Squamous Cell Carcinoma of the Renal Pelvis, A Rare Site for a Commonly Known Malignancy
Murugappan Nachiappan1, Manjusha Madhusudhan Litake2, Varun Gautam Paravatraj3, Navil Sharma4, Aditya Narasimhan5
1 Assistant Professor, Department of Surgery, BJGMC and Sassoon General Hospitals, Pune, India.
2 Associate Professor, Department of Surgery, BJGMC and Sassoon General Hospitals, Pune, India.
3 Junior Resident, Department of Surgery, BJGMC and Sassoon General Hospitals, Pune, India.
4 Junior Resident, Department of Surgery, BJGMC and Sassoon General Hospitals, Pune, India.
5 Junior Resident, Department of Surgery, BJGMC and Sassoon General Hospitals, Pune, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Murugappan Nachiappan, No 1571/1 2nd Cross 2nd Main Road Nagappa Block Srirampuram Bangalore-560021, India.
E-mail: arun184@gmail.com
Chronic nephrolithiasis predisposes to squamous metaplasia and subsequently SCC which is a rare malignancy of the upper urinary tract. A 60-year-old woman with a long standing history of renal calculi presented with flank pain and fever. Investigations revealed a mass in the superior pole of a non functioning left kidney while the right kidney was sub optimally functioning, hydronephrotic and there was presence of bilateral staghorn calculi. Patient underwent decompression of right kidney by double j stenting and left radical nephrectomy that revealed well differentiated squamous cell carcinoma of renal pelvis. Most SCC of the renal pelvis present with advanced disease and dismal prognosis while our patient presented with localized disease without lymphatic and distant metastasis. Thus radical nephrectomy can be curative if the disease can be diagnosed at an earlier stage. This emphasizes the need of early treatment of nephrolithiasis to prevent the development of SCC and screening of patients with long standing staghorn calculi.
Radical nephrectomy, Squamous cell carcinoma of kidney, Staghorn calculi, Xanthogranulomatous pyelonephritis
Case Report
A 60-year-old female presented with complaints of pain in bilateral flank region over 3 months with an associated history of fever and burning micturition with no history of haematuria. Patient was not a known diabetic. An outside ultrasound report from 2012 suggested the presence of bilateral pelvi-calyceal system calculi with moderate to severe hydronephrosis with associated mobile internal echoes suggestive of pyonephrosis with associated thinning of the renal cortices. Patient did not undergo any treatment for the same. Patient had a plain computed tomography scan of the abdomen and pelvis done in the month of April 2015, which suggested grossly enlarged kidneys with multiple bilateral pelvicalyceal system calculi with the largest calculus on the right side measuring (4.5 *2 *1 cm) and the largest calculus on the left side measuring (3.5 *3 *1.3 cm) with associated gross hydronephrosis on the right side with thinning of the right renal parenchyma. Patient also had large multiple hypodense areas scattered in the left renal parenchyma.
On examination, patient was febrile, with mild tenderness in bilateral renal angles. On investigating the patient further, patient had a serum creatinine value of 2.4, total leucocyte count of 7,900 cells/mm3 and a haemoglobin value of 7mg/dl. Urine routine and microscopy showed presence of a few pus cells, mild albuminuria with no evidence of microscopic haematuria. Culture did not show the growth of any microorganism.
Ultrasound abdomen and pelvis showed a severely enlarged right kidney of size (18*10*9 cm) with severe hydronephrosis secondary to a (4.6*1.5 cm) pelvi-infundibular staghorn calculus with papery thin cortex with evidence of a large echogenic soft tissue mass extending on the medial aspect involving the retroperitoneum. Left kidney was also found to be severely enlarged size (19*12*8 cm) and hydronephrotic with a (4*1.6 cm) pelvi-infundibular staghorn calculus with a cortical thickness of (1-2)mm and a large heterogenous lobulated mixed solid cystic soft tissue mass of size (9*6 cm) on the antero medial aspect. Cystic spaces showed polypoidal wall projections with mild vascularity with parenchymal extension and retroperitoneal infiltration. There was an evidence of a large echogenic soft tissue mass extending on the medial aspect involving the retroperitoneum. Left renal vein and IVC were free of the mass. Right ureter was found to be dilated in the upper and mid regions secondary to a stricture in the lower third 2 cm proximal the right uretero- vesical junction.
