Intertrochanteric fractures are relatively common injury. Many epidemiological studies have shown increasing incidence of proximal femoral fractures, which is because of significantly increased life expectancy of the general population during the past few decades [1]. More than 90% of hip fractures in elderly are intertrochanteric fractures with complication rate of 20-30% and mortality rate of about 17% [1–3]. Most intertrochanteric femoral fractures occur in elderly individuals as a result of mild to moderate trauma due to osteoporotic bones while in younger patients, these fractures usually result from high-energy trauma [2]. Operative treatment is the best option in most of the cases of trochanteric fractures [4]. Conventional implants like dynamic hip screw, angular blade plates or cephalomedullary nails can be used for the successful treatment of stable intertrochanteric femoral fractures [5].
However, comminuted and unstable intertrochanteric fractures according to AO/ASIF classification (31-A1 stable intertrochanteric fracture, 31-A2/ 31-A3 unstable intertrochanteric fracture) and combined intracapsular and extracapsular fractures are challenging injuries that are prone to complications [6]. The use of cephalomedullary nails, when compared to the dynamic hip screw, has demonstrated increased fracture stability, with no difference in operation time or intraoperative complication rate [7,8]. Nevertheless, a high incidence of secondary implant failure ranging from 3% to 17% has been reported [9]. The current dictum for intertrochanteric fractures is “No Lateral Wall, No Hip Screw” [10]. Due to the absence of a lateral osseous buttress, there is uncontrolled collapse with medialization of the femoral shaft and lateralization of the proximal femoral fragment if a dynamic hip screw (DHS) is used, which results in varus collapse, femoral head screw cut out and nonunion [Table/Fig-1].
To overcome the complications associated with dynamic hip screw, dynamic condylar screw or other intramedullary devices, Locking compression plate was introduced as a new implant that allows angular stability for the treatment of complex comminuted, osteoporotic and unstable fractures of proximal femur. This is a precontured stainless steel plate specially designed for the left and right femur to accommodate average femoral neck anteversion. In this study we analysed the results of unstable intertrochanteric fractures treated with proximal femoral locked compression plate (PFLCP) as compared with similar patients treated with dynamic hip screw (DHS).
Materials and Methods
A combined prospective and retrospective nonrandomised observational study of unstable intertrochanteric fractures (Type 31- A2.1, 31- A2.2 and 31- A2.3 in AO/ASIF classification) was conducted with one group treated with PFLCP and another with DHS. Prospective arm of 27 patients (31A2.1 - 14, 31A2.2 - 9, 31A2.3 – 4) who were treated with PFLCP was compared retrospectively with a group of 35 patients (31A2.1- 19, 31A2.2 – 11, 31A2.3 – 5) treated with DHS.
This study included the patients presenting to Orthopaedics outpatient clinic and emergency of a tertiary level Hospital in a particular unit with fresh unstable intertrochanteric femoral fractures (from March 2011 to November 2012 in prospective group and between March 2008 to February 2010 in retrospective group. Data for this retrospective group was obtained from the previous study done in the same department evaluating the results of DHS in unstable intertrochanteric fractures during the period mentioned above.
Fresh Unstable intertrochanteric femoral fractures (Type 31-A2.1, 31-A2.2 and 31A2.3 in AO/ASIF classification) were considered eligible for the study. Exclusion criteria were pathological fractures, neglected fractures, fractures associated with polytrauma, previous surgery on the ipsilateral hip or femur, severe concomitant medical condition (grade V on American Society of Anesthesiologist (ASA scale). All the patients included in the study presented within a week of sustaining injury. Background variables including age, sex, ASA risk score, mode of injury and side of involvement were recorded for all patients [Table/Fig-2]. Blood samples were collected in vacutainer tubes and a baseline haemogram, TLC, DLC, blood urea, serum creatinine, and random blood sugar were done in all patients.
