Periodontics and restorative dentistry are two disciplines of dentistry which share a synergistic bond and are heavily interdependent [1]. Hence having a detailed understanding on this interrelationship not only aids the clinician in delivering optimum aesthetics but also a comforting dentition. The principles of biologic width have been intensively researched and also governed as clinical guidelines for perio-restorative interrelationships [2]. Crown lengthening surgery is performed to correct gingival asymmetries and to reposition the dentogingival complex as an adjunct to perio-aesthetic procedures. Not only does this procedure lead to an increase in clinical crown length, but it also involves a concurrent increase in biologic crown length which is defined as the distance from the incisal edge of the tooth to the crest of the bone [3]. There is a general lack of common opinion concerning the amount of tooth structure that must be exposed coronal to crest of bone for restorative purposes [4–9].
It is a well-known fact that practitioners tend to underestimate the amount of tooth structure that must be exposed during a crown lengthening procedure, leading to biologic width violation. Various subjective methods have been followed in the past, like the use of acrylic templates but these are imprecise and burden the patient with additional cost and multiple visits [10]. Thus an objective measuring device would prove to be a valuable aid in assuring that sufficient tooth structure is exposed, as well as in establishing a clinical crown with ideal width-to-length proportional relationship. Chu aesthetic gauges are a series of innovatively designed, color coded measurement gauges that provide a biologically based, step-by-step approach to periodontal aesthetic crown lengthening. While there have been a few case reports on performing surgical crown lengthening using Chu aesthetic gauges, there are no studies done till date. Hence the purpose of this study was to perform aesthetic crown lengthening using Chu aesthetic gauges and to evaluate the healing of biologic width over a period of six months.
Materials and Methods
A total of 15 systemically healthy patients requiring crown-lengthening in relation to maxillary anterior teeth selected from the outpatient department of JSS Dental College and Hospital, affiliated to JSS University Mysore, Karnataka, took part in this clinical study from March 2013-May 2015.
The purpose of performing crown lengthening surgery in this study was to ensure providing enough tooth structure to facilitate placement of restorative margin such that it does not violate the biologic width and hence restoring not only an aesthetically pleasing smile but also a long lasting restoration.
The inclusion criteria were: Those patients who self reported to the OPD of Department of Periodontology, stating they were unhappy with their present smiles (either due to uneven wear or faulty restorations, or tooth length/width discrepancies or a gummy smile) were taken into the study after taking into account their biologic width requirements (Only those patients in whom placing any restoration subgingivally would lead to biologic width violation) were taken in for crown lengthening surgery after obtaining an informed consent. The other criteria that were taken into account were: Systemically healthy patients within the age group 18-50 years both males and females, patients who after completing the initial phase of periodontal therapy, displayed the ability to maintain good oral hygiene, those who required maxillary anterior crown lengthening surgery to correct disproportionate length to width ratios resulting in unaesthetic smiles.
The exclusion criteria were: Local or systemic contraindications to surgery, unreasonable compromise on adjacent alveolar bone support, mobile teeth, periodontal pockets ≥4mm, unfavourable crown-root ratio.
Study design: A total of 15 patients were selected after the initial completion of phase one periodontal therapy. The investigation was performed in accordance to the requirements of the “Declaration of Helsinki” [11]. The study protocol explained herein was approved by the Institutional Review Board (IRB), JSS Dental College and Hospital, an affiliated institution of the JSS University, Mysore. Patients were given a brief description of the study, and a written informed consent letter was obtained from all the patients. The selected sites were divided into three groups: (1) Treated (TS) sites: Sites on teeth selected for crown-lengthening; (2) Adjacent (AS) sites: Interproximal sites that shared a proximal surface with the treated tooth; (3) Nonadjacent (NAS) sites: Interproximal sites away from the treated tooth.