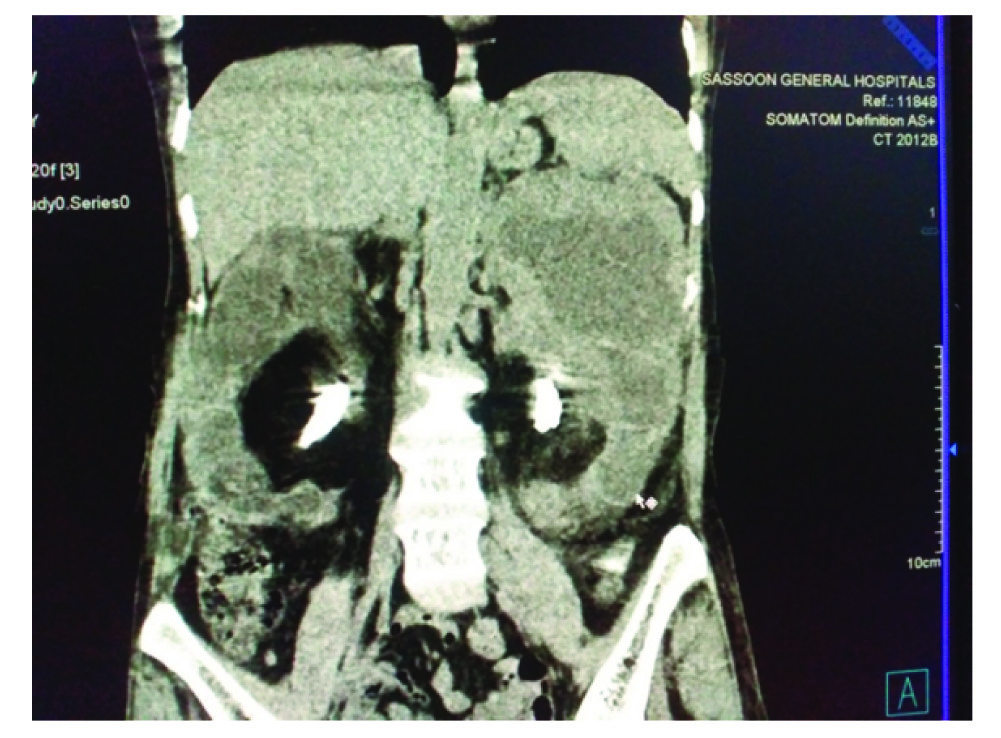
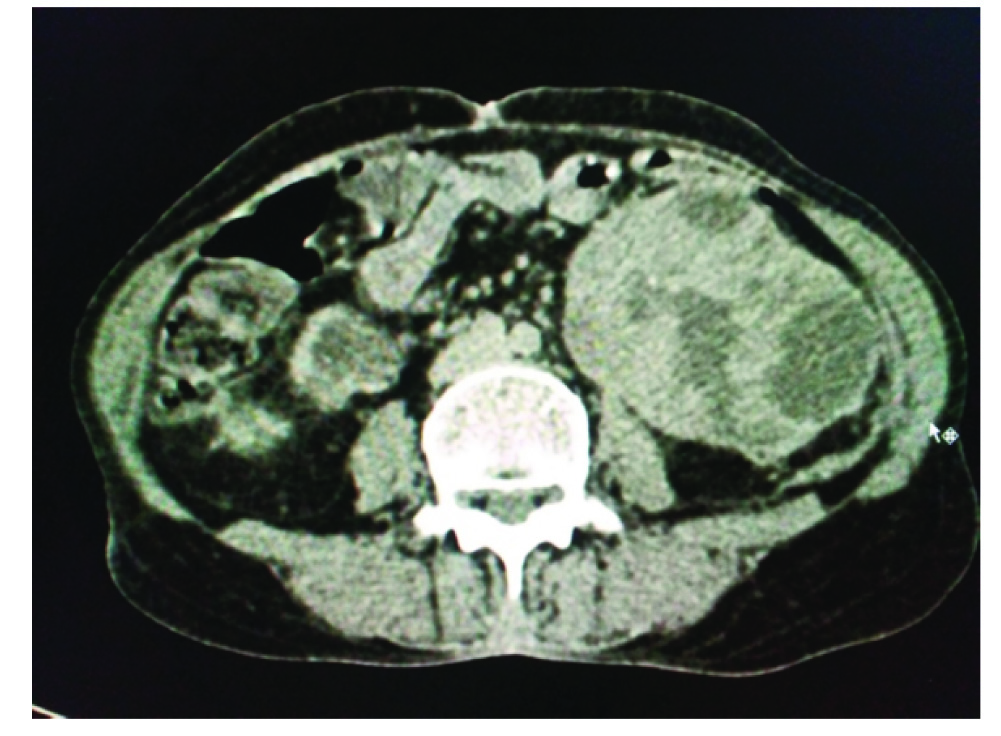
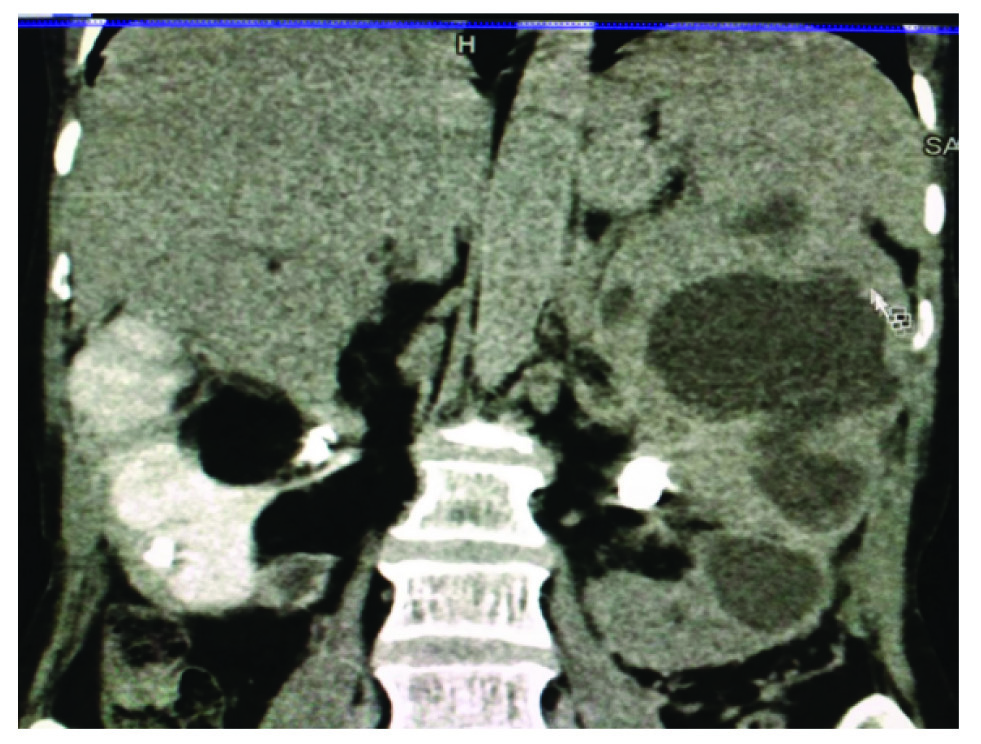
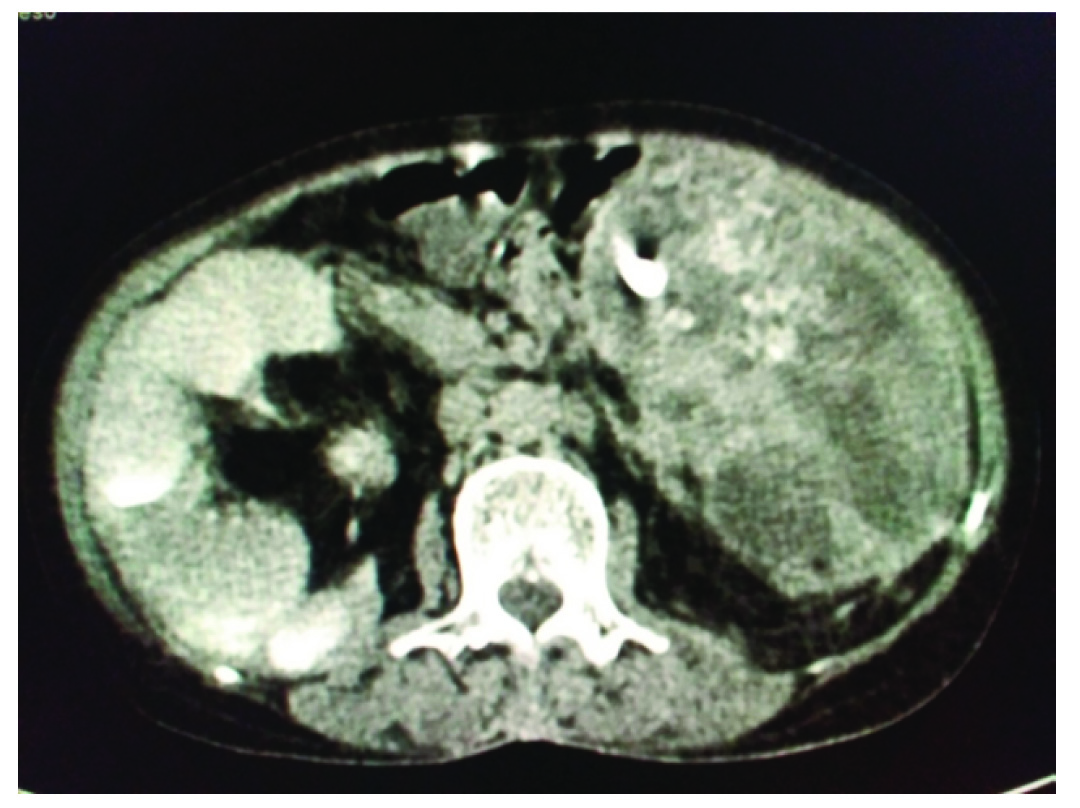
With a suspicion of xantho-granulomatous pyelonephritis and a left renal mass with bilateral staghorn calculi, the patient underwent a CT Urography which confirmed the findings of the ultrasound. There was a well defined partially exophytic complex cystic lesion in the upper pole of the left kidney with few septae and calcifications within and an eccentrically located soft tissue mass [Table/Fig-1,2]. There was evidence of a few enlarged left renal hilar lymph nodes with the largest measuring 1.1 cm. Left kidney did not show excretion of contrast even on delayed scans [Table/Fig-3,4].
Coronal view showing well defined partially exophytic complex cystic lesion in the upper pole of the left kidney with few septae and calcifications within and an eccentrically located soft tissue mass with bilateral staghorn calculi.
Axial view showing complex cystic lesion of the left kidney with few septae
Coronal view showing no contrast excretion by the left kidney
Axial view showing the presence of the dye in the right kidney and the left kidney with no contrast excretion. Also, seen is the part of the staghorn calculi in the pelvis.
DTPA scan done to assess bilateral kidney function in view of no excretion of the contrast of the left kidney was suggestive of an optimally functioning obstructed right kidney and a negligibly functioning left kidney with a total GFR of 47.1 ml per minute.
