Introduction
Extraction of third molars accounts for a large volume of cases and the most frequent intervention in contemporary oral surgical practice [1,2]. There is an acute inflammatory response due to the surgical procedure [3] which is often associated with significant deterioration in oral health related quality of life (physical, social and psychological) in the immediate postoperative period, particularly during the first five days [4].
Prolonged periods of pain and inflammation are mediated by release of local prostaglandins [5]. Postoperative oedema is the consequence of surgical procedures, which involve the raising of muscular attachments, and direct trauma to blood and lymph vessels. This condition represents fluid accumulation in the interstitial area due to transudation from the injured blood vessels and fibrin obstruction of lymph drainage [6].
Third molar surgery is often accompanied by pain and oedema of varying degrees and many pharmacological agents are used to alleviate these symptoms. The most common being anti inflammatory steroids, the ideal requisite would be a drug that can alleviate pain, swelling and oedema while causing minimal drug interaction and adverse effects [7].
Currently, surgeons attempt to avoid patient’s postsurgical unease, by administration of corticosteroids [5,8], analgesics [9], anti-inflammatory drugs [10], enzyme preparations [11], cold packs [7], low level laser therapy [12] to name a few. Recently, the drug Tranexamic Acid (TXA) has also proven to be a reliable haemostatic agent in controlling postsurgical bleeding [13]. Although some of these agents have been proven efficient in management of postoperative pain and oedema [14–16], adverse effects and associated morbidity still pose a serious problem [17,18]. Hence, the clinician’s quest for a superior drug is still on.
Aprotinin a naturally occurring protease inhibitor isolated from bovine lung tissue, containing 58 amino acid residues, inhibits mainly the trypsin like enzymes including those concerned with the formation of certain mediators of acute inflammation [11,19]. Initially named "kallikrein inactivator", aprotinin was first isolated from cow parotid glands in 1928 by Kraut et al., [20].
Aprotinin indirectly inhibits bradykinin, inactivates plasmin, a proteolytic enzyme responsible for digesting fibrin and other plasma proteins. It activates the potent anaphylotoxin C3a in the complement cascade [21,22]. Thus, reduces bleeding after surgeries. Aprotinin has also been used in haemorrhagic shock, fibrinolysis, obstetric and gynecological disorders, urological surgery, and neurosurgery.
Pharmacodynamics: Aprotinin is a broad spectrum protease inhibitor which modulates the systemic inflammatory response associated with surgery. Systemic inflammatory response results in the interrelated activation of the haemostatic, fibrinolytic, cellular and humoral inflammatory systems. Aprotinin, through its inhibition of multiple mediators (e.g., kallikrein, plasmin) results in the attenuation of inflammatory responses, fibrinolysis, and thrombin generation [23].
Aprotinin inhibits pro-inflammatory cytokine release and maintains glycoprotein homeostasis. In platelets, aprotinin reduces glycoprotein loss (e.g., GpIb, GpIIb/IIIa), while in granulocytes it prevents the expression of pro-inflammatory adhesive glycoproteins (e.g., CD11b) [24].
Aprotinin acts as a potent inhibitor of serine proteases. These include: human trypsin, plasmin, plasma kallikrien and tissue kallikrien by forming reversible stoichiometric enzyme inhibitor complexes. The inhibitory effect of aprotinin is due to formation of aprotinin-proteinase complexes by the active serine site of enzyme. It not only binds to the isolated enzymes but also to enzymes already complexed by a third binding partner provided there is still free access to the active site of the enzyme. Thus aprotinin efficiently inhibit free plasmin and plasmin streptokinase complex, which is an intermediate in plasminogen activation formed during thrombolytic therapy with streptokinase [24].
