Skeletal tuberculosis (TB) accounts for about 9% of all TB cases. Tuberculosis of the sternum is not a common presentation. The case of primary multidrug-resistant (MDR) TB of the sternum is even rare. So far no such case has been reported in the medical literature. Herein, we present the very first case of primary extrapulmonary MDR TB of the sternum in a 21-year-old immunocompetent Indian female who presented with chest pain and an increased swelling over the anterior chest with an intermittently discharging sinus. She was diagnosed with multidrug-resistant tuberculosis of the sternum without the active pulmonary disease. Conservative management with oral multidrug antitubercular therapy (ATT) completely cured the patient.
Antitubercular therapy, History taking, Osteomyelitis, Sternum
Case Report
A 21-year-old Indian female, presented to the OPD with a painful swelling with intermittent discharge from the lower part of the sternal region since two months. The swelling was about 1×1 cm two months back, which gradually increased to a size of about 5×5 cm about 15 days back when it was associated with a purulent, non-sticky, non-foul smelling discharge. Since the time of the onset of discharge, the swelling had regressed in size and the discharge was intermittent. At the time of the presentation she had a swelling of about 3×3 cm. There was a history of intermittent fever; loss of appetite and loss of weight about six kilograms in the last three months. There were no respiratory complaints or past history of tuberculosis. However, the women gave a family history of MDR-TB to her mother-in-law, who was treated for pulmonary MDR-TB one year back. Besides, there was no history of trauma or any major surgical or medical intervention in the past.