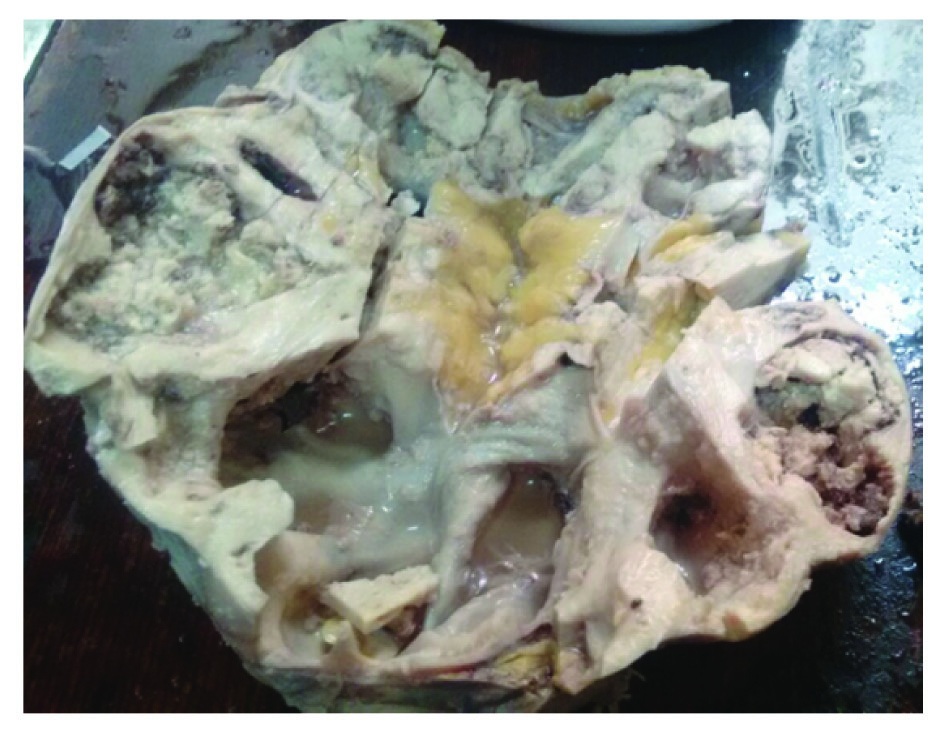
Patient underwent insertion of a double J stent in the right kidney. Patient’s serum creatinine value reduced to 1.4. In view of suspicion of malignancy of the left kidney, patient underwent a left radical nephrectomy, the procedure was uneventful with no immediate postoperative complications. On gross examination, the specimen was found to be enlarged with a nodular surface covered with perinephric fat measuring (20*15*5 cm). On gross section the entire kidney was replaced by a mass in the upper pole and large dilated cystic areas in the lower and mid portions. Mass was whitish grey and measured (6*6*5 cm) showing large areas of necrosis and haemorrhages with a variegated appearance [Table/Fig-5]. Cut open specimen also showed the presence of multiple calculi. Para- aortic lymph nodes identified with the largest measuring (1.5*1*0.5 cm). There was no involvement of the perinephric fat and the adrenal gland by the tumour.
Showing entire kidney replaced by a mass in the upper pole and large dilated cystic areas in the lower and mid portions.
Microscopic evaluation revealed tumour tissue composed of large, round to polygonal cells with pleomorphic and hyperchromatic nuclei arranged in cords and sheets. Many keratin pearls seen. Areas of calcification and vascular emboli were noted suggestive of well to moderately differentiated squamous cell carcinoma of the kidney [Table/Fig-6]. Multiple sections through different areas of the kidney revealed no normal renal tissue. Para-aortic lymph nodes were found to be free of the tumour. Patient has been planned for adjuvant cisplatin based chemotherapy.
Showing large, round to polygonal cells arranged in cords and sheets. Many keratin pearls seen.