Absorption, distribution and excretion: After 24 hour I.V. infusion of aprotinin at a dosage of 250,000 KIU/ hour (35 mg) a constant plasma concentration of 40-50 KIU/ml is obtained in patients. Following intravenous administration of aprotinin rapid distribution occurs throughout the extracellular compartment. Under normal conditions, aprotinin does not cross the blood brain barrier. Aprotinin is metabolized to shorter peptides or amino acids by lysosomal activity in the liver and kidneys. Unchanged aprotinin excreted in urine, a biphasic elimination pattern with an initial half-life of 0.7 hours and terminal half-life seven hours is observed.
Pharmacological Properties
1. Anti-inflammatory action: Aprotinin inhibits the kinin generation and activation of complement system through enzyme kallikrein, thus acts as a potent anti-inflammatory agent.
2. Analgesic effect: Bradykinin, is 10 times more potent as a vasodilator than histamin, and causes intense pain when applied to tissue. Since bradykinin is dependent on kallikrein for its activation, aprotinin inhibits this mediator.
3. Haemostatic effect: Plasmin which is responsible for the degradation of fibrin is inhibited by aprotinin. Aprotinin also prevents prolongation of bleeding time suggesting that platelet function is preserved. This platelet preservation effect is due to reduced thrombin generation, reservation of platelet adhesive receptor, reduced thromboxane A2 release and prevention of heparin-induced platelet dysfunction.
Indications and Usage: Haemostatic, reduces postoperative pain, anti-inflammatory, anti-thrombolytic and controls hyper fibrinolytic haemorrhage.
Contraindications: Patients with known hypersensitivity to the drug, pregnancy, lactation and renal dysfunction.
Adverse Reactions: Anaphylactic reaction.
Dosage: The dose being 10,000 and 10,00,000 KIU. The potency of aprotinin is given in units; one unit is the amount that activaties 0.5 μg (micrograms) of trypsin; it corresponds to 0.14 μg of pure aprotinin. It is supplied as a clear, colourless, sterile isotonic solution for intravenous administration. Each milliliter contains 10,000 KIU i.e. 1.4 mg of aprotinin per 1 ml of isotonic saline.
Drug Interactions: Aprotinin is physically incompatible invitro with corticosteroids, heparin, tetracycline, nutrient solutions containing amino acids or fat emulsions. Therefore, concomitant administration of aprotinin with another drug should be accomplished by using separate intravenous lines.
Based on the above known properties and advantages of the drug the present study aimed at assessing the effectiveness of this polypeptide, aprotinin in plummeting postsurgical pain and swelling, in patients undergoing surgical removal of impacted lower third molars under local anaesthesia.
Materials ans Methods
A total of 30 systemically healthy adult patients, male and female between the age group of 16-35 years were selected for this double blind randomized clinical trial. This study was conducted in the Department of Oral & Maxillofacial Surgery, KLES Institute of Dental Sciences, Belgaum for a period of six months, from May 2008 to October 2008. The patients were selected randomly from the outpatient department based on the following criteria.
Inclusion criteria
1. Patients requiring extraction of bilaterally impacted lower third molars with similar degree of impactions (moderate to difficult).
2. Male and female patients, age ranging from 16-35 years.
3. Class II position B impaction based on radiographs (Pell and Gregory’s classification).
4. Patients without any infection, pain and inflammation at the site of operation one week before the procedure.
5. Patients with any symptoms of pre-op infection were treated with antibiotics and then taken up for surgery once the infection was under control.
Exclusion criteria
1. Patients with systemic diseases, pregnancy and breast-feeding.
2. Patients taking any medications that could interfere with the healing process.
3. Patients under any antibiotic regimen or taking anti inflammatory drugs within the one week period before the procedure.
4. Patients who exhibited any hypersensitivity to the drug aprotinin.
All patients were explained the details about the surgical procedure and the possible complications associated with the same. A written consent accordingly was obtained from all the patients before the surgery was carried out. The study was approved by the institutional ethical committee board.
The selected 30 patients were undertaken for surgical removal of impacted third molar on both the sides simultaneously.
Preoperative assessment
A general medical history was recorded following which the clinical examination was done. Following which measurements for pain and swelling were carried out.