| PFLCP | DHS |
|---|
| No. of Patients | 27 | 35 |
| Male: female | 17:10 | 19:16 |
| Mean age (years) | 56.4 | 53.8 |
| Side of injury (left: right) | 15:12 | 20:15 |
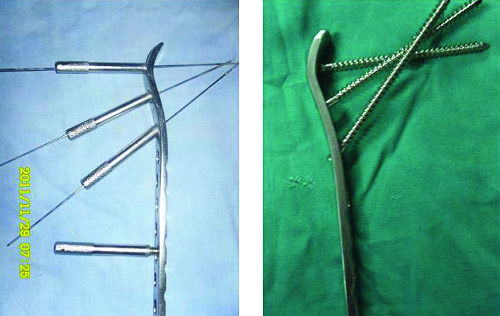
Proximal femoral locked compression plate (PFLCP) is a precontured stainless steel plate specially designed for the left and right femur to accommodate average femoral neck anteversion. The convergent angle design (95°/120°/135°) and the locking interface of the proximal 6.5 mm non-cannulated locking screws should alleviate and improve proximal femoral fixation especially in osteopenic bone. The remaining 4–16 screw holes, in the plate shaft, are LCP combi-holes, which allow the placement of either a cortical or a locking head screw [Table/Fig-3a,b]. This provides the surgeon with the flexibility to achieve plate-to-bone apposition as well as axial compression or angular stability. After achieving closed reduction in most of the cases, plate can be applied by minimally invasive percutaneous plate osteosynthesis (MIPPO) Technique. In another group 135 degree angled dynamic hip screw (DHS) was used for fracture fixation after obtaining close/open reduction.
Picture of the PFLCP showing orientation of the proximal screws for the head of the femur and the distal combi-holes for locking/cortical screws.
Treatment
All operations were done by the first three surgeons. Preoperative intravenous cefoperazone + salbactum (500mg + 500mg) was given in every patient. Spinal anaesthesia was used in both groups. Operations were performed according to the basic protocols for either PFLCP or DHS group. Closed or open reduction of the fracture was obtained on the operating table using usual classical technique.
Closed reduction was performed by gentle longitudinal traction on slightly abducted, externally rotated and extended limb followed by internal rotation to bring the limb in neutral rotational alignment. Only 4 patients (AO type 31 A2. 1 – 3, and AO type 31A2.2 – 1) in PFLCP group needed open reduction when unsatisfactory reduction was observed under fluoroscopic view, MIPPO technique was used for fixation in all cases where closed reduction was achieved in PFLCP group. PFLCP was provisionally fixed to the bone with help of K-wires proximally and distally. Sleeves applied and guide wire passed under fluoroscopic control. Screws were put after assessment of size. DHS fixation was done in usual classical manner. In 26 patients fracture was reduced by close method where nine cases needed open reduction. Out of these nine patients, five were of AO type 31- A2.1, three were of type 31- A2.2 and one was of type 31- A2.3.
Length of incision, close/open reduction, fluoroscopy time, blood loss, operation time and any intraoperative complications were recorded [Table/Fig-4]. Prophylactic postoperative antibiotics were given in all patients. Under the surgeon and physiotherapist guidance patients were encouraged for hip, knee and ankle range of motion exercises on 1st postoperative day. Non weight bearing walk was started on 3rd postoperative day in both groups. In DHS group weight bearing was allowed after 4-6 weeks of operation where as in PFLCP group it was delayed till the radiological evidence of union was seen (on an average by 8-10 weeks postoperatively).
| Variables | PFLCP | DHS | Statistical significance |
|---|
| Length of incision(cm) | 10±2 | 12±3 | 0.003 |
| Operating time (min) | 75±5 | 56±9 | 0.0001 |
| Open reduction (n) | 4 | 9 | 0.3582 |
| Blood Loss (ml) | 300±50 | 500±50 | 0.0001 |
| Blood Transfusion (n) | 25 | 32 | 1.000 |
| Flouroscopy time (min) | 3±5 | 1±2 | 0.0350 |
Follow- Up
Plain anteroposterior and cross table lateral radiographs were obtained on the first postoperative day, and analysed for reduction of fracture and position of implant. Follow-up reviews were performed at 1, 3, 6 and 12 months after surgery and then annually (minimum follow up period was 1 year) and evaluated clinically by Harris hip Score and radiologically for fracture union and any complication related to implant [Table/Fig-5a-b,5c-d5e-f,6a-b,6c-d,6e-f].
