Spontaneous Subdural Haemorrhage: A Rare Association with Plasmodium Vivax Malaria
Ajay Raj Mallela1, Shetty Hariprasad2, Rohini Koya3, Vasudev Acharya4, Shastry Barkur Anantha Krishna5
1 Junior Resident, Department of Internal Medicine, Kasturba Medical College, Manipal, India.
2 Assistant Professor, Department of Internal Medicine, Kasturba Medical College, Manipal, India.
3 Junior Resident, Department of Internal Medicine, Kasturba Medical College, Manipal, India.
4 Professor, Department of Internal Medicine, Kasturba Medical College, Manipal, India.
5 Professor, Department of Internal Medicine, Kasturba Medical College, Manipal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajay Raj Mallela, Junior Resident, Department of Medicine, Kasturba Medical College, Manipal, Udupi-576104, Karnataka, India.
E-mail: ajayprakashdr@gmail.com
Malaria is an endemic disease in tropical countries and disease of universal importance. Central Nervous System (CNS) complications of malaria are severe and associated with significant mortality. Thrombocytopaenia in malaria causing haemorrhagic CNS complications is rare. We report a case of 35-year-old male patient presented with headache, vomiting and was diagnosed to have subdural haemorrhage (SDH). On examination patient was found to be febrile with peripheral smear showing evidence of Plasmodium vivax (P.vivax) infection with severe thrombocytopaenia. In endemic regions with malaria, SDH being rare presentation of malaria should be considered as a differential diagnosis in febrile patients with neurological manifestations. Rarity of spontaneous SDH in malaria and raising awareness amongst treating physicians about the same is the driving factor for reporting this case.
Cerebral malaria, Falciparum, Thrombocytopaenia
Case Report
A 35-year-old man presented with sudden onset of headache and vomiting since five days. On examination patient had jaundice and was haemodynamically stable. CNS examination showed Glasgow Coma Scale (GCS) of 12(E3V4M5), pupils were bilaterally equal and reacting to light, extraocular movements were normal with no facial asymmetry. Motor and sensory system examination was grossly normal. Deep tendon reflexes were normal with bilateral plantar response being flexor. Fundus examination was normal. Other system examination was unremarkable.
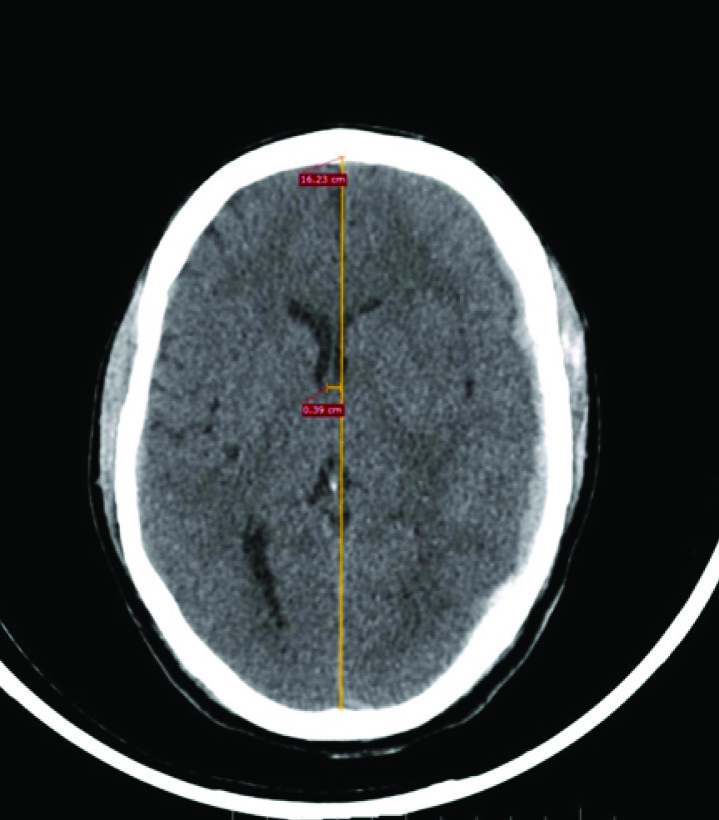
So immediate Computed Tomography (CT) of brain was obtained which showed subdural haemorrhage along left frontal, parietal and temporal convexities with midline shift and mass effect [Table/Fig-1]. Patient developed high grade fever (102o F) with worsening of sensorium.