Postoperative pain
Postoperative pain was assessed using the (Verbal Pain Intensity Scale) [25], which measures pain verbally and a numeric value was attached to each, 0 = No pain; 1= Mild pain; 2 = Moderate pain; 3 = Severe pain; 4 = Very severe pain; 5 = Worst possible pain. Mean readings were taken at each 1st, 2nd, and 7th Postoperative days [Table/Fig-1].
Clinical assessment of facial swelling on aprotinin and control side. Right side was control and left was Aprotinin: a) Aprotinin injection; b) Swelling measurement; c) Pre operative; d) Swelling 1st day Postoperatively; e) Swelling 2nd day Postoperative; f) Swelling 7th day post op.

Measurement of swelling
Patients were asked to keep the neck straight and sit in a relaxed position on the dental chair and look straight. Swelling was measured by drawing lines from angle of the mandible to 5 various points viz: (1) Tragus of ear; (2) Lateral canthus of eye; (3) Alae of nose; (4) Corner of mouth; (5) Menton on both sides of the patient on the 1st, 2nd, and 7th Postoperative days [26] [Table/Fig-1b]. The preoperative readings for each patient were taken as the standard values. The statistical significance was analysed using Student t-test.
Surgical Procedure and Medications
All patients in the study routinely received a prophylactic antibiotic (1 g Amoxicillin), 1 hour prior to the surgery. Multi vial bottle containing 50ml of the solution, each milliliter containing 10,000 KIU of aprotinin in saline was used for the study [Table/Fig-1a]. A test dose for aprotinin was first administered subcutaneously on the ventral surface of right forearm, marked and looked for any hypersensitivity reaction. Once no signs and symptoms were ascertained, the patients were asked to pick one out of two chits which decided the study side for that individual.
On the basis of this random selection, five minutes before commencement of the surgical procedure the study side was submucosally infiltrated with 1ml of 10,000 KIU/ml injection aprotinin in isotonic saline around the surgical site as follows. 0.3 ml submucosally each in lingual and buccal area followed by 0.4 ml in the retromolar area in systematic divided doses. The contra lateral side was infiltrated with 1ml of isotonic saline in the same manner. This was done before obtaining local anaesthesia [Table/Fig-2].
Depicting the intra oral peri apical radiographs and clinical site of injection of aprotinin: a) Periapical radiograph of lower right impacted third molar(48); b) Periapical radiograph of lower left impacted third molar (38); c) Submucousal injection of saline on right side; d) Submucosal injection of aprotinin on left side.

All the surgeries were performed by the same operator with identical surgical technique using the standard armamentarium. The patient’s face was prepared with 10% povidone-iodine solution (BetadineTM) and then draped following which inferior alveolar nerve, lingual nerve, and long buccal nerve block were administered using 2% Lignocaine Hydrochloride (with 1:80,000 Adrenaline) in 2 ml syringe with 26 gauge needle to achieve desired local anaesthetic effect. A standard incision (Ward’s incision) [27] was made in all cases and a mucoperiosteal flap was reflected using a Howarth’s periosteal elevator. The surrounding bone was removed with stainless steel burs (no.8). Wound closure was achieved using 3-0 black braided silk. After the surgery details of operation and duration of surgery (from incision to last suture) were recorded. Immediate postoperative instructions were given and no postoperative antibiotics were prescribed. However, all patients were prescribed paracetamol 500 mg (1 tablet every 6 h for two days) postoperatively and advised to avoid any medications but those prescribed. Patients were asked to take diclofenac sodium 50 mg 1 tablet if they experienced intolerable pain, only after rating their daily pain score as severe pain.
The patients were recalled for follow up on the first, second and seventh postoperative day by the same examiner. The patients were assessed for swelling, pain, wound healing and global pain on day 7 after removal of sutures. At the end of investigation, patients were asked to choose the least painful side. The mean value and standard deviation for each of the parameters was considered and checked for statistical significance using the Mann-Whitney test, which is used for non-parametric values.
