Trends of Various Techniques of Tubectomy: A Five Year Study in a Tertiary Institute
Kavita Mahadevappa1, Naveen Prasanna2, Ramalingappa Antartani Channabasappa3
1 Assistant Professor, Department of Obstetrics and Gynaecology, Karnataka Institute of Medical Science (KIMS), Hubli, Karnataka, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, Karnataka Institute of Medical Science (KIMS), Hubli, Karnataka, India.
3 Professor and Head, Department of Obstetrics and Gynaecology, Karnataka Institute of Medical Science (KIMS), Hubli, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kavita Mahadevappa, Flat No-DAISY S-3, Aakruti Gardens Apartment, Bhavaninagar, Hubli-580023, Karnataka, India.
E-mail: kavipgi10@gmail.com
Introduction
Female sterilization is one of the best and effective methods of contraception for women who have completed their family. Tubectomy during caesarean operation and minilaparotomy are popular methods in developing countries whereas laparoscopic sterilization and hysteroscopic tubal occlusion are the preferred methods in developed countries.
Aim
To know the trends, incidence and immediate complications of methods of female sterilizations performed at our institute.
Materials and Methods
This is a retrospective analytical study conducted at our tertiary care centre from January 2010 to December 2014 in Karnataka Institute of Medical Sciences, Hubli, Karnataka. The case files of all the patients who underwent sterilization were taken from the medical records section and reviewed in detail. The cases were grouped as caesarean tubectomy, minilaparotomy and laparoscopic sterilization, based on the abdominal entry. For minilaparotomy and during caesarean tubectomy, modified pomeroy’s technique was used. For laparoscopic sterilization, falope rings were used. Data was analysed by Karl Pearson’s correlation co-efficient method and Chi-Square test. The p-value < 0.05 was considered significant.
Results
Out of 5442 cases of female sterilization, 2872 underwent caesarean tubectomy, remaining half underwent minilaparotomy (1306) and laparoscopic sterilization (1264). Sterilizations were significantly more during puerperal period (caesarean tubectomy + post abortal + postpartum) compared to interval period. There was an increasing trend in caesarean tubectomy and laparoscopic sterilization.
There were 11 procedure related complications in the laparoscopic sterilization, one in caesarean tubectomy and none in minilaparotomy. Two deaths were reported in minilaparotomy, one in laparoscopic sterilization and four in the caesarean tubectomy, which were due to septicaemia.
Conclusion
An increasing trend in caesarean tubectomy and laparoscopic sterilization is seen in this study. Female sterilization should be individualized based on the timing, place and surgeons experience. Sepsis is a major cause of death and asepsis could be compromised when female sterilization is done in large numbers in camps. Hence target related approach towards female sterilization should be avoided. Laparoscopic sterilization has more procedure related complications, which can be better handled in tertiary care centres.
Caesarean tubectomy, Laparoscopic sterilization, Minilaparotomy, Postpartum
Introduction
Female sterilization is one of the best and effective methods for women who have completed their family. In Asia, female sterilization rose from 34% in 1980-1984 to 42-43% in 1985-2005 [1]. In contrast the share of female sterilization remained fairly level at 5-8% in Sub Saharan, Africa and the developed countries. In India according to National Family Health Survey (2005-06), 37% of currently married women in the age group 15-49 years were sterilized which accounted for 66% of all the contraception use, making it a leading method of contraception [2]. In the US, second leading method of contraception was female sterilization, used by 10.3 million women. Female sterilization is the leading method among women 35 years and older [3].
Female sterilization can be carried out, at any of the following time, postpartum sterilization – done within seven days of delivery, caesarean tubal ligation – the 2 procedures are combined, interval ligation done six weeks after delivery, postabortal ligation -immediately after evacuation of uterus after induced or incomplete abortion, gynaecological ligation-combined with gynaecological surgeries such as myomectomy, cystectomy or fothergill’s operation. Female sterilization may be performed in several ways such as minilaparotomy, laparoscopic sterilization and hysteroscopic methods. In India, postpartum sterilization is usually done by minilaparotomy, whereas interval and postabortal are usually done by laparoscopy. Tubal ligation done by minilaparotomy is a simple procedure, but requires large incision and is associated with more wound infections, postoperative pain and longer hospitalization, whereas laparoscopic sterilization needs smaller incisions, shorter hospital stays, but needs well trained gynaecologists with expensive, high maintenance equipment [4]. The rates of major complications, death, and technical failure are acceptably low for minilaparotomy and laparoscopic sterilization [5]. In both procedures, most major complications are related to general anaesthesia and abdominal entry. Caesarean tubal ligation, where two procedures are combined, has an advantage of avoiding additional incision, anaesthesia, financial burden and reduces hospital stay.