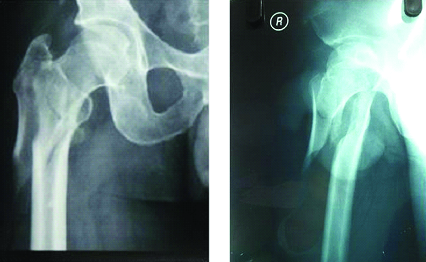
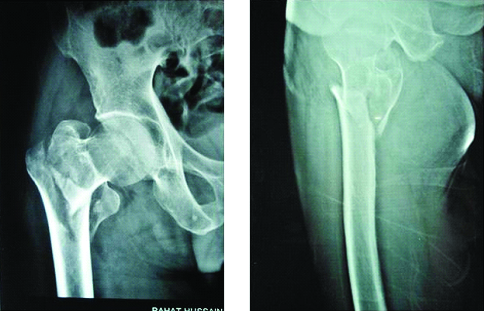
Preoperative radiographs of the hip (AP&Lateral) showing unstable intertrochanteric fracture.
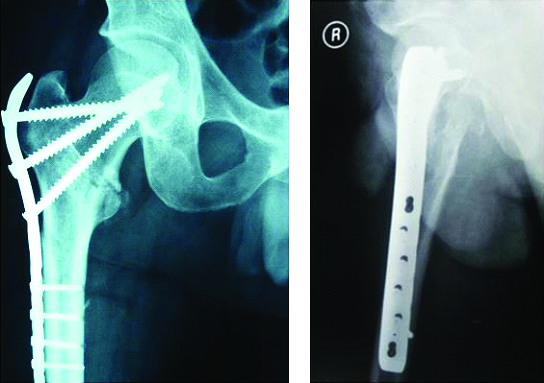
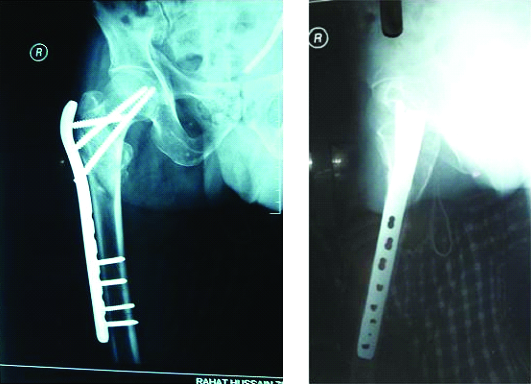
Immediate postoperative radiographs of the hip (AP&Lateral) showing acceptable reduction with maintained neck shaft angle.
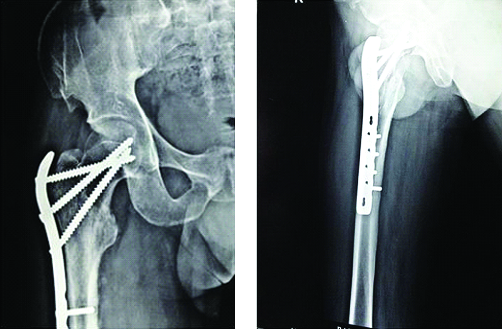
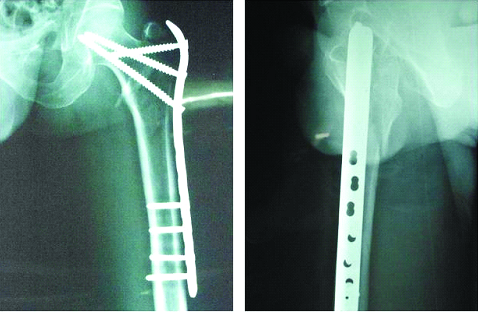
Six months postoperative radiographs showing good union without any change in the neck shaft angle or the position of the implant.
Preoperative radiographs of the hip (AP&Lateral) showing unstable intertrochanteric fracture.
Immediate postoperative radiographs of the hip (AP&Lateral) showing acceptable reduction with maintained neck shaft angle.
Four months postoperative radiographs showing good union without any change in the neck shaft angle or the position of the implant.
