According to the UNSCEAR (United Nations Scientific Committee on Effects of Atomic Radiation) as reported in the year 2008, approximately 480 million of diagnostic radiographic examinations in dentistry are done worldwide annually and these dental radiographic examinations comprise of 15% of all diagnostic X-ray examinations in health care [1].
Furthermore, dentists use radiographs more frequently than any other health profession [2]. Lack of robust quality assurance programmes and high paediatric use also make the radiation safety measures more important for the dentists to adopt. Statistically, radiation exposures in dentistry have been associated with salivary gland tumours, thyroid cancer, meningioma and low birth weight babies in pregnant females. Radiation doses used during dental treatment might be low for individual examinations but most of the time, patients are exposed to repeated examinations and many people are exposed during the course of dental care [3]. Thus, besides the extensive benefits obtained from the diagnostic application of X-rays in both medicine and dentistry, professional negligence or ignorance can lead to radiation hazards which are harmful to the living tissues in a way that is enough to cause cancer [4].
In terms of reducing the radiation dose, the optimization and justification of radiography is now an important issue for dental professionals [2]. In order to reduce patients’ exposure to radiation, appropriate use of a lead apron, thyroid collar, right collimation and suitable technique are included in the practice of radiologic examination. Every deliberate radiographic exposure to the patient during the examination and treatment procedure should be clinically justified and each exposure should be expected to give the benefit of a confirmed diagnosis. Since radiographic examinations in dentistry are one of the most frequent radiological procedures, radiation hazards caused by diagnostic X-rays have been one of the primary public health concerns [3]. Therefore, a radiograph shall be recommended only for a patient when the benefit of disease detection outweighs the risk of damage from x-radiation [4].
Considering the concerns mentioned above regarding the radiographic exposure involved in dentistry for both the patient and the dentist, this study was conducted with the aim to investigate the knowledge and behaviour of general dentists practicing in Noida regarding radiation safety during oral radiographic procedures.
Materials and Methods
The study was conducted in the Department of Public Health Dentistry at I.T.S Dental College, Hospital & Research Centre, Greater Noida. The database for the sampling of general dentists practicing in Noida was extracted from the office of IDA. From the list of the general dentists practicing in Noida, the sampling was done randomly. The general dentists practicing at their own clinic or a hospital in Noida were included in the study whereas the specialist dentists and post graduate students were excluded from the study. A total of 500 questionnaires were distributed to the general dentists practicing in Noida. Two hundred and fifty questionnaires were distributed personally to the dentists practicing nearby the author for convenience and the other 250 were distributed online to the dentists practicing far away via esurveyspro.com. The questionnaire given/sent to the participants included informed consent and a covering letter. The total response rate recovered was 70.6% including both online and offline responses.
The prevalidated questionnaire used in the study was adopted from Shahab S et al., [2]. This questionnaire was pilot tested on 50 dentists in Noida before the required modifications were made and these 50 dentists were included in the main study itself. The inter-examiner reliability was found to be 0.8 (Kappa Statistics). The questionnaire consisted of a set of 22 statements(apart from demographics) which were concerned with the practitioner’s knowledge about the relative radiation exposure in different techniques and their opinion on the role of radiation protection in dentistry. Also, the appropriate application of this knowledge for correct patient selection criteria, right use of equipment and positioning and radiation protection barriers and modification of exposure dose in order to protect themselves and their patients from radiation hazards was also a segment of the questionnaire. Of all the close-ended questions, three were demographic based questions, seven were knowledge based questions and 15 were practice based.
Prior to administration of the questionnaire the institutional ethical committee approval was obtained. The study was completed in a time frame of 4 months. Data was computed and tabulated in Microsoft excel worksheet and statistical analysis was performed using SPSS version 21.0.
