Renal Papillary Necrosis (RPN) is idefined as Ischemic necrobiosis of the papilla in the medulla of the kidneys. Variety of etiological factors are recognized which cause papillary necrosis, such as analgesic nephropathy, diabetes mellitus, urinary obstruction and sickle cell haemoglobinopathy. The early diagnosis of RPN is important to improve prognosis and reduce morbidity. Radiological Imaging offers early diagnosis and can guide prompt treatment of papillary necrosis and can minimize a decline in renal function. Here we report three cases of RPN with typical imaging findings. One of them was diabetic and hypertensive female with recurrent Urinary tract Infections and other was a male with no known co-morbidity. Both of them were diagnosed to have renal papillary necrosis on CT scan and were managed operatively and conservatively, respectively. Third case was a healthy female being investigated to be renal donor for her son. Here RPN was an incidental finding and was treated conservatively. Thus CT scan could detect it pre-operatively and complications due to transplantation of a kidney with papillary necrosis were avoided. So, we want to emphasize the importance of Radiology, particularly CT scanning in detection of RPN and to guide early and prompt treatment.
CT-scan, Papillae, Transplantation
Case Report
Case 1
A 48-year-old diabetic and hypertensive female with recurrent history of urinary tract infection presented with complaints of Flank pain, Urgency and frequency of Micturition, Haematuria and lower abdominal pain. On physical examination, temperature was normal. Blood Pressure measured 130/90 mm Hg. Retinal examination revealed Grade III Diabetic retinopathy changes. On Laboratory investigations, Serum Creatinine was increased and pus cells and Red blood cells were present in Urine. Plain X ray KUB showed no abnormality. On Ultrasound, both kidneys showed hydronephrosis and multiple echoes within the Pelvi calyceal system. CT IVP was done and it showed normal excretion of contrast with presence of multiple non enhancing filling defects in Pelvi calyceal systems [Table/Fig-1a,b]. Provisional Diagnosis of Renal papillary necrosis was made on CT scan. Cystoscopy confirmed the presence of RPN and Sloughed papilla were removed with placement of PCN tube. No residual Disease was found in Check nephrostomogram performed after a week. On follow up, the patient is doing well with no complaints.
Axial section of Delayed phase of CT scan showing normal excretion of contrast with multiple filling defects in Pelvi calyceal system (white arrow).

MPR reformation of coronal section of Delayed phase of CT scan showing normal excretion of contrast with multiple filling defects in Pelvi calyceal system (white arrow).

Case 2
Another 40-year-old non diabetic male patient presented with flank pain and haematuria. Physical and Laboratory Findings were within normal limits. Renal function tests were normal. Plain X ray KUB was normal. On Ultrasound, presence of bilateral hydronephrosis with internal echoes was seen. Retrograde Pyelography showed multiple filling defects. CT IVP showed presence of hydronephrosis with multiple non enhancing filling defects in Pelvi calyceal system which also extended in to pelvis [Table/Fig-2a,b]. Cupping of all the calyces was seen consistent with the Egg in the Cup deformity seen typically in renal papillary necrosis. So, radiologically diagnosis of RPN was made and he was maintained conservatively and is asymptomatic on follow up.
Axial section of Delayed phase of CT scan showing normal excretion of contrast with multiple filling defects in Pelvi calyceal system and pelvis (white arrow).

MPR reformation of coronal section of Delayed phase of CT scan showing normal excretion of contrast with multiple filling defects in Pelvi calyceal system (black arrow).

Case 3
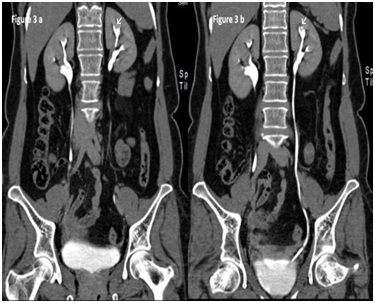
A 55-year-old healthy female was being investigated as a potential Donor for her Son. Ultrasound of kidneys was unremarkable. CT Renal Angiography was performed for vascular assessment. It showed evidence of cupping and Ball in cup appearance of Pelvi-Calyceal system on either side [Table/Fig-3a,b]. So, probable diagnosis of RPN was thought of and she was investigated further. On detailed clinical investigations after the probable diagnosis of RPN, she found to be frequent Analgesic user for back pain. Unfortunately she was rejected for Donation and was kept on conservative treatment of RPN. On follow up, she is doing well.
MPR reformation of coronal section of Delayed phase of CT scan showing normal excretion of contrast with cupping of visualized calyces.