At each post-operative review plain anteroposterior and lateral radiographs were obtained. All changes in the position of the fracture and implant (varus collapse, cut out of femoral head screw and medialization of the distal fragment), when compared with the radiograph taken on the first post-operative day, were recorded and considered as secondary measures of outcome. During follow up visits patients were examined regarding certain variables like infection, limb shortening and mobility score [Table/Fig-7].
| Variables | PFLCP | DHS | Statistical significance |
|---|
| Superficial infection | 0 | 0 | NS |
| Deep infection | 1 | 1 | NS |
| Implant Failure/ Breakage of convergent screw | 3 | 0 | NS |
| “Cut Out” of femoral head screw | 0 | 3 | NS |
| Medialization | 0 | 7 | 0.0347 |
| Varus collapse | 3 | 8 | NS |
| Mean shortening of Femur (cm) | 0.18±0.02 | 1± 0.2 | Less than 0.0001 |
| Mean time of mobilization with frame (days) | 3 | 3 | NS |
| Mobility Score (at final follow up) | 5.4±1.4 | 5.6±1.2 | NS |
Statistical Analysis
Statistical analysis was performed using SPSS17. Quantitative variables were analysed using the Student’s t-test and categorical variables were analysed by the χ2 test or Fisher’s exact test where appropriate. The level of statistical significance was set at a two-sided p-value of 0.05.
Results
Among 27 patients (17 males and 10 females, average age 56.4 years, range 42-73 years) treated with PFLCP, one patient expired 6 weeks postoperatively and one patient lost to follow up, so 25 patients were evaluated for final outcome of which 23 (92%) patients showed union at follow up of 12 months. According to Harris hip Score 14 (56%) patients had excellent, 8 (32%) had good, 1 (4%) fair and 2 (8%) patients had poor results. Overall good to excellent result was seen in 22 (88%) cases. One patient developed deep infection which healed after two debridement. Three patients developed either bending of or breakage of proximal screws / convergent screw and so all the three developed varus collapse [Table/Fig-8]. These were the patients who were less compliant and started early weight bearing. This may be the reason for breakage/ bending of the screws leading to varus collapse. These values were not statistically significant as compared to other group.
Six weeks postoperative radiograph showing varus collapse and bending of proximal screws!

Among 35 patients (19 males and 16 females, average age 53.8 years, range 46-78 years) treated with DHS, One developed deep infection which healed after 1st debridement, and three had cut out of femoral head screw. Both the differences were not significant. According to Harris Hip Score excellent result was seen in 9 (25.7%) cases, good in 12 (34.3%), fair in 10 (28.6 %) and poor in 4 (11.4%) cases. Overall good to excellent result was seen in only 21 (60%) patients where as in PFLCP group 88% (22/25) patients had good to excellent results. In seven patients medialization of distal fragment occurred which was statistically significant (p = 0.0347). Varus collapse occurred in eight patients as compared to three in PFLCP group which was statistically not significant. Need for open reduction was even not significant.
Length of incision, operating and fluoroscopy time were favourable in DHS group, but blood loss was less in PFLCP group [Table/Fig-7]. Mean time for mobilization was comparable in both groups.