In developed countries laparoscopy and hysteroscopic are the preferred methods, but in developing countries minilaparotomy and caesarean tubal ligation are still the preferred methods. The World Health Organisation’s (WHO) Task Force on Female Sterilization stated: The ideal female sterilization would involve a simple, easily learned, one-time procedure that could be accomplished under local anaesthesia and involve a tubal occlusion technique that caused minimum damage. The sterilization procedure should not only be safe and readily accessible but also have high efficacy rate, cost-effective, be culturally and personally acceptable. The task force concluded that both laparoscopy and minilaparotomy were close to meeting the required criteria listed above according to the data of a large multicentre prospective study [6]. We intend to find out the trends of various methods of female sterilization and its immediate complications in our institute, so that we can plan and improvise on the contraceptive care.
The present study was done to know the trends, incidence and immediate complications of methods of female sterilizations performed at our institute.
Materials and Methods
This is a retrospective analytical study conducted at our tertiary care centre from January 2010 to December 2014, in Karnataka Institute of Medical Sciences, Hubli, Karnataka. The case files of all the patients who underwent sterilization were taken from the medical records section and reviewed in detail. The cases were grouped as caesarean tubectomy, minilaparotomy and laparoscopic sterilization, based on the abdominal entry. The patients who underwent the procedure within 7 days of vaginal delivery were taken as postpartum sterilization. The patients who underwent the procedure within 7 days of abortion were taken as postabortal sterilization. For minilaparotomy and during caesarean tubectomy, modified pomeroy’s technique was used. For laparoscopic sterilization, falope rings were used. Patients who underwent the procedure 6 weeks after delivery were taken as interval sterilization.
Statistical Analysis
Data analysis was done using Karl Pearson’s correlation coefficient method to find out the p-value, to know the statistical significance of increase or decrease in the various types of sterilization methods over a period of 5 years. Chi-square test was used to compare cases undergoing minilaparotomy and laparoscopic sterilization based on timing of sterilization. Chi-square test was also used to compare the complications in the different methods of sterilizations. The p-value < 0.05 was considered as significant.
Results
In our study, a total of 5442 patients had undergone sterilization procedure. Following were the results observed and they were tabulated. [Table/Fig-1] shows the age distribution of patients. Maximum number of patients 4241(77.93%) underwent sterilization between the age group of 20-29 years. [Table/Fig-2] shows the year wise distribution of sterilization cases based on abdominal entry. In the year 2010, 52.3% of patients underwent caesarean tubectomy. In 2011 the number of patients undergoing caesarean tubectomy reduced to 49.6% and then gradually increased in the subsequent years to reach 58% in 2014. Minilaparotomy cases have reduced from 33.3% in 2010 to the minimum of 13.7% in the year 2014. The number of laparoscopic sterilization cases was 14.4% in 2010 and it has subsequently increased to a maximum of 28.4% in 2014. This trend of sterilization is shown in [Table/Fig-3].