Clinical parameters: All measurements were standardized using customized acrylic stents with grooves and recorded using a UNC-15 probe (Hu-Friedy) and rounded to the nearest 0.5 mm by a single examiner not related to the study. Calibration exercises were conducted on 10 patients with two sets of readings taken in a two-hour interval by a single examiner. The assessment was made by an independent source, and intraexaminer reproducibility was found to be 90%. The following clinical parameters were recorded at six sites (mesiobuccal, midbuccal, distobuccal and mesiopalatal, mid palatal and distopalatal) around every TS, AS and NAS site at baseline, 3 and 6 months:
Plaque Index (PI)- (Silness and Loe, 1964) [12]
Gingival Index (GI)-(Loe and Silness, 1963) [12]
Position of Gingival Margin (PGM) - Distance from the fixed reference point to the free gingival margin.
Relative Attachment Level (RAL)- Distance from the fixed reference point to the base of the pocket
Bone Sounding (BS)- After the experimental area was anaesthetized, bone level (BL) was obtained via transgingival probing.
Biologic Width (BW)-Bone sounding minus sulcus depth.
Probing Depth (PD)- Relative attachment level minus position of gingival margin.
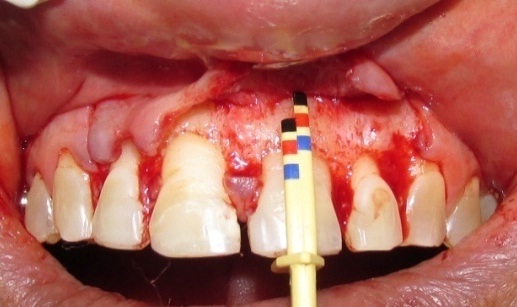
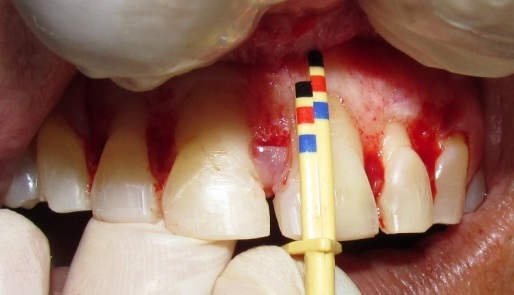
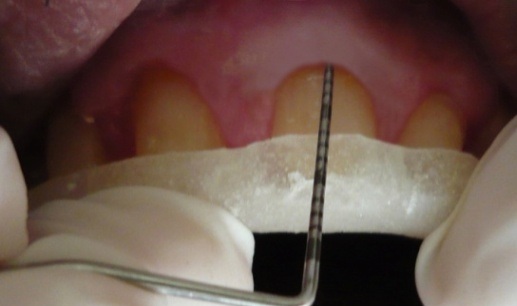
Pre Surgical Protocol: Pre operative photographs were taken of the patient [Table/Fig-1]. Four weeks post phase 1 therapy, patients with good oral hygiene compliance were further prepared for the surgical phase. Prior to any surgical intervention, the final incisal edge position was determined for each patient by diagnostic wax up. The position of gingival margin [Table/Fig-2], sulcus depth [Table/Fig-3] and bone sounding [Table/Fig-4] were recorded at baseline level prior to the surgery.

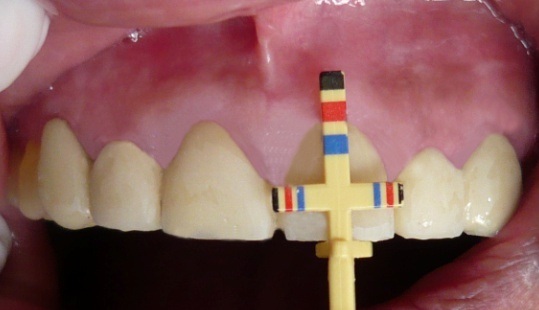
Position of gingival margin – baseline.