On examination, the patient was thinly built, afebrile and with normal pulse and blood pressure. The systemic examinations were normal. Local examination revealed a 3×3 cm swelling over the sternum. There was no visible discharging sinus. The lesion was soft, fluctuating, tender, warm, with well-defined margins, movable, and not attached to the underlying bony structures [Table/Fig-1]. There were no palpable regional lymph nodes.
Picture showing the anterior chest wall swelling.

Since the lesion appeared inflamed, the patient was given an oral antibiotic course of a third generation cephalosporins. After completion of the antibiotic schedule, pus greyish white in color was aspirated and was sent to the lab for pyogenic culture and Ziehl-Neelsen (Z-N) staining. There was no growth of any pyogenic organism after 48 hours of the incubation, but acid fast bacilli (AFB) were seen in Z-N stain. The Adenosine deaminase level in pus was 448 IU/L, with necrotic materials and RBC’s present. The biochemical analysis of pus, showed sugar 64 mg/dl and protein 7.6 g/dl. The TLC was 64500 per cumm with mainly lymphocytes 95 percent. Routine Blood investigations revealed hemoglobin 9g/dl, TLC-8700 per cumm, RBC count 3.77 million/cumm, PCV 30.8 percent, MCH-26.53. Mantoux test was strongly positive with induration of 17×18 mm after 72 hours. Rest all blood investigations were within the reference range. The AFB smear of sputum was negative.
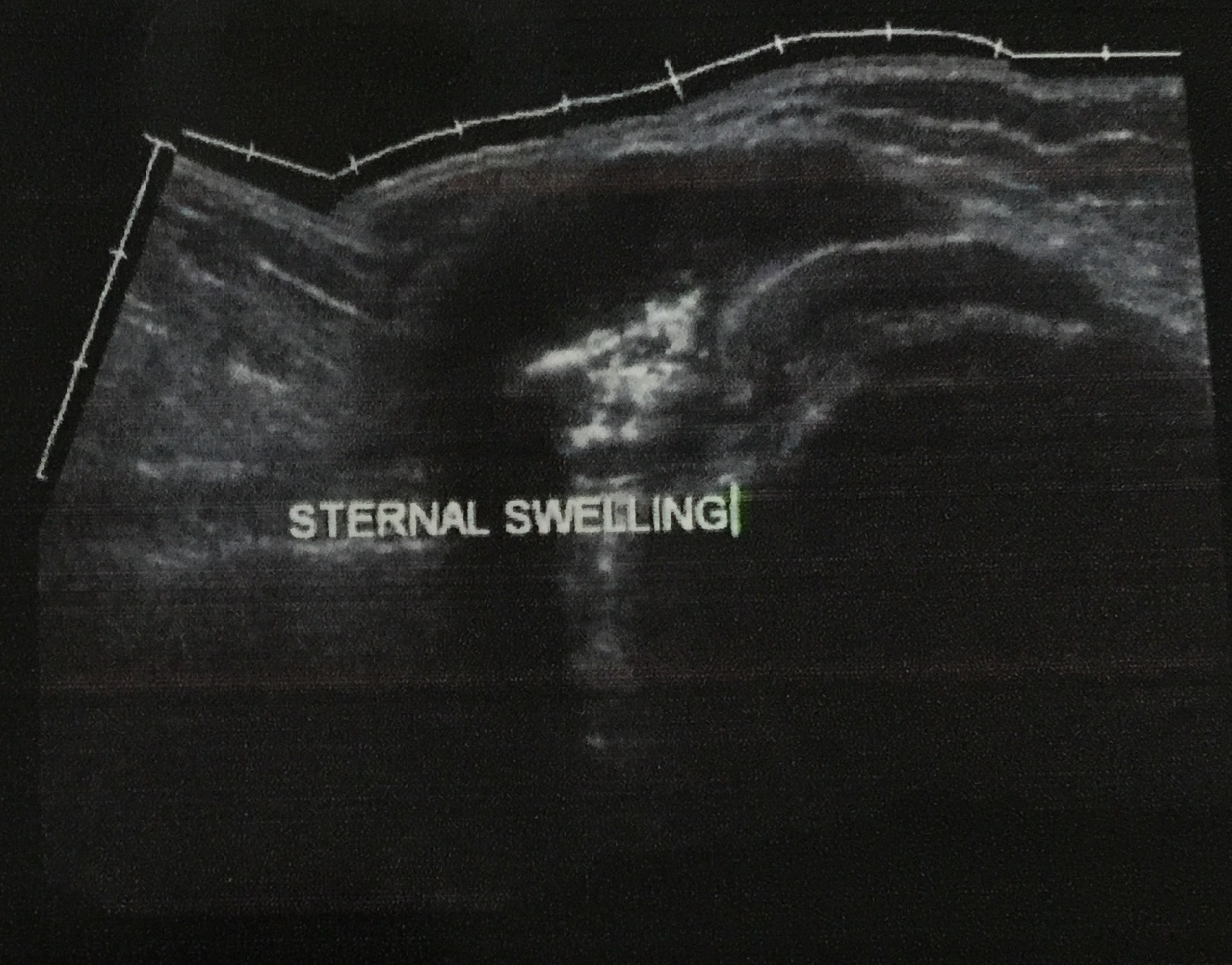
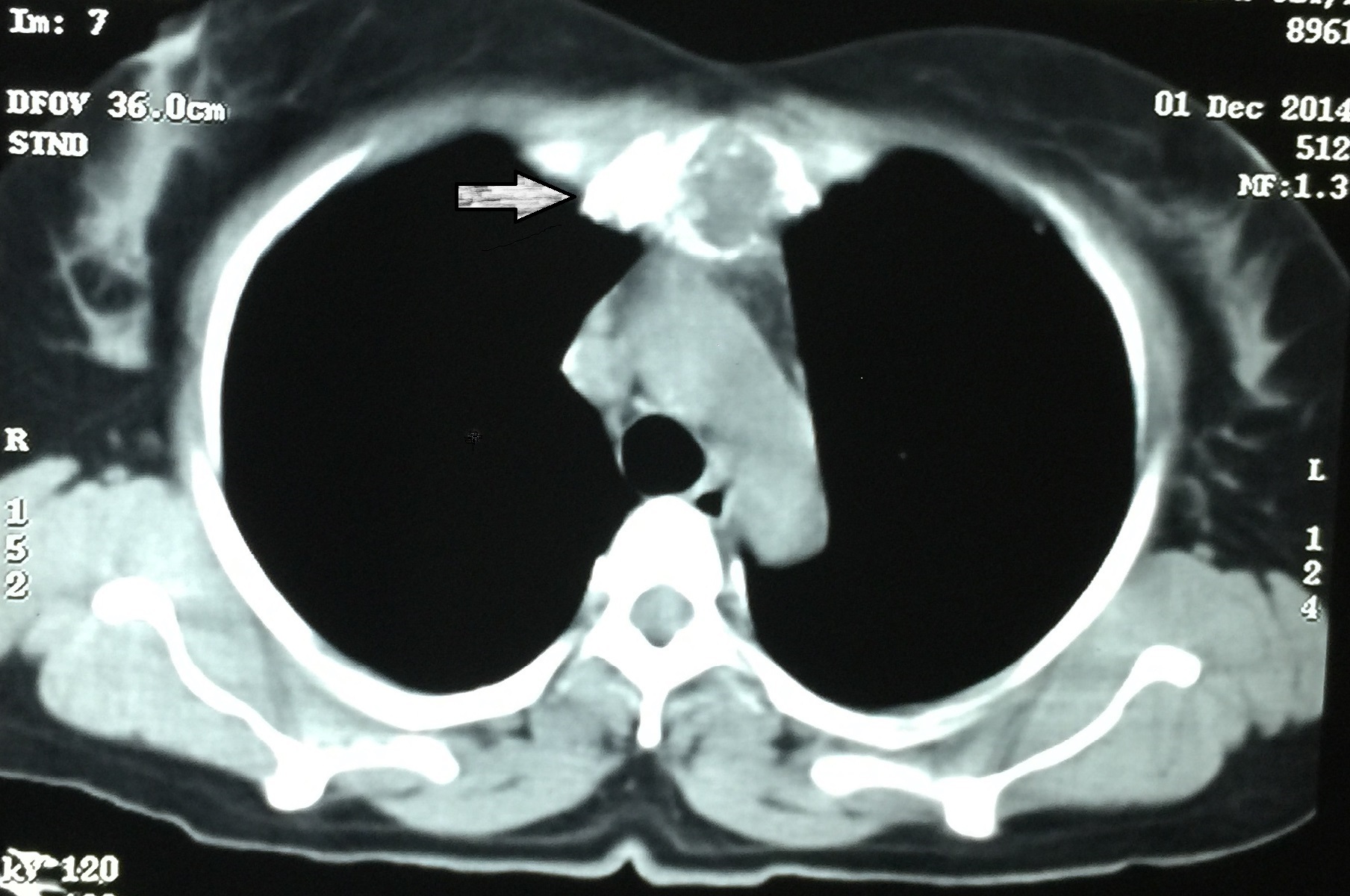
Ultrasonography of the chest revealed 55×50×20 mm sized hypoechoic partially cystic lesion seen in the subcutaneous tissues of the left side of the midline, extending up to the sterno-chondral junction and also there was focal, partial destruction of the bone. Thus, suggesting abscess formation in the sternal/parasternal region on the left side with bone involvement [Table/Fig-2]. The chest radiograph PA view was normal [Table/Fig-3]. Serology for HIV was non-reactive. A CECT of the chest revealed a hypodense lytic lesion eroding the body of the sternum, with chest wall, suggestive of osteomyelitis of the sternum with cold abscess formation [Table/Fig-4]. Also, there was no evidence of either lung parenchymal lesion or mediastinal lymphadenopathy. Ultrasound of the abdomen was within normal limits.