Discussion
RPN is an entity caused by necro-biosis of renal papilla in medullary region [1]. Varieties of factors can cause RPN. It is commonly seen bilaterally and it can also affect a single papilla. Mean age of presentation is 40 years in more than 90% of cases. Women are more commonly affected than men. The exact prevalence of RPN is unknown. Transplanted kidneys, from cadavers, appear to be more susceptible to renal papillary necrosis. Analgesic nephropathy is considered the most common causative factor; most common is phenacetin [2]. Other major causes include Diabetes mellitus (IDDM in 24% cases), Urinary obstruction with infection. Rarely may it occur as a result of severe acute infection without other factors. ARF in infancy may also complicate subsequently as Papillary Necrosis [3]. S - haemoglobinopathy is also a major cause. RPN occurs more frequently in patients with diabetes mellitus (DM). Incidence of developing RPN in patients with DM is 2.7% to 7.2 %and in patients without DM is reported to be less than 0.3 % [4]. Radiological evidence of RPN has been reported in as many as 23.7% of patients with long-standing Insulin dependent Diabetes Mellitus [5,6]. Other causes include shock, Dehydration, Hypovolaemia, Sickle cell disease, Tuberculosis, Trauma, Cirrhosis, Coagulopathy, Renal vein thrombosis, Haemophilia, Christmas disease, Acute tubular necrosis etc. RPN may be asymptomatic but when present, symptoms include fever and chills, flank and/or abdominal pain, haematuria and acute ureteral obstruction from sloughed papillae [3]. Clinical picture in such cases may also include fever, chills and sepsis. Acute renal failure with oliguria or anuria is rare presentation. In Acute RPN, kidneys appear enlarged and in chronic type, patchy papillary or calyceal changes are seen in early stages and all papillae are affected to some extent in later stages. RPN may affect single papilla or the entire kidney. Distal zone of medulla and papilla are more commonly involved. RPN is classified as focal or diffuse according to the area involved [4]. If renal function deteriorates suddenly in a patient with patients of diabetes, in a patient with a known history of chronic obstruction and/or pyelonephritis, the diagnosis of papillary necrosis can be suspected even if the patient is asymptomatic. Increased urinary white cell excretion rate in absence of bacteriuria also can be a signal to look for renal papillary necrosis [3]. Differential diagnosis of RPN includes Focal reflux nephropathy, Tuberculosis, Back pressure atrophy, Localized papillary atrophy associated with calculus disease, medullary sponge kidney and Calyceal cyst [7]. Radiological diagnosis of RPN depends upon demonstration of appropriate papillary/ calyceal abnormality without focal loss of renal substance. The imaging study should be done prior to cystoscopy and if it is inconclusive Retrograde Pyelography can be done to confirm the diagnosis.
Cases from available literature were reviewed. In all reviewed cases presence of varied etiological factors was seen and radiological imaging was the key factor in diagnosis even in absence of strong prediction of RPN [Table/Fig-4].
Shows Various Aetiological factors and Diagnosis of RPN.
| Sr No. | Study (author name) | Year | Age(years) | Sex | Type of organ | Etiology | DiagnosisDone on |
|---|
| 1 | Zadeii G et al., [2] | 1997 | 66 | M | native | Sickle cell trait | IVU |
| 2 | Eknoyan G et al., [5] | 1989 | 23 | M | Allo graft | Epstein’s syndrome | USG |
| 3 | Saravu K et al., [8] | 2013 | 42 | M | Native | Fungal | Biopsy |
| 4 | Brenke B et al., [9] | 1996 | 27 | F | Native | Analgesic Abuse | USG |
Importance of various Imaging studies and appearance of RPN is as follows:
Plain Radiograph: Is not diagnostic. However, it rules out presence of calculus. Calcification in a sloughed papilla appears as a calcified ring shadow and it is commoner in patients with analgesic nephropathy than in S haemoglobinopathy [10–12].
Intravenous urography: Is the investigation of choice. It gives excellent display of anatomy and Calyceal dilatation. Persistent streaking of contrast from the fornix at the upper and lower poles is most specific feature of renal papillary necrosis. However, Intravenous urography is contraindicated in patients with azotaemia and other known allergy to contrast media. Various findings useful to diagnose RPN on intravenous urography include:
Shrinkage and irregularity of papillae, with consequent widening of calyceal fornices, which is known as hooks and spurs.
Desquamated papilla in situ, demarcated by contrast material as a ring shadow.
A calyx without a papilla.
Partially calcified filling defect in the renal pelvis known as sequestered papilla.
Contrast-containing rice grain sized cavaties in the papilla are the pathognomonic feature of the medullary form of renal papillary necrosis [13].
Retrograde pyelography: is more invasive. However, it is useful when the renal collecting system opacifies poorly with intravenous contrast or when there is renal insufficiency. Antibiotics prophylaxis is needed prior to this imaging. Images may reveal a clubbed calyx or a filling defect in the PC system or ureter [13].