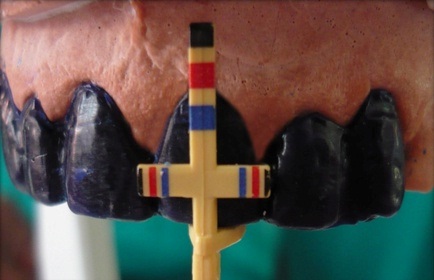
Surgical Protocol: The surgical area was anaesthetized with 2% lignocaine HCL containing 1:80,000 adrenaline solution. Chu aesthetic gauges [13] (Proportion gauge, Crown lengthening gauge, Sounding gauge) (Hu-Friedy Inc, Chicago, IL) were used to perform crown lengthening. First sounding gauge was used to perform bone sounding. After the biologic width was determined, tooth width to length ratio was determined with the Chu proportion gauge [Table\Fig-5]. The incisal stop of the Chu proportion gauge was rested on the incisal edge of the tooth. Each colour coded band on the horizontal arm corresponded to the same colour coded band on the vertical arm. The red band stood for the length and width of the central incisors, yellow for canines and blue for lateral incisors. Depending on individual tooth size variations, it was moved either one band up (for larger teeth) or one band down (for smaller teeth). If the colour coded bands did not coincide with existing tooth proportions, a diagnosis of width to length discrepancy was arrived at. Next, bleeding points were established as guided by the Chu-proportion gauge [Table/Fig-6]. External bevel gingevectomy was then performed to achieve the ideal anatomic crown length [Table/Fig-7,8]. A full thickness flap was reflected, and Chu biologic periogauge was used to achieve the proper midfacial clinical and biologic crown length simultaneously as it had a preset midfacial dentogingival measurement of 3 mm. The colour codes on shorter arm aided in determining the clinical crown length and those on longer arm represented biologic crown length, hence facilitating in determining the exact amount of bone to be resected [Table/Fig-9,10 and 11]. The flaps were then approximated with sutures and a periodontal dressing was placed (Coe-Pak, GC America Inc., Alsip, IL).
Preoperative clinical crown length.



Post operative Ideal clinical crown length.

Pre operative biologic crown level.

Post ostectomy biologic crown length.
Postoperative Care: Routine postoperative instructions were given to the patient. A chlorhexidine mouthwash was prescribed along with systemic antibiotics and analgesics for patient comfort. Patients were then asked to report after one week post surgery for suture removal and a check up. Patients were recalled three months later and clinical parameters were re-recorded [Table/Fig-12,13]. Post diagnostic wax up [Table/Fig-14], crowns were fabricated. The Patients were then followed up for six months with reassessment of clinical parameters [Table/Fig-15,16 and 17]. The permanent restoration of crowns was done after six months of uneventful healing [Table/Fig-18]. The pre and postoperative photographs when compared highlighted the results that were achieved even more [Table/Fig-19,20].
Position of gingival margin– 3 months.

Position of gingival margin- 6 months.


Final restoration- 6 months.


Statistical Analysis
Descriptive statistics were calculated and expressed as mean and standard deviation. Since the data was quantitative in nature, within group comparisons were made using paired t-test. The comparisons were made from baseline to three months, baseline to six months and from three months to six months. All the analysis were performed using SPSS software version 19, 2010 (IBM, USA). A p-value of less than 0.05 was considered to be statistically significant.
Results
Fifteen patients completed this study and no complication related to the surgery or prosthetic treatment was observed.
Plaque and Gingival Index (PI,GI)
The mean values of PI and GI ranged from 1.15 to 1.32 and 1.21 to 1.24 respectively. No significant change was noted in the plaque index or the gingival index at the treated, adjacent and nonadjacent sites at any intervals of time.
Changes in Position of gingival margin for treated site (TS), Adjacent site(AS), and Nonadjacent site (NAS).