Results
All 30 patients completed the study.
Postoperative pain and pain distribution
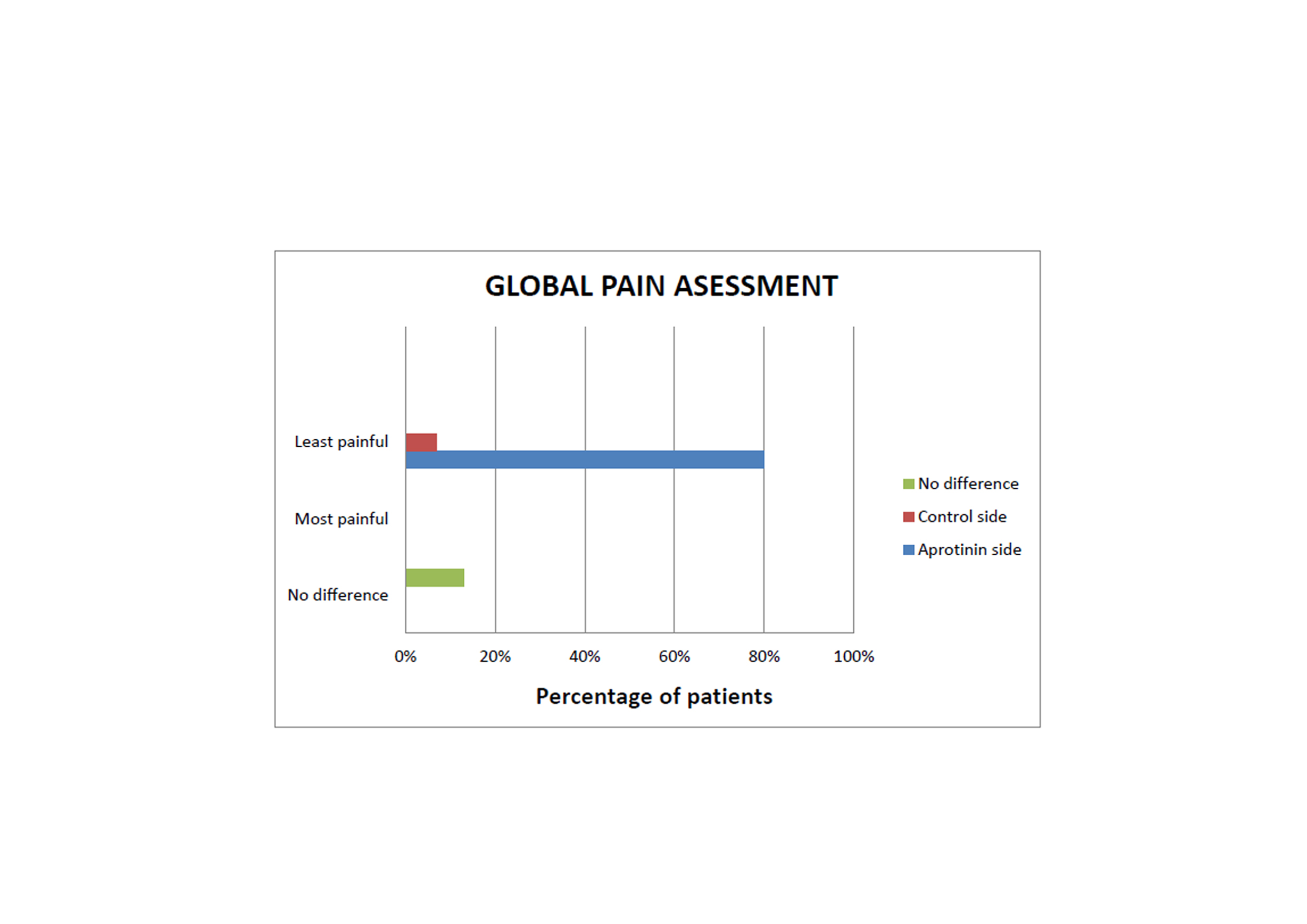
When global pain was assessed, 24 (80%) of the patients chose aprotinin side to be less painful than the control. Two (7%) patients chose control side less painful and four (13%) patients found no difference between study and control side [Table/Fig-3]. Mean readings were taken on each 1st, 2nd, and 7th postoperative days according to the degree of pain the patients described verbally as mild, moderate, severe, very severe and worst pain (0, 1, 2, 3, 4 and 5). No patients complained of very severe pain and worst possible pain. Mann-Whitney U-test was used to calculate the difference in pain between aprotinin and control side. Subjects experienced less pain on the aprotinin side compared to control side postoperatively. On the 1st and 2nd Postoperative days the mean pain scores on the aprotinin side was less compared to the control side [Table/Fig-4] with p-values of 0.000 and 0.000 respectively which was highly significant. On the 7th Postoperative day the mean pain score was 0.03 on the aprotinin side, whereas it was 0.20 on the control side (p-value of 0.046) which was also significant.