Results
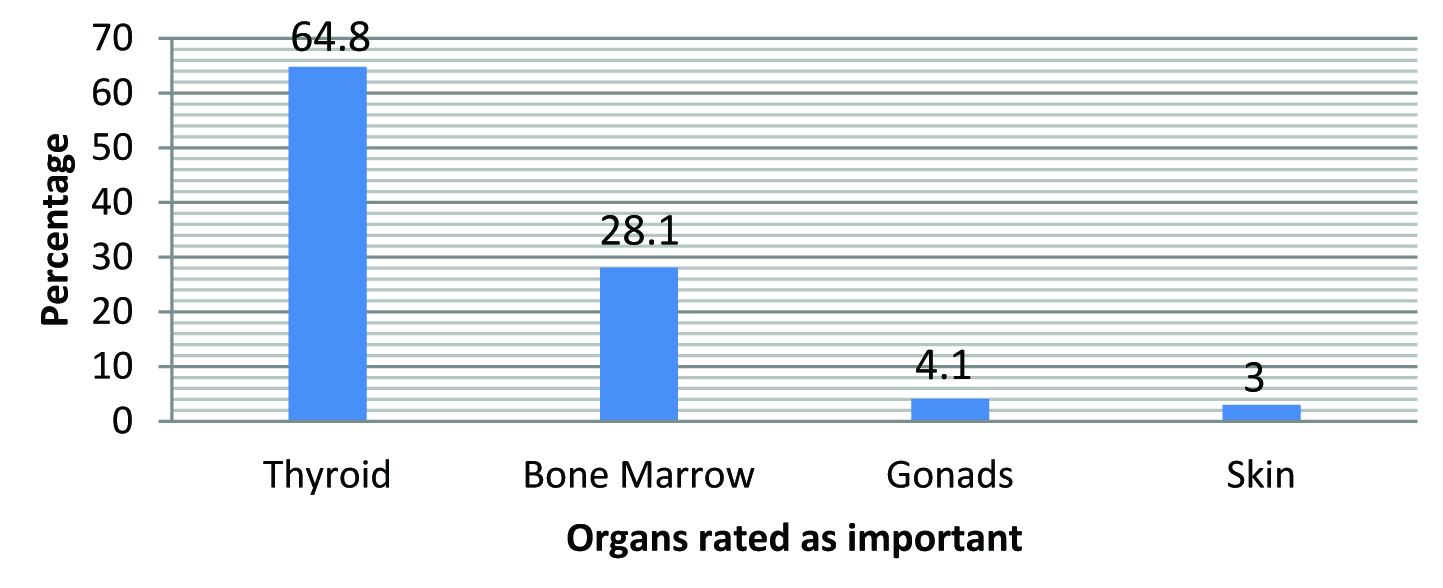
Out of all respondents, 59% were males and 41% were females. It was found that 86% owned an X-ray machine. It was seen that 91.7% (324) knew the correct rationale for radiation protection. The answers by the general dentists suggested that most important organ for radiation protection is thyroid (64.8%) [Table/Fig-1]. Out of the total subjects, 69.1% (244) believed that full mouth radiography gave more radiation exposure to patients than panoramic radiography. A 71.1% of the dentists used radiographic film as their radiographic receptor.
Most important organ for radiation protection as per the opinion of study population.
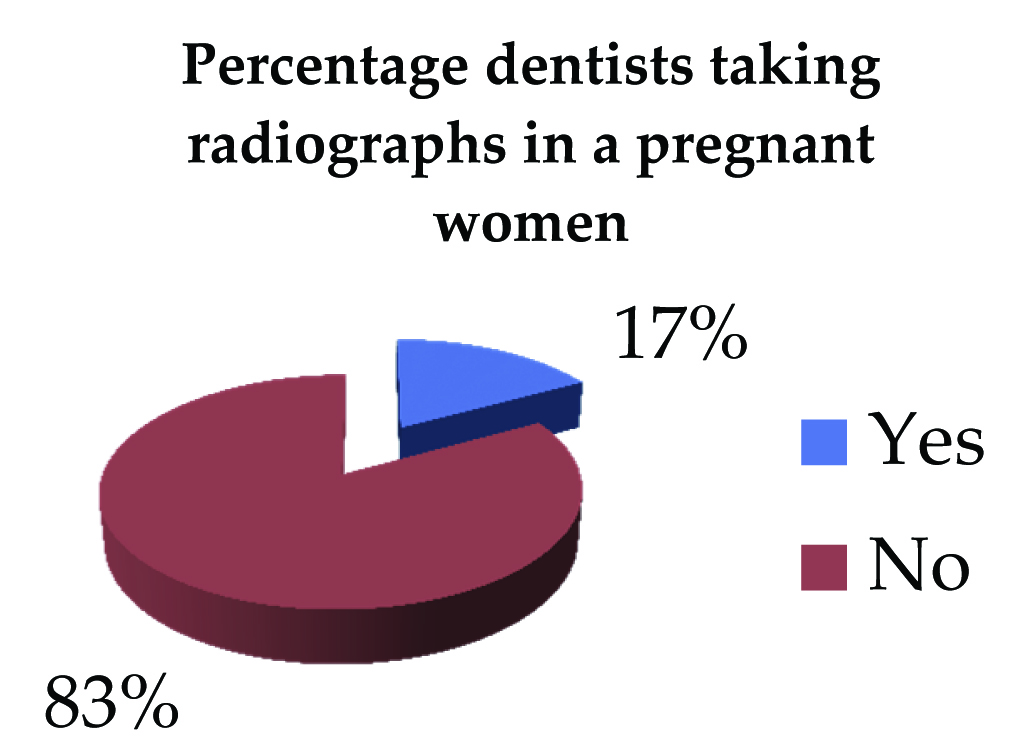
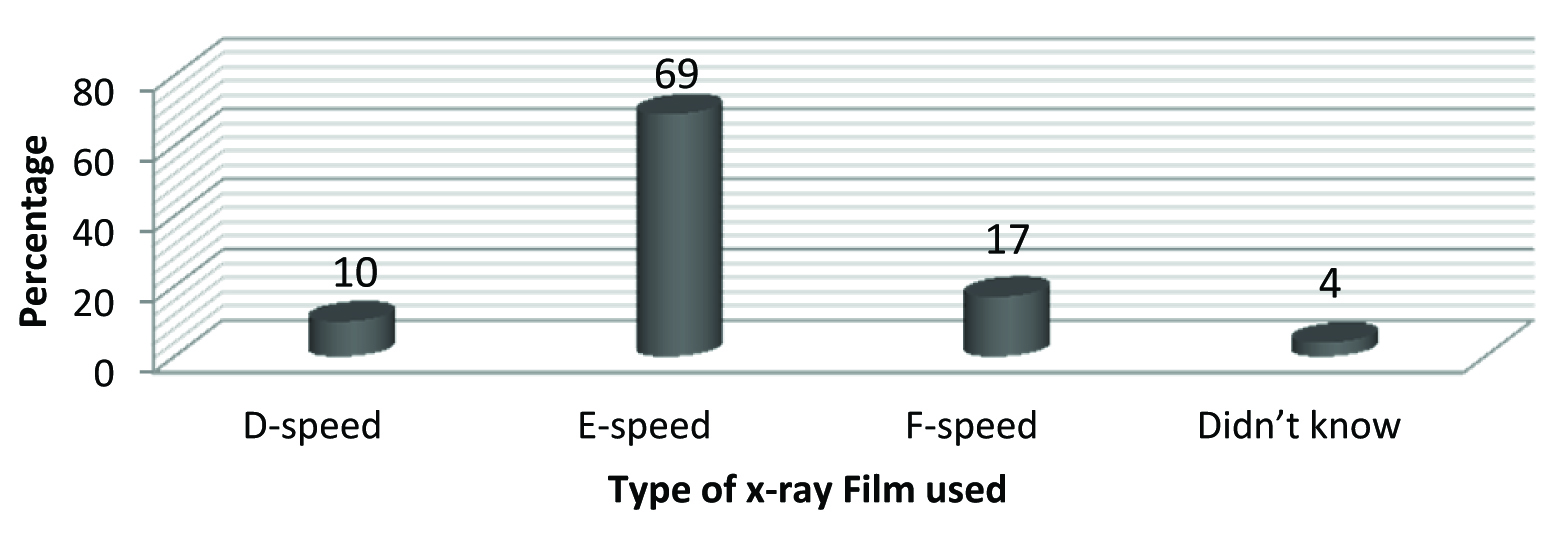
It was found that 86.1% (304) preferred selective periapical view in initial visits. The preference on taking radiographs in pregnant women has been shown in [Table/Fig-2]. Only, 19% of the general dentists got periodic check-ups of their machines done whereas, 89% followed bisecting-angle technique for taking radiographs and almost all the dentists accounting to 96% used round collimators. Majority of the general dentists used collimators of length 20cm [Table/Fig-3] and E films [Table/Fig-4]. Only 2% of dentists always used leaded apron and thyroid shield before shooting a radiograph. A total of 74% of the respondents used the same exposure time for all the patients and the locations of the tooth. Only 28.8% of the general dentists followed the position and distance rule correctly, 73.9% of dentists disposed of radiographic films with regular waste and 60.9% flushed the old developer and fixer solutions down the drain.