Discussion
Treatment of Proximal femoral fractures is challenging [11]. The treatment goal is to achieve anatomic reduction with a stable fracture fixation to allow early functional rehabilitation. Over the past decades, intertrochanteric and subtrochanteric fractures were predominantly treated by dynamic hip screw [12]. However, the complication rate for unstable fractures treated with a dynamic hip screw or dynamic condylar screw plate has shown to be as high as 3% to 26% [13]. Primary or secondary varus collapse and hardware failure by “cut-out” of the femoral head screw are the most frequently reported complications [14]. Unstable proximal femoral fractures can be treated by dynamic hip screw or dynamic condylar screw plates but they cannot prevent secondary limb shortening after weight bearing due to lateralization of the neck/head fragment from gliding along the screw or because of distal fragment medialization [15]. Role of intramedullary devices like proximal femoral nail (PFN), gamma nail (GN) and Proximal femoral nail antirotation (PFNA) in the treatment of these unstable intertrochanteric fractures are also controversial with varying results, though they have some theoretical advantage over the DHS. Various authors have shown high complication rate with the use of these implants. Failure rate of gamma nail for the treatment of these fractures ranges from 12.7% to 15% [16,17]. Fogagnolo et al., showed a complication rate of about 23.4% with the use of PFN for the treatment of these unstable fractures [18]. In another study done by Uzun et al., [19] nonunion was seen in 5.7%, secondary varus collapse in 25.7%, cut out of proximal screws in 5.7% and reoperation in 14.3% cases. As for PFNA, Takigami et al., [20] showed complications in 14% of the cases and 4% required reoperation. In another study by Yaozeng et al., intraoperative complications were seen in 20% cases and 9.1% cases had femoral shaft fracture [21]. Comminuted fracture of intertrochanteric region extending into the lateral cortex of femur, intertrochanteric fracture with long subtrochanteric extension, reverse oblique type of fractures, fractures associated with severe osteoporosis are not successfully treated with DHS. The PFLCP seems to be superior to the sliding hip screw because DHS lag screw does not hold the lateral cortex and telescoping of the implant might promote lateralization of the trochanteric fragment leading to varus collapse and shortening [22]. PFLCP provides anatomic reduction, stable fixation and preservation of blood supply. Plate length allows spanning of entire diaphysis in segmental fracture patterns. Biomechanically PFLCP is stronger or equivalent to other fixation methods for fractures of the trochanteric and subtrochanteric region [23].
In the present series size of the incision, operating and fluoroscopy time favoured surgery with DHS. Meanwhile blood loss was significantly more in DHS group. But do these variables really matter when the outcome of surgery is weighed upon. Stunning higher number of cases having varus collapse and “cut-out” of femoral head screw in our study may lead us to reconsider the treatment protocol for unstable intertrochanteric fractures. Intertrochanteric fractures have no problem with getting united. Concern should be to prevent medialization, achievement and maintenance of proper reduction and hence to get as negligible limb length discrepancy as possible. The more bothersome result in our study was statistically significant more cases having medialization of distal fragment in DHS group, and the similar is finding with shortening of operated limb.
Glassner PJ et al., [23] in their study on 10 patients showed 70% failure including 30% with varus collapse, 20% each with breakage of screw and plate when treated with PFLCP as compared to 12% failure rate (varus collapse and screw breakage) in our study. Karl Wieser et al., [22] in their study on 14 patients showed 4 cases with failure when they used PFLCP. In two cases postoperative X rays showed a slight varus malalignment. This inaccurate reduction may predispose implant failure. They concluded in their study that the prerequisite in using the PFLCP in unstable facture pattern, is restricted weight bearing until callus formation is seen. All reported fracture displacement took place in cases where posteromedial buttress was missing and the patients were unreliable in their compliance to limited weight bearing.
We conducted the study on patients admitted on a particular day of a week, to be followed in a particular unit. So this limited the number of patients included in the study. The smaller sample size was the major limiting factor to come upon a strong conclusion. Another weakness of this study is that the groups were not randomized and number of each type of fracture pattern was not same in the two groups. PFLCP represents a feasible alternative for the treatment of unstable intertrochanteric fractures. The weakness of this construct is stress concentration at the junction of the LCP and the proximal locking screws. As compression of trochanteric fragments is not possible, the bending stress at the junction of the plate and the proximal femur increases and may result in breaking of the proximal locking screws close to the plate as it occurred in one of our cases. Proper reduction of the fracture and restriction to early postoperative weight bearing can only prevent complications of PFLCP. Further biomechanical studies are required to assess effectiveness of PFLCP.
Conclusion
The purpose of surgical intervention in treatment of unstable intertrochanteric fractures is stabilization of fracture, early mobilization, restoration of limb length and painless function. This was achieved more satisfactorily with the use of PFLCP than with DHS. At present we consider PFLCP has a good promise for unstable intertrochanteric fractures even though more randomized control trials with higher sample size are needed to support or refute the present work.
Declaration
Present manuscript has been presented in Asia Pacific Orthopaedic Association Conference (APOA 2014) at Pattaya, Thialand and in Indian Orthopaedic Association Conference (IOACON 2014) at Hyderabad, India.