Global pain assessment between study and control side.
Depicting mean and standard deviation of pain scores on the Aprotinin and control side for the 1st, 2nd and 7th postoperative day respectively. SD (Standard deviation).
| 1st post op day | 2nd post op day | 7th post op day |
|---|
| SIDE | Mean | SD | p-value | Mean | SD | p-value | Mean | SD | p-value |
|---|
| APROTININ | 1.07 | 0.64 | 0.000 | 0.33 | 0.48 | 0.000 | 0.03 | 0.18 | 0.046 |
| CONTROL | 1.80 | 0.66 | 1.20 | 0.48 | 0.20 | 0.41 |
The pain distribution was assessed on 1st, 2nd and 7th day postoperatively where patients complained of no pain, mild pain, moderate pain and severe pain on both study and control side [Table/Fig-5]. The difference in pain distribution between aprotinin and control side on all days was not significant. The p-values on 1st, 2nd and 7th day were 0.73, 0.14 and 0.57 respectively. Zero percent of patients complained of pain on the aprotinin side on 1st Postoperative day whereas on test side 4% complained of severe pain. On the 7th day 96.6 % patients complained of no pain [Table/Fig-6].
Pain distribution on 1st, 2nd and 7th day Postoperatively on both study and control side.
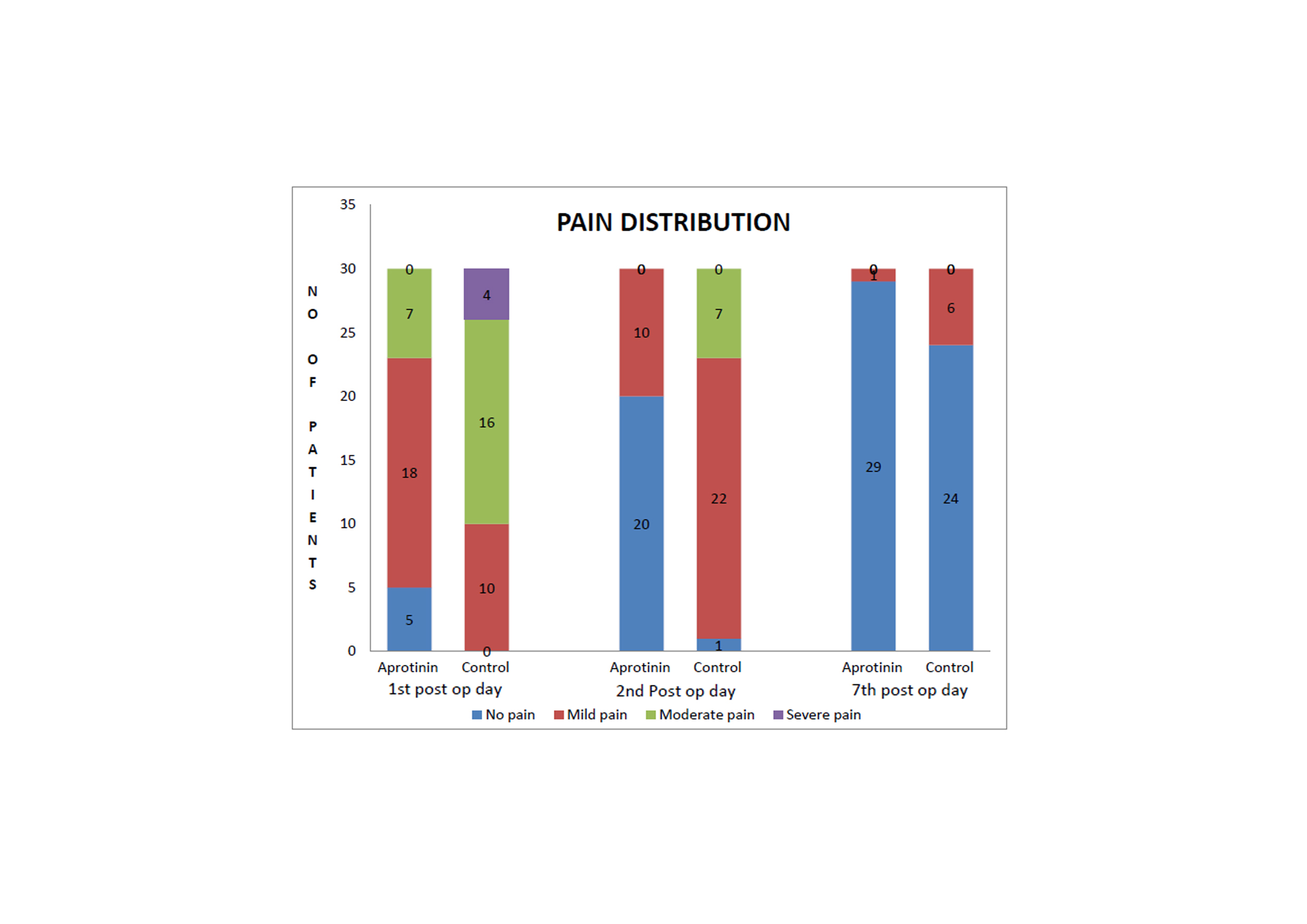
Shows the pain distribution in study and control side for all the patients on the 1st, 2nd and 7th postoperative days.
| STUDY SIDE |
| PAIN SCORE | No. of patients1st post-op day | No. of patients2nd post-op day | No. of patients7th post-op day |