Study population affirmative of taking radiographs in pregnant women.
Distribution of study population according to the length of collimator used.

Distribution of study population according to the speed of x-ray film used.
There was no statistically significant difference found in the adoption of radiation protection techniques adopted in dental practice by male and female general dentists (p>0.05) [Table/Fig-5]. However, significant association was found in the knowledge regarding radiation exposure and safety among male and female general dentists [Table/Fig-6]. It was seen in the knowledge based questions lesser female dentists gave correct answers regarding thyroid, being the most important organ for radiation protection, IOPA, the most preferred radiograph for the initial visits, panoramic radiographs delivered less radiation exposure than full mouth radiography and exposure time for mandibular incisors was believed to be more than that for maxillary molar. Dentists who were operating X-ray machines older than five years had an increased tendency to use lead aprons, thyroid collars where as a decreased tendency to use film holders was observed among them (p<0.05) [Table/Fig-7]. It was also observed the dentists who used a digital receptor took more radiographs than the ones who used X-ray films [Table/Fig-8].
Association between gender and (i) periodic check-ups of x-ray machines, (ii) position & distance rule followed and (iii) Disposal of radiographic waste.
| Statement | Male | Female | Total | p value |
|---|
| Periodic check-ups of X-ray machines | 10.8% | 8.2% | 19% | 0.064 |
| Correct usage of position and distance rule | 19.7% | 9.1% | 28.8% | 0.071 |
| Proper disposal of radiographic waste | 44.7% | 29.2% | 73.9% | 0.056 |
Association between gender and knowledge (i) thyroid, as the most important organ for radiation protection (ii) preference for IOPA in initial visits, (iii) panoramic radiographs deliver less radiation than full mouth radiographs, (iv) variation of exposure time in mandibular incisors and maxillary molar.
| Statement | Male | Female | Total | p value |
|---|
| Thyroid, most important organ for radiation protection | 38.7% | 26.1% | 64.8% | 0.032 |
| IOPA, preferred radiograph in initial visits | 49.1% | 37.0% | 86.1% | 0.013 |
| Panoramic radiographs deliver less radiation than full mouth radiographs | 39.6% | 29.5% | 69.1% | 0.023 |
| Study participants who believed that exposure time for mandibular incisors is more that for maxillary molar | 9.4% | 7% | 16.4% | 0.037 |
Association of age of x-ray machine and radiation protection barriers & techniques used by the study population (i) usage of leaded apron & thyroid shield, (ii) film holder (iii) position and distance rule followed
| Statement | Less than five years | More than five years | Total | p value |
|---|
| Usage of leaded apron & thyroid shield(always or occasionally) | 14.1% | 17.0% | 31.1% | 0.043 |
| Use of film holders while taking radiographs | 41.3% | 11.1% | 52.4% | 0.010 |
| Correct usage of position and distance rule | 12.6% | 16.2% | 28.8% | 0.029 |
Association of number of radiographs taken with the receptor used
| Statement | Digital receptor | X-ray films | Total | p value |
|---|
| More than 16 radiographs per week | 36.8% | 20.1% | 56.9% | 0.043 |
Discussion
To be certain of the radiation safety of the patient and the operator, protocols, principles and guidelines have been given to achieve radiation exposure dose for the patient As Low As Reasonably Possible (ALARA). Not many studies focussing on radiation safety have been conducted in India.
The preference towards selective peri-apical view in initial visits was found to be in accordance with the study conducted by Shahab et al., in Iran [2]. This preference abides by the ALARA principle as it avoids any unnecessary radiation exposure. In case of radiographs taken by specialists of South India for dental implant assessment however, panoramic radiation has been seen as the preferred choice [5,6]. A greater percentage of dentists used conventional radiography, similar observations were made in another study done in Mumbai [7]. It was observed that a very low percentage of dentists got periodic check up of their X-ray machines and similar findings have been observed in a study done in states of Punjab & Haryana by Sheikh S et al., [8]. The periodic check up of X-ray unit was necessary to assure appropriate radiation exposue without any radiation leakage. According to Praveen BN a well calibrated dental X-ray machine will have an output of 0.7 to 1R/sec. This calibration must be done in every three years [9].
