. This study analysed the possibility of constructing a design and hence it did not measure the relationship between variables. So, instead of finding statistical significance and measures of association, this study used Pearson correlation coefficient to analyse the linear correlation between variables. Pearson correlation was done with IBM SPSS statistics version 21.
Results
Thirty subjects of age group 17 to 19 years (mean 17.63) participated in this study. Their body mass index was 21.63 ± 3.03 with a 95% confidence interval of 1.09.
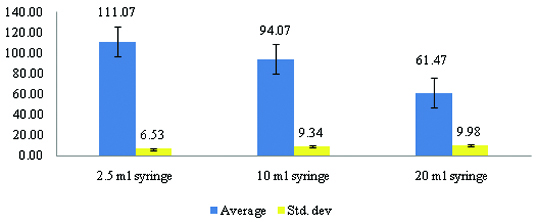
Maximum inspiratory pressure
When a 2.5 ml syringe is used as mouth piece, the values recorded are high. This can be explained by Boyle’s law which tells the inverse relationship between volume and pressure. Smaller the volume of the mouthpiece, greater is the pressure recorded.
The Pearson correlation analysis showed no linear relationship with other sized mouthpieces. While, 10 ml and 20 ml syringe mouthpieces showed positive correlation, better values are obtained with 10 ml syringe mouthpiece [Table/Fig-4,5].
Maximal inspiratory pressure using different sized mouth pieces. X-Axis indicates the various size of the syringe used. Y-Axis indicates the mean of the pressure recorded.
Correlation analysis between mouth pieces of various diameters.
| Age | | Age | MIP | MEP |
|---|
| | 1 | 2.5 ml | 10 ml | 20 ml | 2.5 ml | 10 ml | 20 ml | SMM |
| MIP | 2.5 ml | -.028 | 1 | | | | | | |
| | .884 | | | | | | | |
| 10 ml | -.188 | .701** | 1 | | | | | |
| | .319 | .000 | | | | | | |
| 20 ml | -.008 | .297 | .635** | 1 | | | | |
| | .967 | .111 | .000 | | | | | |
| MEP | 2.5 ml | .144 | .261 | .326 | .023 | 1 | | | |
| | .448 | .163 | .079 | .906 | | | | |
| 10 ml | .094 | .325 | .454* | .178 | .959** | 1 | | |
| | .623 | .080 | .012 | .346 | .000 | | | |
| 20 ml | .134 | .149 | .411* | .170 | .898** | .902** | 1 | |
| | .479 | .433 | .024 | .369 | .000 | .000 | | |
| SMM | -.038 | .128 | .359 | .033 | .724** | .731** | .730** | 1 |
| | .841 | .501 | .052 | .864 | .000 | .000 | .000 | |
**. Pearson’s correlation is positively significant. (Values closer to +1) MIP: Maximum Inspiratory Pressure, MEP: Maximum Expiratory Pressure
SMM: sphygmomanometer
Maximum expiratory pressure
A 2.5 ml syringe mouthpiece showed no correlation. 10ml, 20 ml and sphygmomanometer showed positive linear associations. 10 ml syringe values were closer to 1 [Table/Fig-5,6].
Maximum expiratory pressures recorded with mouth pieces of different size (green bars) and sphygmomanometer (red bar). X- Axis indicates the various size of the syringe used. Y-Axis indicates the mean of the pressure recorded.
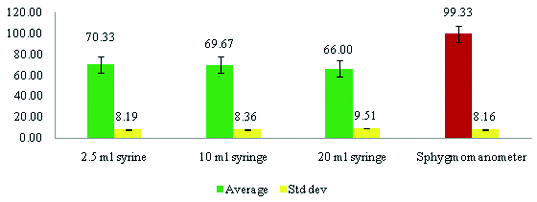
Confidence limit
The confidence limit used in this study in 95%. For maximum inspiratory pressure, the confidence limit for 2.5 ml syringe was 2.34. Similarly for 10 ml was 3.34 and 20 ml were 3.57. For maximum expiratory pressures, the confidence limit for 2.5 ml syringe was 2.93. Similarly for 10 ml was 2.99 and 20 ml were 3.4. For sphygmomanometer it was 2.92.
Discussion
American Thoracic society /European Respiratory Society [13] recommend pressure transducers in connection with various forms of systems like air-filled balloon, liquid filled catheter, and catheter mounted transducer and fiber optic sensors. The reference method for respiratory pressure measurement is intra oesophageal catheter placement and recording [13]. Though these tests are more precise, it requires enormous technical specifications and expert hands to carry out. Moreover, being invasive there is very little chance of performing these tests in average day care settings.