| NO PAIN | 0 | 20 (66.6%) | 29 (96.6%) |
| MILD PAIN | 18 (60%) | 10 (33.3%) | 1 (3.3%) |
| MODERATE PAIN | 7 (23.3%) | 0 | 0 |
| SEVERE PAIN | 0 | 0 | 0 |
| CONTROL SIDE |
| PAIN SCORE | No. of patients1st post-op day | No. of patients2nd post-op day | No. of patients7th post-op day |
| NO PAIN | 0 | 1 (3.3%) | 24 (80%) |
| MILD PAIN | 10 (33.3%) | 22 (73.3%) | 6 (20%) |
| MODERATE PAIN | 16 (53.3%) | 7 (23.3%) | 0 |
| SEVERE PAIN | 4 (13.3%) | 0 | 0 |
Time taken for surgery
The total time for surgery was noted (from the time of incision was placed till the last suture was given). It was found that on aprotinin side the minimum time taken for surgery was 51.3±10.3 minutes. In the saline group the mean duration of surgery was 59.4±8.9 min. Hence there was no significant difference between both groups.
Measurement of Swelling
The swelling was measured on pre operative, 1st, 2nd and 7th postoperative days. On the 1st postoperative day, the mean swelling was 1.07±0.64 mm on the aprotinin side, whereas on the control side the mean was 1.80±0.66 mm. On 2nd Postoperative day the mean was 0.33±0.48 mm on the aprotinin side, whereas on the control side the mean was 1.20±0.48 mm. On the 7th Postoperative day the mean was 0.03±0.18 mm on the aprotinin side, whereas on the control side the mean was 0.20 ± 0.41mm. The difference in swelling was not statistically significant. The average swelling in millimeters on each day is depicted in [Table/Fig-7].