Ultrasound: Is safe, quick, inexpensive, noninvasive, and diagnostic for hydronephrosis, calculi and certain anomalies. However, it is operator dependant and not sensitive enough to be confirmatory in the earlier (reversible) phases. Filling defects in the pelvi calyceal system or ureter, necrosed papillae in cavities in the medullary region are seen on ultrasound. Associated hydronephrosis may be seen. Tumour, calculus and clots are various differential diagnosis of sloughed papilla [13].
CT scan: Is the investigation of choice to rule out calculus. However, it is less sensitive than IVU and not specific for Papillary Necrosis. Features are most visible on CT in the excretory phase, when hyper attenuated urine with contrast material fills the clefts and delineates the destructive process [13].
Magnetic Resonance Imaging: Is useful for patients with known contraindications for CT scans (i.e. allergy to contrast media and poor renal function). However, gadolinium may cause nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD) [13].
Radionuclide studies are useful to assess renal function but they provide little anatomic information on the location of lesions [13].
Regarding treatment of the renal papillary necrosis, Prevention of recurrent infection, control of infection and control of diabetes are first to be achieved. However, early diagnosis holds the clue to proper management of such patients. Thus Radiological imaging plays a pivotal role for early diagnosis in even asymptomatic patients. Infection, Obstruction, Calculus formation due to slough papillae and development of Transitional Cell Carcinoma are the known complications of Renal Papillary necrosis.
Conclusion
Radiology plays a pivotal role in early diagnosis of renal papillary necrosis by diagnosing it at early stage. Thorough knowledge can guide us about choosing proper imaging study at proper time in detecting RPN.
Abbreviations
RPN – renal papillary necrosis
KUB – Kidneys urinary bladder
CT scan - Computed tomography scan
IVU – Intravenous Urography
RGP – Retrograde Pyelography
PCN – Percutaneous Nephrostomy
[1]. Jung DC, Kim SH, Jung SI, Renal papillary necrosis: review and comparison of findings at multi-detector row CT and intravenous urographyRadiographics 2006 26(6):1827-36.PMID: 17102053 [Google Scholar]
[2]. Zadeii G, Lohr JW, Renal papillary necrosis in a patient with sickle cell traitJ Am Soc Nephrol 1997 8(6):1034-39.PMID: 9189873 [Google Scholar]
[3]. Grainger RG, Allison DL, Renal Parenchymal disease. In: Grainger RG, Allison DL editorsDiagnostic Radiology: A textbook of Medical imagingVol. 23rd ed:1358 [Google Scholar]
[4]. http://misc.medscape.com/pi/iphone/medscapeapphtml/A439586-business.html [Google Scholar]
[5]. Eknoyan G, Renal papillary necrosis. In: Massry SG, Glassock RJ editorsTextbook of Nephrology 2001 4th edBaltimore, MDLippincott Williams & Wilkins:1004-1010. [Google Scholar]
[6]. Shapeero LG, Vordermark JS, Papillary necrosis causing hydronephrosis in therenal allograft: sonographic findingsJ Ultrasound Med 1989 8(10):579-81.PMID: 2681830 [Google Scholar]
[7]. Grainger RG, Allison DL, Diagnostic Radiology: A textbook of Medical imaging. In: Grainger RG, Allison DL editorsRenal Parenchymal diseaseVol. 23rd ed:1359 [Google Scholar]
[8]. Saravu K, Vishwanath S, Shastry BA, Candidal Renal Papillary Necrosis ConqueredJ Assoc Physicians India 2013 61(8):573-74.PMID: 24818347 [Google Scholar]
[9]. Brenke B, Nahm AM, Ritz E, Papillary necrosis in a ballet dancer with no history of analgesic abuseNephrol Dial Transplant 1996 11:2501-3.PMID: 9017634 [Google Scholar]
[10]. Pedrosa I, Sun MR, Spencer M, MR imaging of renal masses: correlation with findings at surgery and pathologic analysisRadiographics 2008 28(4):985-1003.PMID: 18635625 [Google Scholar]
[11]. Craig WD, Wagner BJ, Travis MD, Pyelonephritis: radiologic-pathologicreviewRadiographics 2008 28(1):255-77.PMID: 18203942 [Google Scholar]
[12]. Prasad SR, Narra VR, Shah R, Segmental disorders of the nephron: histopathological and imaging perspectiveBr J Radiol 2007 80(956):593-602.PMID: 17621606 [Google Scholar]
[13]. Papillary Necrosis, Christopher Powell, Bradley Fields Schwartz, http://emedicine.medscape.com/article/439586-overview [Google Scholar]