Age wise distribution of patients undergoing sterilization
| Age Years | No of cases | % |
|---|
| 20 – 29 y | 4241 | 77.93 |
| 30 - 39 y | 1178 | 21.65 |
| ≥40 y | 23 | 0.42 |
| Total | 5442 | 100.00 |
Total number of patients who underwent sterilization by different methods
| Year | Caesarean Tubectomy | % | Minilap | % | Lap | % | Total | % |
|---|
| 2010 | 413 | 52.3 | 263 | 33.3 | 114 | 14.4 | 790 | 14.52 |
| 2011 | 489 | 49.6 | 350 | 35.5 | 146 | 14.8 | 985 | 18.10 |
| 2012 | 576 | 50.0 | 310 | 26.9 | 267 | 23.2 | 1153 | 21.19 |
| 2013 | 640 | 52.8 | 205 | 16.9 | 368 | 30.3 | 1213 | 22.29 |
| 2014 | 754 | 58.0 | 178 | 13.7 | 369 | 28.4 | 1301 | 23.91 |
| Total | 2872 | 52.8 | 1306 | 24.0 | 1264 | 23.2 | 5442 | 100.00 |
Trends of female sterilization over 5 years (2010 to 2014)
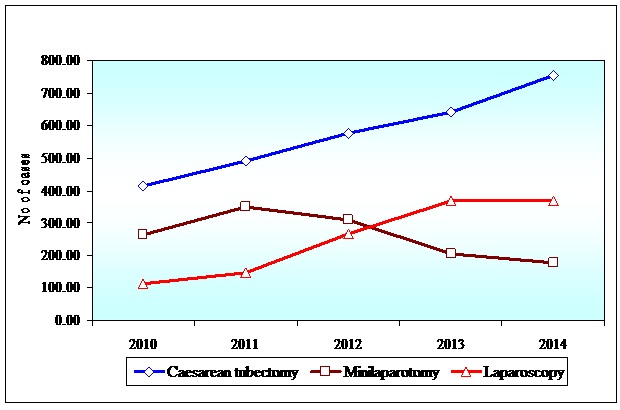
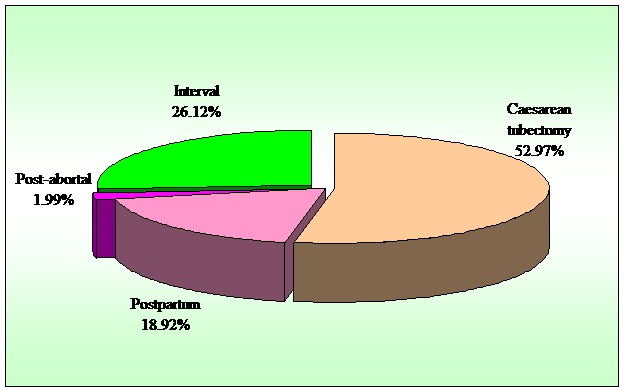
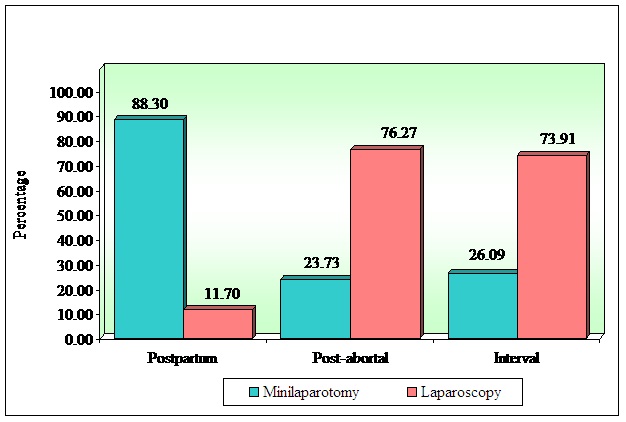
Out of 5442 cases of sterilization, 2872 (52.8%) underwent caesarean tubectomy, remaining half underwent minilaparotomy 1306 (24%) and laparoscopic sterilization 1264 (23.2%). The increase in the number of patients opting for laparoscopic sterilization and caesarean tubectomy, seen over the study period was statistically significant as shown in the [Table/Fig-4]. Though there is a decrease in the number of patients undergoing minilaparotomy, the decrease is not statistically significant. [Table/Fig-5], shows distribution of patients based on timing of sterilization. A total of 2872 (52.8%) underwent sterilization during caesarean operation, 1026 (18.92%) underwent sterilization in the postpartum period, 108 (1.99%) underwent sterilization in the post-abortal period and the remaining 1416 (26.12%) patients underwent interval sterilization. Hence patients opting for sterilization were significantly more during puerperal period (caesarean tubectomy + post-abortal + postpartum) when compared to interval sterilization (74.88% vs 26.12%). [Table/Fig-6] compares the method of abdominal entry opted at different timings of sterilization. Minilaparotomy cases were more in postpartum period, whereas laparoscopic sterilization was the preferred method in postabortal and interval period. As shown in [Table/Fig-7], this difference was statistically significant (p<0.00001). [Table/Fig-8] shows the complications that were encountered in all the methods of sterilization. The procedure related complications were surgical emphysema (5), mesosalpinx tear (5) and trocar injury to uterine fundus (1) in the laparoscopic sterilization, one case of mesosalpinx haematoma in the caesarean tubectomy and none in minilaparotomy sterilization. This difference was statistically significant (p=0.00001). Wound infections were more in minilaparotomy and caesarean tubectomy compared to laparoscopic sterilization. One patient of minilaparotomy and one patient of laparoscopic sterilization had developed peritonitis postoperatively, was subsequently managed with laparotomy with drainage of pus and peritoneal lavage. Two deaths were reported in minilaparotomy, one in laparoscopic sterilization and four in the caesarean tubectomy, which were due to septicaemia.