Comparison of mean swelling size between study and control side Postoperatively.
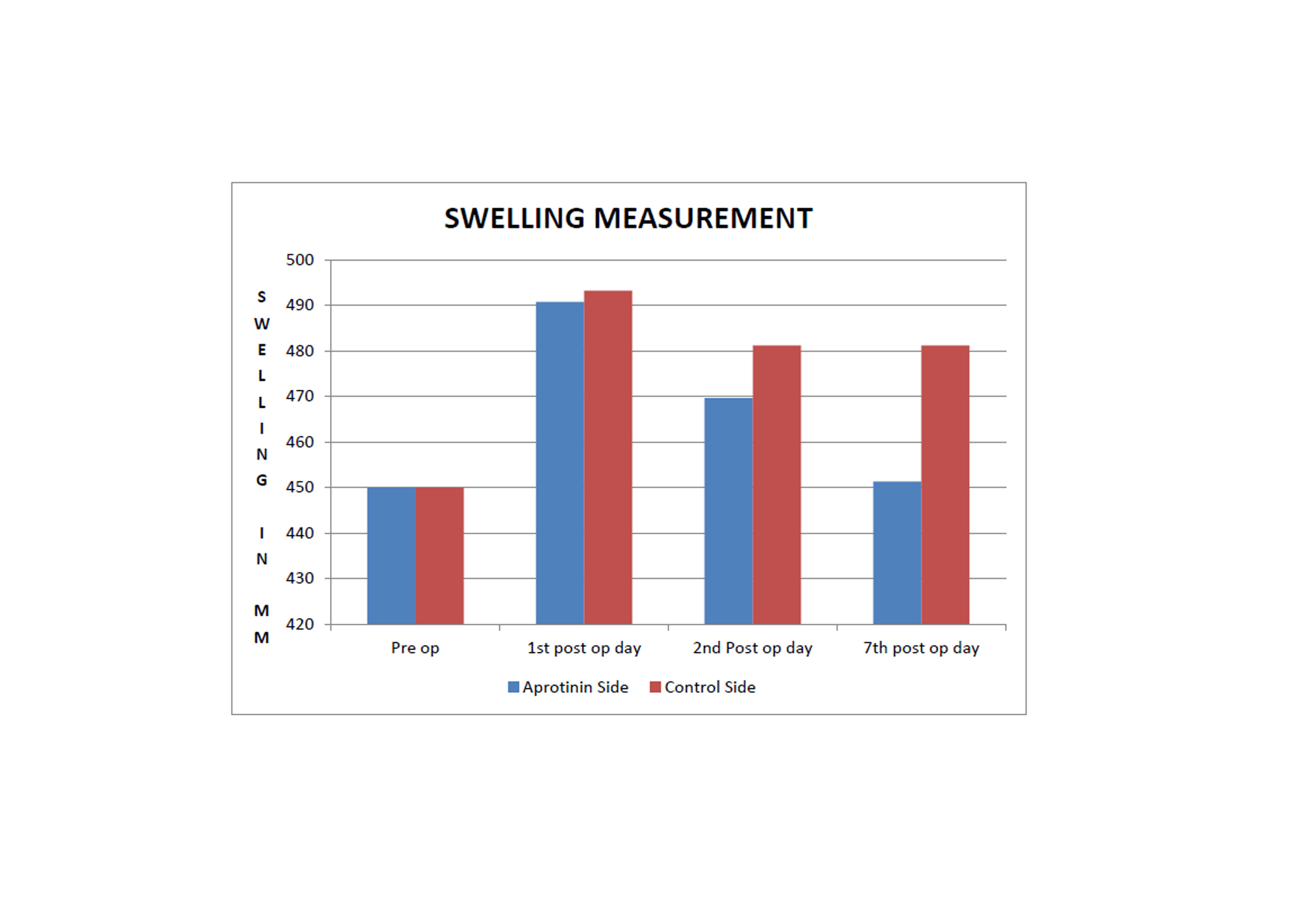
However, clinically it was evident that swelling on the side with aprotinin was less as compared to the control side on the 1st, 2nd, and 7th postoperative days [Table/Fig-1d-f]. The comparison of mean swelling size between test and control side is depicted in [Table/Fig-7]. It can be observed that swelling size is evidently lesser in the aprotinin side compared to control. The total time for surgery was also noted and found that on aprotinin side the mean time taken for surgery was 51 minutes whereas on control side was 50 minutes respectively.
