A Case of Metastatic Esophageal Carcinoma in a Pregnant Woman with Radiologic Findings
Zülküf Akdemir1, Erbil Karaman2, Harun Arslan3, Iskan Çalli4, Hüseyin Akdeniz5
1 Medical Doctor, Department of Radiology, Van Training and Research Hospital, Van, Turkey.
2 Assistant Professor, Department of Obstetric and Gynecology, Yuzuncu Yil University, School of Medicine, Van, Turkey.
3 Assistant Professor, Department of Radiology, Yuzuncu Yil University, School of Medicine, Van, Turkey.
4 Medical Doctor, Department of General Surgery, Van Training and Research Hospital, Van, Turkey.
5 Medical Doctor, Department of Radiology, Van Private Lokman Hekim Hospital, Van, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Erbil Karaman, Assistant Professor, Hafiziye Mahallesi Iki Nisan Caddesi, Efes Sitesi A Blok No:9 Ipekyolu, Van, Turkey.
E-mail: erbil84@gmail.com
The incidence of all malignant tumours during pregnancy is extremely rare and esophageal carcinoma ranges from 0.07 to 0.1% of all malignant neoplasms. The physiological changes during pregnancy frequently mask the complaints and symptoms related to the disease. The physical and physiological clinical conditions limit the diagnostic approaches. Therefore, the stage of cancer at the time of diagnosis is usually advanced. The management with cancer surgery and chemotherapy regimens must be modified in pregnant women in order to minimize fetal and maternal risks. Here, we report a very rare case of metastatic esophagus cancer in a 39-year-old woman with 28 weeks of pregnancy and aim to show the ultrasound (USG) and magnetic resonance imaging (MRI) findings with treatment and follow up management.
Esophageal cancer, Magnetic resonance imaging, Pregnancy, Ultrasound
Case Report
A 39-year-old gravida 5 parity 4 patient at 28 weeks of gestation presented to the outpatient department with complaints of difficulty of swallowing liquid and solid foods, body weight loss, bleeding from mouth and vomiting. She had no history for cesarean delivery. On detailed history, it was noted that the patient was hospitalized in her thirteenth weeks of pregnancy due to resistant hyperemesis gravidarum and had some relief with conservative treatment but did not accept the requested endoscopy procedure and she was discharged. Then, she was not followed properly due to her inconsistency. On obstetric examination, a singleton intrauterine live fetus with growth corresponsing to 28 weeks of gestation consistent with last menstrual period was noted. No pathology regarding fetus or placenta were seen. The body mass index of the patient was 17. The body mass index of the patient in first trimester of pregnancy was 19. She was referred to a gastroenterologist and planned for endoscopy. The upper gastrointestinal endoscopy revealed an ulcerovegetan mass causing significant narrowing of the lumen noted at 25th cm of esophagus from incisors. The endoscope was not forwarded to stomach due to the risk of bleeding and obstruction.
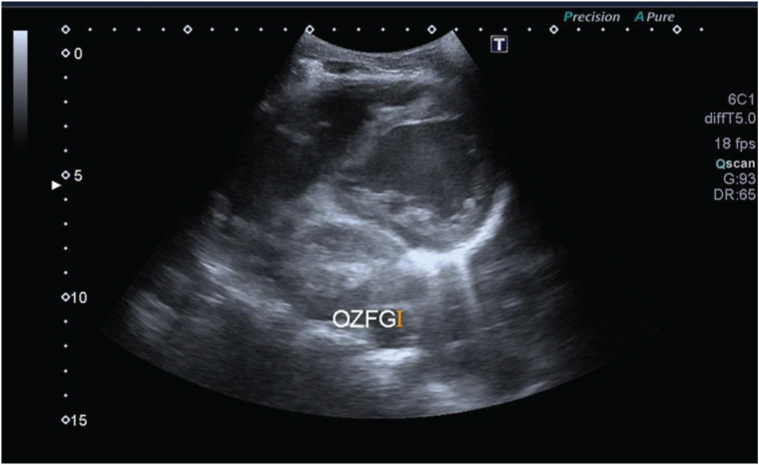
An abdominal ultrasound was performed and it revealed approximately 1.8 cm wall thickening at cardioesophageal junction and lymphadenopathies in gastrohepatic ligament were seen. Also, irregular wall thickening through the distance from mitral valve level to cardioesophageal junction was seen in view of investigation from intercostal margin [Table/Fig-1].