USG-Chest suggesting abscess formation in the sternal/parasternal region on the left side with bone involvement.
Chest radiograph PA view showing normal lung fields.

CECT of the chest suggesting a hypodense lytic lesion eroding the body of the sternum, with chest wall, suggestive of osteomyelitis of the sternum with cold abscess formation.
The pus sample was also sent to the National Reference Laboratory for culture and sensitivity of Mycobacterium tuberculosis, in view of the family history of MDR-TB. Sample grew M. tuberculosis on Lowenstein Jensen medium after seven weeks of incubation. In-line probe assay (GenoType MTBDRplus, Hain Life Science, Nehren, Germany), the isolate, was identified as M. tuberculosis and found to be resistant to Isoniazid (H) and Rifampicin (R) but was sensitive to other first line drugs, that is, Pyrazinamide (Z) and Ethambutol (E) by Bactec MGIT (Mycobacteria Growth Indicator Tube) 960 system.
Thus, a diagnosis of primary extrapulmonary multidrug-resistant tuberculosis of the sternum was made. The patient was started on 2nd line anti tubercular therapy (ATT) with Kanamycin 0.75 g, Levoflox 750 mg, Cycloserine 750 mg, Ehionamide 750, PAS powder 10 gm and Ethambutol 1.2 g, Pyrazimide 1.5 g. After six months of treatment Kanamycin was stopped and the rest of the drugs were continued for 18 months. Her symptoms improved after three months with swelling subsided, pain in the chest had reduced and the intermittent pus drainage had stopped completely. The patient was on regular follow-up and she completed 24 months of treatment and had no recurrence till date. A written and an informed consent was obtained from the patient to publish the case details.