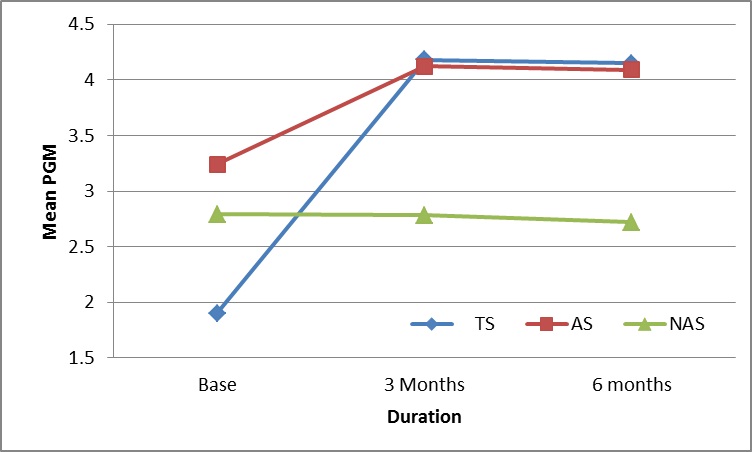
In relation to the mean distances from the reference stent to the gingival margin, at all sites, there was an apical displacement in the position of gingival margin from baseline (1.90±0.017) to three months (4.18±0.05) and six months (4.15±0.05) p=0.001, which was statistically significant. The PGM at the TS sites was more apical when compared to that at the AS and NAS sites at six months. However, the difference in position of gingival margin from three months to 6 months was statistically non significant.
Changes in Biologic Width for treated site (TS), Adjacent site (AS), and Nonadjacent site (NAS).
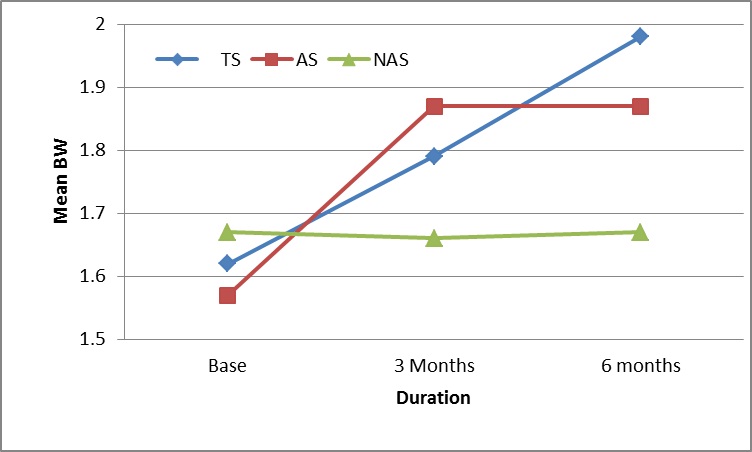
The mean biologic width at the treated site, from baseline i.e., (1.63±0.02) increased (1.79 ±0.01) at three months and further increased to the mean of 1.99±0.01 at six months. The difference at all 3 intervals i.e., baseline to three months, three months to 6 months and baseline to six months was statistically significant (p=0.001). At the adjacent site, the baseline biologic width i.e., 1.57±0.02 increased to 1.87±0.016 at three months and then increased to the mean of 1.87±0.01 at six months. The difference in from baseline to three months and to six months was statistically significant (p=0.001), however the difference from three months to six months was statistically non significant. At the non adjacent sites, the difference of biologic width measurements at all three intervals i.e., baseline to 3 months, 3 months to 6 months and baseline to six months was statistically non significant.
Discussion
Preservation of a healthy periodontium is critical for the long-term success of a restored tooth [14]. It is a well-known fact that practitioners tend to underestimate the amount of tooth structure that must be exposed during a crown lengthening procedure, leading to biologic width violation. It therefore becomes more prudent to increase adequate dimension of clinical crown through crown lengthening rather than risk a violation of the biologic width & thereby harm the periodontium.
There is a lack of consensus regarding the amount of tooth structure that must be exposed coronal to the crest of bone for re-storative purposes. At most occasions a minimum distance of 3 mm from the osseous crest to the final restorative margin following a crown-lengthening procedure is accepted as optimum [15–21]. This 3 mm encompasses 1 mm of supracrestal connective tissue attachment, 1 mm of junctional epithelium and 1 mm for sulcus depth [21]. The amount of bone reduction in this study was guided by the crown lengthening gauge which had a preset colour coded markings at 3 mm hence ensuring 3mm osseous reduction from the clinical crown.