Discussion
Female sterilization is the most requested contraceptive method worldwide and one of the most frequently performed elective, intra-abdominal surgical procedure performed in reproductive-age women. The technique, timing and setting of the operation have progressively changed since the early 1970’s and the advent of minimally invasive surgery. The most appropriate method of female sterilization in a particular family is often determined by local situations and constraints. According to Cochrane review, the decision which method to choose should be a multifactorial one, depending on the setting, the surgeons experience and the woman’s preference [6]. Laparoscopy is a preferred method in many developed country settings. FIGO 2010 recommends avoiding female sterilization during caesarean operations [7]. However, caesarean tubectomy is one of the preferred method of sterilization in developing countries. In developing countries, age at marriage and childbearing, is earlier than in developed countries. After completion of family at an early age, women look forward for a permanent contraception, rather than temporary methods of contraception which need repeated followup and care. In our study, out of 5442 patients, 58.2% opted for caesarean tubectomy, and there is an increasing trend towards caesarean tubectomy over the 5 years. All the caesarean operations in this study were done for obstetric indications. All the patients undergoing caesarean tubectomy had more than two living children and hence might have opted for caesarean tubectomy to prevent repeated hospitalization and financial burden. Swende TZ et al., conducted a study in Nigeria, where sterilization was done along with caesarean operation in a majority of the patients {37 (47.4%)}, representing 2.7% of all acceptors of family planning methods. Contraceptive effectiveness was 100%. No complication specific to tubal ligation was noticed. It was found to be safe and effective [8]. In another study conducted in Brazil, more than 70% of female sterilizations were combined with a caesarean operations [9].
In our study patients who adopted minilaparotomy were 1306 and laparoscopic sterilization with falope rings were 1264. Minilaparotomy cases have reduced from 33.3% in 2010 to the minimum of 13.7% in the year 2014. The number of laparoscopic sterilization cases was 14.4% in 2010 and it has subsequently increased to a maximum of 28.4% in 2014. There is an increasing trend towards the acceptance of laparoscopic sterilization in our study. In this study, 1426 patients underwent interval sterilization, out of which 372 underwent minilaparotomy and 1054 underwent laparoscopic sterilization. Out of 118 patients, who underwent postabortal sterilization, 28 were minilaparotomy and 90 were laparoscopic sterilizations. This clearly shows the preference of laparoscopic sterilization over minilaparotomy as a method of sterilization during postabortal and interval periods. Whereas out of 1026 patients who underwent postpartum sterilization, 906 were minilaparotomy and 120 was laparoscopic sterilization. This result shows preference of minilaparotomy over laparoscopic sterilization during puerperal period. This is statistically significant. The size of the uterus and the oedematous tubes in the puerperal period make laparoscopic sterilization technically difficult, at the same time this is an advantage for performing minilaparotomy easily. All the surgeons in our institute are trained for performing laparoscopic sterilization and minilaparotomy, but may have been comfortable in performing minilaparotomy in the puerperal period for the above reasons
Correlation between years and number of three types of sterilization cases.
| Sterilization Methods | r-value | t-value | p-value |
|---|
| Caesarean Tubectomy (2871) | 0.9963 | 20.0796 | 0.0003* |
| Minilap (1306) | -0.6983 | -1.6895 | 0.1897 |
| Lap (1264) | 0.9641 | 6.2889 | 0.0081* |
*p<0.05 (Karl Pearson’s correlation coefficient method was used to see the relationship between two quantitative variables)
Distribution of patients by timings of tubectomy
Distribution of patients by timings of sterilization in Minilaparotomy and Laparoscopic sterilization.