Discussion
Tuberculosis (TB) is an infectious disease caused by airborne transmission by the acid fast bacillus Mycobacterium tuberculosis and is an important cause of death worldwide [1]. Since, 1990 the drug resistant TB has become a major public health problem [2]. In the year 2013, the WHO estimated the prevalence of primary MDR-TB in India around 3.5%; however, this prevalence is 20.5% among previously treated cases [3–5]. Primary MDR extrapulmonary TB is an uncommon form of the disease, even in the immunocompromised patients, and it requires a great deal of suspicion to diagnose such a case [4]. There is scanty information regarding extra-pulmonary primary MDR-TB in the literature [6]. The MDR-TB develops due to spontaneous mutations in the genes of the bacilli. The MDR-TB is basically a man-made problem, as a result of improper or poorly administered treatment [7,8].
The tuberculous osteomyelitis of the sternum is rare presentation and the literature concerning it is sparse [9–11]. It accounts for less than one percent (%) of cases of musculoskeletal tuberculosis [12]. The diagnosis is often delayed because of unusual presentation and unfamiliarity. In a large study Tuli and Sinha reported 14 cases of TB of sternum in a series of 980 cases of osteoarticular TB however, this study lacked the use of advanced imaging modalities such as MRI [13]. This study also reported that nearly 1/3rd of these 14 patients had detectable TB lesions in the lungs [13]. In a more recent study by Davies et al. 1984, reported only two cases of TB of the sternum out of the total 4000 cases [14]. So far, a case of primary extrapulmonary MDR-TB of the sternum without pulmonary involvement is not available in the medical literature.
TB of the sternum is more common in young adults, affecting more males than females [15]. The clinical findings in such cases are sternal and sterno-clavicular pain, painful swelling, cold abscess with or without a discharging sinus, in addition to other constitutional symptoms of TB [15]. The differential diagnosis of a sternal lesion includes: inflammatory conditions such as acute pyogenic osteomyelitis; sub-acute osteomyelitis; fungal, actinomycosis and parasitic infections; sarcoidosis and malignancy [15]. The diagnosis involves a detailed history taking with the FNAC of the swelling followed by histopathology and culture [15]. The role of history taking is very important, as the clinical features of the disease are often subtle and are difficult to detect in the early stages [15]. The radiological changes are also not conclusive in early stages. Therefore, a high index of suspicion is essential to make early diagnosis [15,16]. Newer and advanced diagnostic techniques like MRI and CT/CECT chest with sternum are indicated in detecting pulmonary or mediastinal involvement, which may not be seen on plain chest radiographs [15]. The bacteriological diagnosis of TB and the drug sensitivity/resistance can be established by the Z-N staining, regular culture, and by BACTEC technique and polymerase chain reaction [17]. A negative microbiology initially does not rule out TB. Sometimes more than one effort at culture may be needed.
Similar cases have been reported in the past, but the present case differs from the published cases in the presence of the primary MDR TB in an immunocompetent patient and thus thus present case is a unique presentation which has not been reported till date [18–21].
Several treatment modalities are available: Anti TB drugs or in addition aspiration of the abscess, open drainage of cold abscess and removal of granulation tissue, curettage of bony lesion, partial resection of the sternum, and partial resection with reconstruction [15]. In general aspiration of the pus and adequate ATT is the treatment of choice. The surgical treatment is rarely justified for a doubtful diagnosis, nonresponsive case or for removal of a large sequestrum [15]. However, further studies with longer follow up would be necessary to clearly establish the indications for surgery in this condition. MDR-TB is generally thought to have high mortality rates [8].
Conclusion
The emergence and spread of drug resistance can be prevented by a detailed history taking, prompt diagnosis and effective treatment of all drug sensitive and resistant cases. High failure rates are usually seen in the treatment of drug resistant TB. Thus the role of psycho social support and regular counselling are very important for the proper completion of the treatment.