Plain CT brain axial section showing subdural haemorrhage along left frontal, parietal and temporal convexities with midline shift and mass effect.
Laboratory investigations including complete blood picture showed anaemia (haemoglobin of 9.1gm/dl) thrombocytopaenia (platelet count of 13 x 103/microlitre), peripheral smear examination showed schizonts and ring forms of P.vivax. Biochemical investigations showed evidence of haemolysis with total bilirubin of 6.7gm/dl (range-0.2 to1.2mg/dl) with unconjugated fraction being 5.9gm/dl with no liver enzyme elevation. Renal function tests, serum electrolytes and coagulation parameters were within normal limits. As per WHO guidelines he was started on intravenous artesunate (2.4mg/kg), followed by same dose after 12 hours and was then continued once daily for five days. Doxycycline 100mg twice daily dosing for duration of one week was given along with artesunate. Antioedema measures were started with intravenous mannitol (0.5g/kg) every 8th hourly.
Neurosurgery opinion was sought regarding SDH and was advised conservative management. Patient was given five units of random platelet transfusion (single donor platelets).
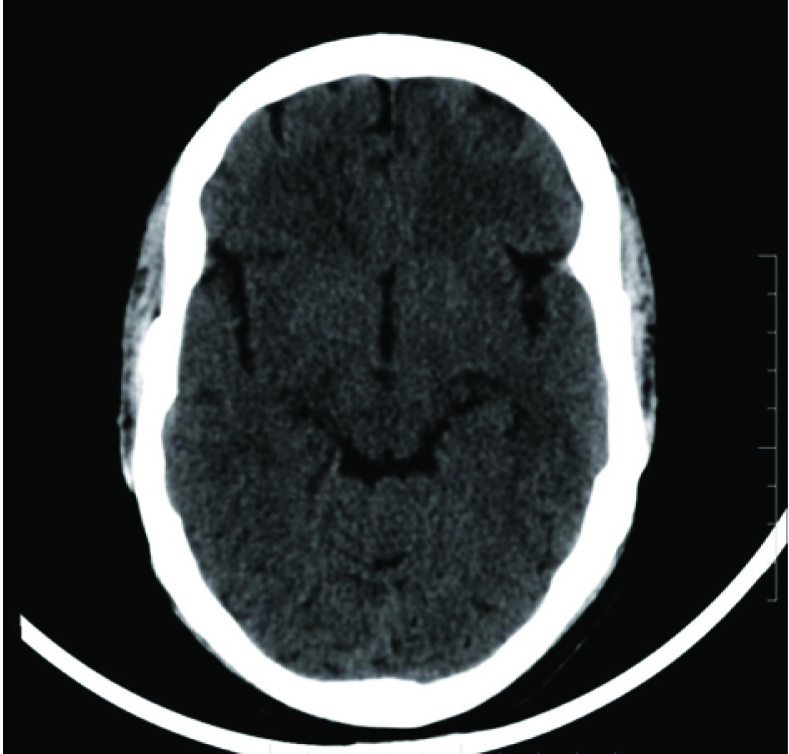
Following therapy, patient became afebrile with rapid and significant neurological improvement. His repeat platelet count (50 x 103/microliter) and biochemical parameters improved. Patient was discharged on primaquine (30mg daily for two weeks). The follow up CT showed resolved subdural haematoma [Table/Fig-2].
Plain CT brain axial section showing completely resolved subdural haemorrhage.
Discussion
Cerebral malaria is considered as severe complication associated with CNS manifestations like convulsions, hemiplegia, delirium, coma and death [1]. Subdural Haemorrhage (SDH) as a complication following Plasmodium falciparum (P.falciparum) infection has been reported in literature [2,3]; however incidence of SDH following Plasmodium vivax (P.vivax) infection is rare, as per our knowledge only one case with isolated plasmodium vivax infection has been reported [4].