| Timings | Mini-laparotomy | % | Laparo-scopy | % | Total | % |
|---|
| Postpartum | 906 | 88.30 | 120 | 11.70 | 1026 | 39.92 |
| Post-abortal | 28 | 23.73 | 90 | 76.27 | 118 | 4.59 |
| Interval | 372 | 26.09 | 1054 | 73.91 | 1426 | 55.49 |
| Total | 1306 | 50.82 | 1264 | 49.18 | 2570 | 100.00 |
*p<0.05
Chi-square=960.4621 p = 0.00001*
Distribution of patients by timings of tubectomy in Minilaparotomy and Laparoscopy method.
Complications of Sterilization
| Complications | Minilap (1306) | Lap (1264) | Caesarean Tubectomy (2872) | Differences Among the Procedures |
|---|
| Chi-Square | p-value |
|---|
| Procedure Related Complications | 0 | 11 | 1 | 31.6401 | p=0.0001* |
| Wound Infection | 18 | 1 | 15 | 18.4902 | p=0.0001* |
| Peritonitis | 1 | 1 | 0 | 2.2371 | p=0.3273 |
| Death | 2 | 1 | 4 | 0.3286 | p=0.8494 |
*p<0.05
According to Cochrane review, major morbidity seems to be a rare outcome for laparoscopy and minilaparotomy [6]. There were 11 procedure related complications in the laparoscopic sterilization. There was one case of trocar injury to uterine fundus, which was repaired by laparotomy. There was 5 cases of mesosalpinx tears, out of which 4 underwent laparotomy to control bleeding and one mesosalpinx bleeding was controlled with bipolar cautery. Surgical emphysema was seen in 5 patients who were all managed conservatively. There was only one procedure related complication in patients, who underwent caesarean tubectomy. That patient developed a haematoma in the mesosalpinx (which had tortuous, engorged vessels) which was evacuated and bleeding vessels ligated. Hence in our study the procedure related complications were more in laparoscopic sterilization, which was statistically significant. Michael Klarke et al., showed 1.4% of patients developed mesoslpinx tear during laparoscopic sterilization and required laparotomy to control bleeding from mesosalpinx tear [10].
Mumford SD et al., in their study compared minilaparotomy and laparoscopic tubectomy for tubal sterilization from 23 countries. Number of cases who underwent laparoscopy with occlusion by the tubal ring was 7053, and minilaparotomy with occlusion by the modified Pomeroy technique was 5081 cases. The failure rate was 0.60% for laparoscopy and 0.30 per 100 women for minilaparotomy. In minilaparotomy, the surgical complication rate (0.79%) is less when compared to laparoscopic sterilization (2.04%), whereas the technical failure rate was double that laparoscopic sterilization. The preference for minilaparotomy over laparoscopy procedure was noted in this study [11].
Infections were the major issue noted in all the three methods of sterilization. There were 7 deaths in our study and all the patients died because of septicaemia. Kulier R et al., reviewed 15 RCT’s of techniques for tubal sterilization, involving 13,209 women of childbearing age, where no deaths reported with any method, and major and minor morbidity were rare [12]. Two weeks after interval sterilization at a camp in the central Indian state of Chhattisgarh, 13 women died. The postmortem examinations of seven of the women indicated towards septicaemia, which can result from poor hygiene during surgery [13]. Strauss LT et al., conducted a global mail survey of 4642 physicians, and received responses from 1298 physicians (28%) in 80 countries. Fifty-five sterilization-associated deaths had occurred from January 1, 1980 to June 30, 1982. Infection, anesthetic complications, and hemorrhage were the most frequently reported causes of death [14].
Our study shows that puerperal sterilization was preferred by the patients in our centre. Caesarean tubectomy is a safe and popular method in our center, with more than half of the patients opting for it. Caesarean tubectomy can be offered for patients who undergo caesarean operation for obstetric indications and who are looking for permanent method of sterilization. If not offered during the puerperal period, women may land up in unwanted pregnancies with a scarred uterus which could be difficult to manage and could pose danger to her life. Women are more receptive towards contraception during puerperal period, hence more assistance and counseling for contraceptive methods can be offered during this period. In our study Laparoscopic sterilization is the preferred method in the interval period.