Volitional tests like oral measurement of respiratory pressures gives indirect estimate of respiratory muscle power. With the best of our efforts, the exact cost quotations of intra oesophageal pressure measurement devices could not be made available in exact figures. Approximate price ranges in multiple lacs. Other volitional tests mentioned in ATS/ERS recommendations [13] necessitate pressure transducers of any form. Incidentally the available pressure transducers of varied types gives different results and standard reference range could not be made out. The existing reference range is for Caucasian ethnic population and not for Indian ethnic group. While these transducers are different in their own kind and less available in domestic market, this manometer used in many Indian studies are simple to design, can be replicated universally and costs less than five hundred Indian Rupees.
Mercury manometers and aneroid manometers are easy and cost effective alternatives for transducer based instruments in respiratory pressure assessment. In a book called “Respiratory care equipments” [14], it has been said that U-shaped mercury manometers can be used for static pressure measurement; whereas aneroid and electromechanical transducers can be used for dynamic pressure measurements. Aneroid and vacuum type manometers are not as accurate as mercury manometers [15]. Moreover, it has been mentioned in a study [16] that aneroid gauge manometers have moving parts that become worn out over time and use. Calibrating a mercury manometer to accuracy (keeping the mercury column at 0 levels) can be done by just adding or removing mercury which is simple. Whereas calibrating aneroid or vacuum manometers need expertise. Even vacuum manometers are also calibrated for accuracy against mercury manometers [17].
Respiratory pressures, being a medium pressure measurement and a static pressure, this present study considered mercury manometer as a better tool than other forms of manometer. Though supportive evidence can be quoted [18], more trials with larger sample are warranted.
Safety measurements in this instrument
The tube that gets connected to the mouth piece is quite lengthy which is sufficient enough to prevent mercury to cross its length. This has been ensured with multiple trials with different sized tubing like intra venous fluid administering drip set, endotracheal tubes connected in series. Ryle’s tube only was satisfactorily stood the trial.
The end of the Ryle’s tube is connected to a standard 3 way connector commonly used in hospital settings. The internal diameter is so small that it does not allow volumes of mercury to spill out.
The tip of the glass syringe is smaller than the 3 way connector. Though there happened to be an accidental spill over of mercury beyond 3 way connector, it will be minimized by the even smaller tip of the glass syringe.
If the mercury crosses the syringe tip the flow velocity of mercury will be dampened by suddenly increasing internal diameter of the glass syringe (Boyle’s law).
Since all the recordings are performed in the presence of a trained technician, the procedure can immediately stopped once the mercury touches the top of the Ryle’s tube.
Mercury manometers are being less used for its toxicity reasons. Elemental mercury used in manometers becomes a concern of toxicity only during accidental spillage and during service. Central Pollution Control Board belonging to Government of India [19] has defined norms for safe disposal of mercury. Accidental spillage can be handled safely if such norms were practiced. Moreover, levels of mercury vapor producing toxicity are also much higher [8]. But World Health Organization report on mercury and health, states that exposure to level 20 micrograms/ cubic meter for several years only produces mild subclinical symptoms [8]. United States Environmental Protection Agency [9] in its fact sheet states that toxicity occurs by inhalation for high dose only.
Regarding the design, we have used glass syringes of different dimensions as mouth piece. Mouth piece internal diameter was inversely correlating with recorded pressure. Gopalakrishna A et al., [20] have reported that diameter of the orifice influences the amount of pressure generated. This study finding has a similar observation as of the previous authors. There was a change in recorded pressure and the correlation analysis result showed a significant difference from both above and below 10 ml mouth piece range. This variation was observed in both maximum inspiratory as well as expiratory pressure recordings. Still, the use of precise mouth piece of particular dimension needs further studies with larger subject population.
Limitations
As the toxicity level of elemental mercury in vapour form has not been determined precisely, the use of mercury manometer in measuring inspiratory pressures becomes doubtful. In that case, only expiratory pressures alone can be measured. Since the standard reference method is intra oesophageal balloon catheter recording, validation of this instrument against the reference could not be made out in this present study. The commercially available equipments themselves are not standardized and validated against intra oesophageal balloon catheter recording. This made validation against commercially made instruments difficult and less accurate.
There is a possibility that the compression of Ryle’s tube itself can alter the pressure recording. This study used Ryle’s tube mainly for its universal availability and easy reproducibility of the design.
Conclusion
Standing by the aim of this study, after weighing the importance of measuring respiratory muscle strength and health care economics in low economic regions against the toxicity concern about mercury, this study considers the use of mercury manometers rational in assessing respiratory pressures as long as the norms for mercury disposal is followed. With the imprecise evidences about toxicity levels of mercury and the limitations of this present study, this study is inadequate to make any recommendations on use of mercury based manometers.
Recommendations
More research on biomedical instrumentation is needed to develop standard and cost effective diagnostic tools for measuring respiratory pressures. Aneroid gauge or vacuum gauge manometers could be designed with the correction for inaccuracies.
Further studies and research are needed to standardize the design so that it can be constructed and made safe to be used in various part of the world. Regarding the toxicity levels of mercury vapor, further correlation studies are needed to determine the toxic dose in accordance with duration of exposure.