Malaria is considered as a great public health problem in tropical countries. Malaria affects all components of blood, usually presents as anaemia and thrombocytopaenia. Most common haematological abnormality of malaria is thrombocytopaenia. Initially it was thought that thrombocytopaenia is a feature of P. Falciparum, later several studies relating P.vivax with severe thrombocytopaenia were published in late 1990s. Precise mechanism of thrombocytopaenia is unknown; however immune mechanisms, oxidative stress, splenic sequestration and parasite interaction with platelets were suspected [5]. Thrombocytopaenia is not included in list of severity criteria for malaria as it is unable to cause mortality by itself [6]. Wang HS et al., reported that acute spontaneous SDH is rare pathological entity without traumatic aetiology and accounts for less than 5% of cases [7]. Several reports of SDH in young individuals, who had risk factors such as hypertension, solid tumour dural metastasis, vascular malformations and alcoholism were reported [8]. SDH is also associated with conditions which cause sudden increase in intravenous pressure (lifting weights, trumpet blowing, defecation, coughing) [9]. In our patient the above mentioned risk factors were absent however SDH could be due to severe thrombocytopaenia associated with malaria.
Aetiology of SDH may be due to sequestration of parasitized red blood cells causing rupture of small vessels in association with severe thrombocytopaenia [3]. Grau GE et al., showed association of rise in serum TNF-alpha with the process of haematoma formation as its concentrations correlate with disease severity [10]. TNF-alpha may contribute sequestration of platelets and red cells in the cerebral circulation thus leading to haemorrhage [11]. According to WHO protocol patient was treated on basis of complicated malaria [12].
Till date; there is no strong evidence in literature regarding management of thrombocytopaenia in malaria. Platelet transfusions are usually given, without evidence of benefits. Though headache is a non-specific complaint in malaria, it should not be overlooked. SDH presenting with neurological manifestation though being common, its association with P.vivax malaria is extremely rare and should be considered as one of the differential diagnosis. SDH being unusual CNS presentation in case of P.vivax malaria warrants imaging and prompt management.
Conclusion
We highlight the need for early identification of unusual presentations of common diseases like malaria. Though altered sensorium is a common manifestation in cerebral malaria other haemorrhagic complications like SDH should be taken into consideration as differential, in regions endemic to malaria. Early and prompt management will reduce significant morbidity and mortality associated with the disease.
[1]. Nicholas JW, Joel GB, Malaria. In: Fauci AS, Kasper DL, Longo DL, Braunwald E, Hauser SL, Jameson JL, et al, editorsHarrison’s Principles of Internal Medicine 2008 17 ednNew YorkMcGraw-Hill:1280-93. [Google Scholar]
[2]. Chaudhary SC, Sonkar SK, Kumar V, Gupta A, Falciparum malaria presenting as subdural haematomaJ Assoc Physians India 2011 59:325-26. [Google Scholar]
[3]. Huda MF, Kamali NI, Srivastava VK, Kaif M, Spontaneous acute subdural haematoma in malaria: A case reportJ Vector Borne Dis 2011 48:247-48. [Google Scholar]
[4]. Thirumal Y, Alugolu R, Spontaneous chronic subdural haematoma following Plasmodium vivax malaria: a rare associationJournal of Vector Borne Diseases 2014 51(1):73-74. [Google Scholar]
[5]. Kumar A, Shashirekha Thrombocytopaenia - an indicator of acute vivax malariaIndian J Pathol Microbiol 2006 49:505-58. [Google Scholar]
[6]. WHOSevere falciparum malariaTransactions of the Royal Society of Tropical Medicine and Hygiene 2000 94(1):S1-S90. [Google Scholar]
[7]. Wang HS, Kim SW, Kim SH, Spontaneous chronic subdural haematoma in an adolescent girlJ Korean Neurosurg Soc 2013 53:201-03. [Google Scholar]
[8]. Hesselbrock R, Sawaya R, Means ED, Acute spontaneous subdural haematomaSurg Neurol 1984 21:363-66. [Google Scholar]
[9]. De Noronha RJ, Sharrack B, Hadjivassiliou M, Romanowski CA, Subdural haematoma: A potentially serious consequence of spontaneous intracranial hypotensionJ Neurol Neurosurg Psychiatry 2003 74:752-55. [Google Scholar]
[10]. Grau GE, Taylor TE, Molyneux ME, Wirima JJ, Vassali P, Hommel M, Tumour necrosis factor and disease severity in children with falciparum malariaN Engl J Med 1989 320:1586-91. [Google Scholar]
[11]. Mannel DN, Grau GE, Role of platelet adhesion in homeostasis and immunopathologyMol Pathol 1997 50:175-85. [Google Scholar]
[12]. WHO guidelines for the treatment of malaria. Geneva, World Health Organization, 2010. http://whqlibdoc.who.int/publications/2010/9789241547925_eng.pdf (Accessed on December 30, 2010) [Google Scholar]