An abdominal sonogram shows approximately 1.8 cm irregular wall thickening at cardioaesophageal junction
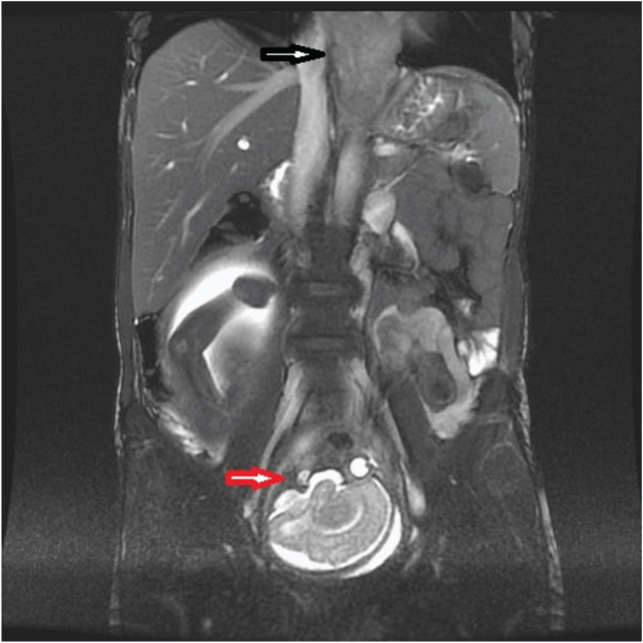
The thorax and abdominal MR imaging showed circumferential wall thickening involving mid-lower thoracic aesophageal segment and extending to cardioesophageal junction, lymphadenopathies on gastrohepatic ligament and suspected metastatic lesions on vertebral corpus [Table/Fig-2]. Biopsy from the mass had findings suggestive of squamous cell carcinoma of esophagus with moderate differentiation. Tube jejunostomy was applied for enteral feeding. Conservative management was decided due to the prematurity of fetus until the lung maturation was occurred. Two doses of betamethasone at 12 hours interval were given intramuscularly to the patient against the possibility of preterm delivery or worsening of maternal condition. Early termination may be done in the case of instability of mother’s health. The patient delivered 2650 gram female baby at 34th week of gestation via C- section, due to the breech presentation. No adverse events of maternal clinical situation was seen in postoperative period. The patient was advised to take neoadjuvant chemotherapy in postpartum period after evaluation in gastrointestinal cancer council but the patient didn’t accept the treatment and left the hospital without permission.
Thorax and abdominal MR imaging shows circumferential wall thickening involving mid-lower thoraxic aesophageal segment and extending to cardioaesophageal junction (black arrow) and intrauterin brain image of the viable fetus (red arrow) at the same image
Discussion
Esophageal cancer is one of the leading cause of cancer-related death worldwide [1]. The complete resection of esophageal cancer tissue with surrounding malignant lymph nodes is the sole potential curative treatment. Preoperative staging is very important to determine the appropriate treatment modalities for patient. So this would prevent unneccesary surgical operations and provides facility to make neoadjuvant chemoradiotherapy/chemotherapy when neccesary. Computed tomography is the first advised imaging technique for the evaluation of extent of disease and/or staging after the pathologic examination. It excludes the unresectability and distant organ metastasis [2]. It is reported that endoscopic ultrasonography is the best modality that shows the depth of tumour invasion and involvement of regional lymph nodes [2].
The role of MRI in esophageal tumour evaluation and real-time guidance for radiotherapy (RT) have not been clearly reported, so far. It has been reported that MRI might be valuable in predicting the poor response to the treatment and disease prognosis [2,3]. There is somewhat limited data regarding the role of MRI in esophageal cancer. Hovewer, the use of MRI in aesophageal cancer is continously improving. The cancer care needs an individual assesment to improve the response, an optimised TN-staging and radiotherapy planning. It is reported that MRI potentially complements the limitations of other imaging strategies regarding these points [3].
Esophageal cancer is seen very rarely during pregnancy [4,5]. The symptoms are usually misinterpereted as pregnancy related symptoms. Consequently the diagnosis is delayed and patient admits to hospital in advanced stages. The practical guidelines for treatment of gastric or intestinal cancer during pregnancy are available while there is limited data about esophageal cancer during pregnancy [6,7]. Ueo et al., reported that the guidelines regarding the treatment of aesophageal cancer are similar to those of gastric cancer during pregnancy [6]. The main determinants in the treatment of esophageal cancer during pregnancy are gestational weeks of pregnancy and stage of cancer. Ueo et al., developed treatment guidelines for gastric cancer during pregnancy [6]. When the gastric cancer is diagnosed before 24 weeks of pregnancy, the surgical treatment is recommended but the treatment changes according to the stage of the tumour if diagnosed between 25 and 29 weeks. If the tumour is resectable with locally advanced extention, the emergentcy surgery for the cancer is recommended despite risk for the fetus. If the gastric cancer diagnosed at early stage, the treatment may be postponed in order to provide greater probability of survival of neonate. If diagnosed beyond 30th week of gestation, delivery is recommended if fetus is viable and then radical resection of the gastric cancer is performed [6].