Discussion
In the upper urinary tract system, transitional cell carcinoma is the more common type of malignancy arising from the renal pelvis, whereas squamous cell carcinoma is uncommon with a reported incidence of only 0.5 -0.8% [1,2]. It is aggressive with high grade at the time of presentation and have a poor prognosis when compared to the other upper urinary tract malignancies [3]. As in other organs, it is believed that chronic irritation, inflammation and infection lead to a squamous metaplastic change in the urothelium of the renal collecting system, which may progress to dysplasia and further to carcinoma sequentially in some patients. It is not clear as to whether squamous metaplasia is the cause or the effect with regards to staghorn calculi [4–6]. While according to some authors it is assumed that the process begins with urothelial metaplasia secondary to chronic irritation, leading to further dedifferentiation, dysplasias and ultimately to a SCC [7]. Thus the pertinent medical history include chronic episodes of pyelonephritis or nephrolithiasis [8,9].
Primary SCC has a slight female preponderance with the most common age group of presentation being 50-70 years. SCC of kidney are similar to other SCCs histopathologically, consisting of keratin pearls and keratotic cellular debris. The radiologic findings of SCC of kidney may vary from a solid mass with hydronephrosis and calcifications, an infiltrative lesion without evidence of distinct margins, a non functioning kidney with renal calculi, to a low density mass in the renal parenchyma with perirenal invasion. The differential diagnosis on basis of radiological investigations include primary and secondary renal neoplasms and xanthogranulomatous pyelonephritis (XGP) associated with renal calculi. XGP is a rare form of chronic pyelonephritis, commonly occurring as a result of chronic obstructive calculi with hydronephrosis with destroyed renal parenchyma. XGP rarely leads to keratinizing squamous metaplasia which closely mimics neoplasm, leading to misdiagnosis of malignancy [9].
In our case there was a well defined partially exophytic complex cystic lesion in the upper pole of the left kidney and an eccentrically located soft tissue mass in a known case of long standing staghorn calculi making the distinction of XGP difficult.
MRI findings of SCC of kidney have been rarely described in the literature, in the few times it has been mentioned, found to be non specific [10]. The non-specific clinical and radiologic features in renal SCC may cause diagnostic confusion and histopathology confirmation is needed [11,12].
Patients with a long standing history of renal calculi and an associated poor functioning kidney or hematuria require an investigation such as CT for the screening of malignancy as reported by Raghavendran et al [13]. A study by Lee et al., found that an enhancing extra luminal and exophytic mass, and sometimes an intraluminal component were two of the most useful features on CT imaging of renal SCC [14]. Further it was suggested that for every patient with renal stone should undergo screening intravenous urography (IVU) periodically, especially, in those patients that present with a history of long standing stones, to check for the split function test for all portions of renal parenchyma. This was advised based on the observation that presence of filling defects, delayed excretion of the dye, or parenchymal thickening in IVU may indicate a renal tumour despite the absence of a solid mass and preservation of renal contour, thus warranting further investigations.
It is essential to rule out metastatic SCC of the by using a combination of clinical history, imaging, and histopathology. In order to label it as primary SCC of renal parenchyma, it is necessary to rule out metastasis from other organs, the other essential finding being normal histopathological findings of the renal pelvis despite other findings as there may exist the possibility of an occult primary SCC somewhere else.
Renal SCC usually presents at an advanced stage-pT3 or higher. Surgery is the mainstay of treatment in SCC of renal pelvis. Adjuvant treatments have marginal benefit. Because of advanced stage at presentation, the prognosis is generally poor, as surgical resection is rarely curative and adjuvant chemoradiotherapy is usually ineffective. The prognosis is dismal with a 5-year survival rate of less than 10% [2,7,12].
The staging is determined by the extent of invasion by the primary tumour and by microscopic evaluation of the regional lymph nodes and radiological evaluation for distant metastasis. In the present case the patient presented with localized disease with no involvement of peri renal tissue and with no evidence of distant metastasis and regional lymph node disease indicating the radical nephrectomy can be curative if the disease is diagnosed at an earlier stage further emphasizing the need for prompt treatment of nephrolithiasis and screening of patients with long standing staghorn calculi.