Bisecting angle technique is universally favoured for taking radiographs in this study and others conducted abroad by Shahab S et al., Mutyabule TK, Jacobs R et al., & Ilguy D et al., and in Punjab and Haryana in India [2,8,10–12]. However, paralleling technique involves less exposure due to scattered radiation to the thyroid gland and the eye and produces more accurate images. Whereas, due to the steep vertical angulation involved in bisecting angle technique, chances of radiation exposure of the thyroid gland and the lens of the eye are higher [9]. Majority of the dentists were not affirmative of taking radiographs in a pregnant women, this finding was a favourable one as according to the recommendations given by Praveen BS et al., in the Journal of Contemporary Dental Practice the greatest risk to the foetus for chromosomal abnormalities and subsequent mental retardation is between 8 and 15 weeks of pregnancy [9].
It has been shown in the studies conducted in Puducherry, Punjab and Haryana that majority of the dentists used round collimators and E-speed films [8,13]. Similar preferences have been seen in this study and also the ones conducted by Mutyabule TK, Ilguy D et al., Bohay RN et al., Alcaraz M et al., Huvakainen R et al., Jacobs R et al., & Geist JR et al., [10–12,14–17]. It has been shown that using of rectangular open ended PID (3.5x4.4cm) reduces the skin exposure by 60% than that of round [9]. E-speed film reduces the radiation dosage to about 50% as compared to the D-speed films and with the usage of F-speed films there’s further 20% reduction in radiation dosage.
It was observed disposal of radiographic waste was done improperly by the dentists. According to Praveen BN et al., in a questionnaire survey conducted in Bengaluru, it was found that 60% dentists were disposing the radiation waste into gutter [9]. Whereas, in another study conducted by Mehta A et al., in Chandigarh, it was observed that a safe system for health-care waste management and disposal was adopted by 96.4% but only 39.8% were sure whether they were following all Occupational Safety and Health Administration regulations in their clinic [18]. Fewer dentists knew the correct and safe distance rule to be maintained while taking radiographs as compared to the study conducted in Puducherry [13].
Most of dentists did not make any changes in the exposure time according to the location of the tooth and patient characteristics however on the contrary 72.5% and 65.6% of the dentists in Puducherry and Punjab and Haryana respectively did adjust the exposure time [8,13]. There was no statistically significant difference found in the adoption of radiation protection techniques adopted in dental practice by male and female general dentists in the study conducted by Binnal A et al., in Mangalore, India which was not observed in this study [19]. Dentists who were operating X-ray machines older than five years had an increased tendency to use lead aprons, thyroid collars whereas a decreased tendency to use film holders was observed (p<0.05) [Table/Fig-7]. In Puducherry, Punjab & Haryana, it was seen that approximately just half the dentists used film holders while taking radiographs [8,13]. These associations were seen in contrast to the study conducted by Binnal A et al., [19]. In Punjab & Haryana, only 19.2% and 4% of the dentists used lead apron and thyroid collars respectively [8]. Significant statistical association was also seen between the number of radiographs taken per week and the digital receptor used, this finding was in accordance with the study conducted by Berkhout WER et al., in the Netherlands [20].
Limitations
Since the sample in the study was not large enough, the results can’t be generalised and so further studies are required in this spectrum of research to obtain a better assessment of the radiation protection practice adopted by the general dentists.
Recommendations
The examinations at the undergraduate level for radiology should be taken intricately so as to ensure adequate knowledge of the budding professionals.
After graduation, the practitioners must keep their knowledge aligned with new evidences and this can be done by attending continuing dental education programmes. The information regarding this can be circulated on social websites as it is easier to reach a large population of dentists this way.
The periodic check-up of X-ray units should be made mandatory for the renewal of registration. On every renewal, the dentist must be handed over a brochure/pamphlet depicting any recent evidence based changes made in recommendations and guidelines provided by the authority. This can help in keeping the dentist updated with any new information beneficial for his practice in case he is not keen into looking into articles and journals himself.
Also, film badges for personal dosimetry should be compulsory to be worn by the dentist and the para-medical staff as well. Also, they should regularly/periodically evaluate the X-ray images for their quality in their clinics or offices so as to ensure optimal exposure reduction and suspect any radiation leakage as early as possible.
Conclusion
The results depict that the knowledge and practices adopted by the general dentists practicing is insufficient for maintaining proper protective barriers from radiation and adhering to the ALARA principle. Thus, methods should be devised so that the dentists abide by more strictly to the appropriate behaviour and practices towards radiation safety and the faculty members should come up with more impactful methods and medium of education for better understanding of the undergraduate students.