[1]. Yadav S, Rawal G, Tubercular Nodular Episcleritis: A Case ReportJ Clin Diagn Res 2015 9(8):ND01-02. [Google Scholar]
[2]. Pablos-Méndez A, Raviglione MC, Laszlo A, Binkin N, Rieder HL, Bustreo F, Global surveillance for antituberculosis-drug resistance, 1994-1997. World Health Organization-International Union against Tuberculosis and Lung Disease Working Group on Anti-Tuberculosis Drug Resistance SurveillanceN Engl J Med 1998 338(23):1641-9.pmid: 9614254 [Google Scholar]
[3]. “Global Tuberculosis Report 2014”, WHO, Geneva, 2014 Available from URL: www.who.int/tb/publications/global_report/. Last accessed 2015 on October 6 [Google Scholar]
[4]. Rawat J, Sindhwani G, Dua R, Primary multi-drug resistant tubercular lymphadenitis in an HIV infected patientIndian J Tuberc 2009 56:157-59. [Google Scholar]
[5]. Sharma SK, Mohan A, Multi-drug resistant extra-pulmonary tuberculosis in a HIV negative patientIndian J Tuberc 2004 51:43-46. [Google Scholar]
[6]. Tageja N, Sharma V, Multidrug-resistant tuberculosis in IndiaLancet 2010 376:682-83. [Google Scholar]
[7]. Kant S, Saheer S, Hassan G, Parengal J, Extra-pulmonary primary multidrug-resistant tubercular lymphadenitis in an HIV negative patientBMJ Case Rep 2012 2012 [Google Scholar]
[8]. Mittal N, Bansal P, Multidrug resistant extrapulmonary tuberculosis – three case reports and review of literatureIntern Med Inside 2014 2:2 [Google Scholar]
[9]. Sharma S, Juneia M, Garg A, Primary tubercular osteomyelitis of the sternumIndian J pediatr 2005 72:709-10. [Google Scholar]
[10]. Choi H, Lee CJ, Lee KJ, Moon KD, Primary tuberculous osteomyelitis of the sternumJ.Cardiovasc Surg (Torino) 2001 42:841-43. [Google Scholar]
[11]. Sipsas NV, Panayiotakopoulos GD, Zormpala A, Thanos L, Artinopoulos C, Kordossis T, Sternel tuberculosis after coronary bypass graft surgeryScand J infect. Dis 2001 33:387-88. [Google Scholar]
[12]. Khan SA, Varshney MK, Hasan AS, Kumar A, Trikha Tuberculosis of the sternumJ Bone Joint Surg 2007 89:817-20. [Google Scholar]
[13]. Tuli SM, Sinha GP, Skeletal tuberculosis "Unusual" lesionsIndian Journal of Orthopaedics 1969 3:5-18. [Google Scholar]
[14]. Davies PD, Humphries MJ, Byfield SP, Nunn AJ, Darbyshire JH, Citron KM, Bone and joint tuberculosis : a survery of notifications in England and WalesJ Bone Joint Surg 1984 66(3):326-30. [Google Scholar]
[15]. Haynes W, Govender S, Tuberculosis of the sternum in patients with infective spondylitisSA Orthop J 2010 9(3):26-30. [Google Scholar]
[16]. Tristano AG, Willson ML, Lopez A, De Abreu F, Sternal osteomyelitis caused by mycobacterium tuberculosis: case report and review of the literatureInfect Dis Clin Pract 2004 12:174-77. [Google Scholar]
[17]. Panicker JN, Nagaraja D, Subbakrishna DK, Venkataswamy MM, Chandramuki A, Annals of Indian Academy of Neurology 2010 13(2):128-31. [Google Scholar]
[18]. Vasa M, Ohikhuare C, Brickner L, Primary sternal tuberculosis osteomyelitis: A case report and discussionCan J Infect Dis Med Microbiol 2009 20(4):e181-84. [Google Scholar]
[19]. Jain A, Chawla S, Kumar M, Sternal tuberculous osteomyelitis: a series of four casesInt J Community Med Public Health 2015 2(3):288-92. [Google Scholar]
[20]. Manu MK, Mohapatra AK, Magazine R, Extrapulmonary multidrug resistant tuberculosis presenting as chest wall abscess –A rare case reportIndian J Tuberc 2013 60:121-23. [Google Scholar]
[21]. Kant S, Maurya AK, Kushwaha RA, Nag VL, Prasad R, Multi-drug resistant tuberculosis: an iatrogenic problemBiosci Trends 2010 4:48-55. [Google Scholar]