Conclusion
SCC of renal pelvis is an aggressive disease, presenting with a higher grade and thus have dismal prognosis as the only effective management which is surgery cannot provide cure. Our patient presented with localized disease without regional nodal or distant spread indicating that a radical nephrectomy can achieve R0 resection and can be curative if the disease is diagnosed early. This outlines the importance of keeping this diagnosis in the back of the mind while dealing with patients of chronic renal calculi and also emphasizes the need for prompt management of patients with renal calculi even when they are non obstructive by nature to prevent secondary changes due to chronic irritation.
[1]. Odabas O, Karakok M, Yilmaz Y, Atilla MK, Akman E, Aydin S, Squamous cell carcinoma of kidneyEastern Journal of Medicine 2000 5:35-56. [Google Scholar]
[2]. Kalayci OT, Bozdag Z, Sonmezgoz F, Sahin N, Squamous Cell Carcinoma of the Renal Pelvis Associated with Kidney Stones: Radiologic Imaging Features with Gross and Histopathological CorrelationJournal of Clinical Imaging Science 2013 3:14doi:10.4103/2156-7514.109741 [Google Scholar]
[3]. Berz D, Rizack T, Weitzen S, Mega A, Renzulli J, Colvin G, Survival of patients with squamous cell malignancies of the upper urinary tractClin Med Insights Oncol 2012 6:11-18. [Google Scholar]
[4]. Li MK, Cheung WL, Squamous cell carcinoma of the renal pelvisJ Urol 1987 138:269-71. [Google Scholar]
[5]. Holmäng S, Lele SM, Johansson SL, Squamous cell carcinoma of the renal pelvis and ureter: Incidence, symptoms, treatment and outcomeJ Urol 2007 178:51-56. [Google Scholar]
[6]. Tyagi N, Sharma S, Tyagi SP, A histomorphologic and ultrastructural study of the malignant tumours of the renal pelvisJournal of Postgraduate Medicine 1993 39(4):197-201. [Google Scholar]
[7]. Mardi K, Kaushal V, Sharma V, Rare co-existence of keratinizing squamous cell carcinoma with xanthogranulomatous pyelonephritis in the same kidney: Report of two casesJ Cancer Res Ther 2010 6:339-41. [Google Scholar]
[8]. Jain A, Mittal D, Jindal A, Incidentally detected squamous cell carcinoma of renal pelvis in patients with staghorn calculi: case series with review of the literatureISRN Oncology 2011 2011:6205746 pages [Google Scholar]
[9]. Talwar N, Dargan P, Arora MP, Sharma A, Sen AK, Primary squamous cell carcinoma of the renal pelvis masquerading as pyonephrosis: a case reportIndian Journal of Pathology and Microbiology 2006 49(3):418-20. [Google Scholar]
[10]. Imbriaco M, Iodice D, Erra P, Terlizzi A, Di Carlo R, Di Vito C, Squamous cell carcinoma within a horseshoe kidney with associated renal stones detected by computed tomography and magnetic resonance imagingUrology 2011 78:54-5. [Google Scholar]
[11]. Karabulut A, Emir L, Gonultas M, Incel N, Germiyanoglu C, Erol D, Squamous cell carcinoma located in the renal caliceal system: A case report and review of the literatureTurk J Cancer 2002 32:20-24. [Google Scholar]
[12]. Bhaijee F, Squamous cell carcinoma of the renal pelvisAnn Diagn Pathol 2012 16:124-27. [Google Scholar]
[13]. Raghavendran M, Rastogi A, Dubey D, Chaudhary H, Kumar A, Srivastava A, Stones associated renal pelvic malignanciesIndian J Cancer 2003 40:108-12. [Google Scholar]
[14]. Lee TY, Ko SF, Wan YL, Cheng YF, Yang BY, Huang DL, Renal squamous cell carcinoma: CT findings and clinical significanceAbdom Imaging 1998 23:203-08. [Google Scholar]