As far as we know from literature, there is only 3 case reports with esophageal cancer in pregnancy until now. The first case was reported by Sharma JB et al., at 2008 of a 36-year-old patient who was 29 weeks of pregnancy and was diagnosed with adenocarcinoma [4]. This case delivery was done at 34th weeks via cesarean section and planned for surgery but patient she underwent radiotherapy due to unresectable tumour. The second case by Al-Githmi in 2009 was of a 29-year-old, 29 weeks of pregnant woman with advanced stage esophagus carcinoma and this case was oriented for palliative treatment [5]. The third case was a 27-year-old woman with history of previous esophagus carcinoma and who had complete remission after chemoradiotherapy, then became pregnant and she had dysphagia at 26th weeks and was diagnosed with reccurent esophagus cancer. This patient was also treated with chemoradiotherapy and tube gastrostomia for dysphagia [8]. Our case was of 39-year-old and diagnosed at 28th weeks of pregnancy with complaints of dysphagia, weight loss and hematemesis. We could mark the similarity regarding the gestational weeks of these patients in literature. The symptoms like vomiting, nausea and weight loss during first trimester of pregnancy are usually encountered and these symptoms may obscure the disease. Also, uterus fundus arises to umblicus level around the 20th weeks of gestation and stomach is pushed upward towards the diaphragm so the symptoms become severe and this compel the patients to report and thus, are finally diagnosed. When we analaysed the detailed history of our case, we saw that the patient was hospitalized in her thirteenth week of pregnancy due to resistant hyperemesis gravidarum and had some relief with conservative treatment but did not accept the requested endoscopy procedure.
Conclusion
Owing to limited number of cases and no standardized guidelines if the literature, such cases presenting to oncology centers should include obstetrician in the multidisciplinary team besides medical oncologist, oncosurgeon, gynaec-oncologist, and radiation oncologist as each case would require individualized approach for the management of the patient. Besides, the gastrointestinal complaints during pregnancy should be looked at suspiciously and especially in resistant case, as in our case, malignancy should be kept in mind and further investigations should be done. Because since the diagnosis becomes difficult the cancer is diagnosed in advanced stage as pregnancy progresses.
Patient consent: The patient gave consent for the case and images.
[1]. Pavlidis N, Coexistence of pregnancy and malignancyOncologist 2002 7:279-87. [Google Scholar]
[2]. Kim TJ, Kim HY, Lee KW, Kim MS, Multimodality Assessment of Aesophageal Cancer: Preoperative Staging and Monitoring of Response to TherapyRadio Graphics 2009 29:403-21. [Google Scholar]
[3]. Van Rossum PS, Van Hillegersberg R, Lever FM, Lips IM, Van Lier AL, Meijer GJ, Imaging strategies in the management of oaesophageal cancer: what’s the role of MRI?Eur Radiol 2013 23(7):1753-65. [Google Scholar]
[4]. Sharma JB, Gupta P, Kumar S, Roy KK, Melhotra N, Challopadhyay TK, Aesophageal carcinoma during pregnancy: A case reportArch Gynecol Obstet 2008 279:401-02. [Google Scholar]
[5]. Al-Githmi I, Aesophageal cancer associated with pregnancyJ Obstet Gynaecol Can 2009 31(8):730-31. [Google Scholar]
[6]. Ueo H, Matsuaka H, Tamura S, Prognosis in gastric cancer associated with pregnancyWorld J Surg 1991 15:293-97. [Google Scholar]
[7]. Saif MW, Management of colorectal cancer in pregnancy: a multimodality approachClin Colorectal Cancer 2005 5:247-56. [Google Scholar]
[8]. Jain Akhil P, Patel Apurva A, Anand Asha S, Shah Sandip A, Aesophageal Carcinoma in PregnancyThe Journal of Obstetrics and Gynecology of India 2014 64(Suppl 1):53-54. [Google Scholar]