The results of this study showed that in relation to the position of the gingival margin, there was a significant apical displacement in the position of gingival margin at three and six months when compared from baseline in the treated and adjacent sites. Also, there was a greater percentage of apical shift in the free gingival margin position at the treated sites from baseline when compared with adjacent and nonadjacent sites at six months. Similar finding has been reported in the studies by Lanning et al and Shobha et al., [14,22]. Contrary to the findings of this study, Bragger et al., Pontoriero et al., and and Ritika Arora et al., observed, a significant amount of rebound in the position of the gingival margin [23–25]. These authors attribute this rebound to the lesser amount of bone reduction and placement of flaps at the osseous crest after suturing to have been the major influences on the rebound that was observed. Also, the reason for these opposite patterns of marginal tissue alteration after surgical crown lengthening may have been due to differences in the interpretation and/or execution of the surgical technique. The stability of the biologic width and the position of the gingival margin achieved in this study could be attributed to the Chu aesthetic gauges which provided a guide to determine precisely how much bone should be removed from a biologic standpoint to ultimately produce a restoration which would be compatible with the periodontium.
The results of our study showed that at all sites, there was an increase in the biologic width dimension from baseline to three months and from baseline to six months. However only in the treated and the adjacent site, this difference attained statistical significance. The changes in the treated and adjacent sites could be attributed to the osseous reduction which was done keeping in mind the positive architecture also it is supported by a study done by Wilderman that histologic bone remodeling can continue for over a year [26]. At the end of six months, the biologic width was reestablished to a more apical region than its original vertical dimension. This could be attributed to the slight gain in the attachment level and apical displacement of the bone level. These finding are similar to a study done by Shobha et al., [14]. However contrary to the findings of our results, Lanning et al., found that the biologic width at all sites was smaller at three and six months except for treated sites which were not significantly different from the baseline at six months [22]. The authors attributed their findings to the surgical technique wherein the amount of bone resected was arbitrarily based on the intended prosthetic margin and the original biologic width. One factor that could have influenced our results was that, bone sounding which is accurately measured after flap reflection, was taken as a closed measurement in our study however it has been shown in previous studies that there is no significant difference between these two modes of measurements [27].
There still remains a controversy as to which time would be ideal for restoration of the tooth which has undergone crown lengthening surgery. Many schools of thoughts prevail in this matter. Three studies provided data regarding periodontal tissue remodeling after surgery. Pontoriero et al., were of the opinion that whenever a restoration is planned in aesthetic important areas [24], a close monitoring of the different degree of tissue regrowth which occurs during healing among patients, should be recommended to determine the achieved gingival margin stability and therefore to assess the ideal time for the definitive restorative purposes. Also, a similar view was stated by Fletcher that while the osseous remodeling may continue for longer than 12 months [3], soft tissue healing is mostly completed by eight weeks. Thus, if the gingival contour has stabilized and crown margins are placed atraumatically intracrevicularly, the definitive restorations can be placed successfully within 8-12 weeks post crown lengthening. Lanning et al., and Shobha et al., suggested that a time period of at least six months is needed for the re-establishment of the biologic width after surgical crown lengthening [14,22]. This timeframe was confirmed by two additional publications Herrero et al., and Bragger et al., [23,28]. The results of our present study also support this view that although the positional changes of the gingival margin, probing depth and attachment levels were stabilized by 3 months, it takes a minimum of six months for the biologic width to re-establish itself.
Conclusion
The purpose of this study was to perform surgical crown lengthening using Chu aesthetic gauges and to evaluate the healing of biologic width over a period of six months. Within the limitations of our study the findings suggests that although the positional changes of the periodontal tissues stabilize by three months, the biologic width if adequate crown lengthening is carried out, reestablishes itself by three months to the original vertical levels and further gets stabilized by six months. The clinical relevance of this study lies in a step by step approach to periodontal aesthetic crown lengthening, which was undertaken using an innovative aesthetic measuring gauge, the Chu aesthetic gauge, which not only determined the ideal crown length of a tooth but also enabled as with a visual precision which was distinct from the conventional guessing or emotional estimations in crown lengthening which is vital for successful, predictable, and aesthetic restorative outcome. However, further studies with larger sample size and long term follow-up are needed to validate the findings of our study.