Conclusion
An increasing trend in caesarean tubectomy and laparoscopic sterilization is seen in our study. Female sterilization should be individualized based on the timing, place and surgeons experience. Sepsis is a major cause of death and asepsis could be compromised when female sterilization is done in large numbers in camps. Hence target related approach towards female sterilization should be avoided. Laparoscopic sterilization has more procedure related complications, which can be better handled in tertiary care centres.
*p<0.05 (Karl Pearson’s correlation coefficient method was used to see the relationship between two quantitative variables)
*p<0.05
Chi-square=960.4621 p = 0.00001*
*p<0.05
[1]. Jain R, Muralidhar S, Contraceptive methods: needs, options and utilizationJ Obstet Gynecol India 2012 61:626-34.doi: 10.1007/s13224-011-0107-7. [PMC free article] [PubMed] [Google Scholar]
[2]. International Institute for Population Sciences (IIPS) and Macro International. 2007National Family Health Survey (NFHS-3) 2005–06 Volume IIndiaMumbai: IIPS [Google Scholar]
[3]. Mosher WD, Martinez GM, Chandra A, Abma JC, Willson SJ. Use of Contraception and use of Family Planning Services in the United States: 1982–2002, Division of Vital Statistics) Advance Data No. 350 + December 10, 2004 (2002 National Surveys of Family Growth (NSFG) [Google Scholar]
[4]. Layde PM, nPeterson HB, Dicker RC, Destefano F, Rubin GL, Ory HW, Risk factors for complications of interval tubal sterilization by laparotomyObstet Gynecol 1983 62:180-4. [Google Scholar]
[5]. Kulier R, Boulvain M, Walker D, Candolle G, Campana A, Minilaparotomy and endoscopic techniques for tubal sterilizationCochrane Database Syst Rev 2004 (3):CD001328 [Google Scholar]
[6]. World Health Organization, Task Force on Female Sterilization, Special programme of Research, Development and Research Training in Human ReproductionMinilaparotomy or laparoscopy for sterilizationAm J Obstet Gynecol 1982 143:645-52. [Google Scholar]
[7]. Dickens B, Female contraceptive sterilisation: International Federation of Gynecology and Obstetrics (FIGO) Committee for the Ethical Aspects of Human Reproduction and Women’s HealthInt J Gynaecol Obstet 2011 115:88-9. [Google Scholar]
[8]. Swende TZ, Hwande TS, Female sterilization by tubal ligation at caesarean section in Makurdi, NigeriaAnn Afr Med 2010 9(4):246-50.doi: 10.4103/1596-3519.70965 [Google Scholar]
[9]. Soares LC, Brollo JLA, Family planning in Brazil: why not tubal sterilisation during childbirth?J Med Ethics 2013 39:710-12.[PubMed] [Google Scholar]
[10]. Klaerke M, Nielsen JEB, Vilsgaard K, Laparoscopic Sterilization with the Falope-Ring Technique in the PuerperiumActa Obstetricia et Gynecologica Scandinavica 1986 65:99-101.doi: 10.3109/00016348609158361 [Google Scholar]
[11]. Mumford SD, Bhiwandiwala PP, Chi IC, Laparoscopic and minilaparotomy female sterilization compared in 15167 casesLancet 1980 2(8203):1066-70. [Google Scholar]
[12]. Lawrie TA, Kulier R, Nardin J, Techniques for the interruption of tubal patency for female sterilizationCochrane Database of Systematic Reviews 2015 9:CD003034DOI: 10.1002/14651858 .CD003034.pub3 [Google Scholar]
[13]. Pulla P, Why are women dying in India’s sterilisation camps?BMJ 2014 :349doi: http://dx.doi.org/10.1136/bmj.g7509 (Published 08 December 2014) [Google Scholar]
[14]. Strauss LT, Huezo CM, Kramer DG, Rochat RW, Senanayake P, Rubin GL, Sterilization-associated deaths: a global surveyInt J Gynaecol Obstet 1984 22(1):67-75. [Google Scholar]