Aprotinin injection
The adverse effects associated with the drug were also recorded. No intraoperative or postoperative complications were encountered in any of the patients included in the study.
Discussion
In the present study the efficacy of aprotinin in management of postoperative pain and swelling after mandibular third molar surgery was assessed. It has been observed that use of aprotinin clinically rarely causes hypersensitivity reaction [19]. Surgical removal of impacted third molar causes moderate to severe pain and forms a useful model for assessing the efficacy of analgesics [6,28]. Therefore, the mandibular impacted third molar was chosen as a clinical model in the present study.
The interpretation of pain, experienced by the patients has always been a challenge since it is based on individual perception. Based on studied methods of pain assessment the Verbal Pain Intensity Scale was used to evaluate pain in the present study [25]. Evaluation of facial swelling resulting from surgical procedure was difficult as swelling involves a three dimensional volumetric change at the tissue and cellular level. Methods used to evaluate swelling include photographic analysis [29], modified face-bow [30], linear measurements [26] and subjective assessment [31]. It has been observed that linear measurements are a practical and reliable technique for measuring swelling [26]. In agreement to this observation, linear measurement for assessing postoperative facial size was incorporated in the present study. All patients were given antibiotics one hour prior to surgery and anti inflammatory drugs following the surgery. The surgical trauma between the aprotinin and control sides was equalized so that patient’s responses would be meaningful.
The postoperative pain assessment reflected that pain was considerably reduced on aprotinin side of the mouth following extraction of third molars on all follow up days. The pain reduction by aprotinin was highly significant on the 1st and 2nd postoperative days and significantly lesser on the 7th postoperative day [Table/Fig-3,4].
The interrelation between complaints after surgical removal of mandibular molar and time taken for surgery has been studied and it has been concluded that longer the operation takes more the postoperative pain [32]. In the present study, surgical time for all cases was noted and mean time taken for both the aprotinin and control side was equal.
Linear measurements of swelling on the 1st, 2nd and the 7th postoperative days were comparatively lesser on the side of the face in which aprotinin was injected than the control side but not statistically significant on either side [Table/Fig-7]. This may be due to the smaller sample size included in the study. The facial size clinically was seen to reach normalcy on the aprotinin side by the 7th postoperative day but not on the control side [Table/Fig-1].
The results of the present study was similar to a previous study conducted to evaluate the value of aprotinin in third molar surgery and which concluded that aprotinin reduced pain and swelling postoperatively [11].
A major concern was healing of the sockets on the side where aprotinin was given which might be compromised because of inhibition of the initial acute inflammatory reaction. However, when sockets were checked for adequate healing after one week, both the sides showed satisfactory healing in all the patients. When the patients were reviewed a week following extractions, most confirmed that aprotinin side of the mouth had been less painful and the discomfort was lesser than the control side. Results from this investigation may be correlated with the unique property of aprotinin in inhibiting the mediators of acute inflammation. These mediators, which cause pain when applied to nerve endings and increase vascular permeability, were not activated and therefore the tissue reaction to trauma was reduced. In view of this observation injection of 1ml aprotinin, submucousally around the surgical site 5 minutes before the surgical procedure markedly reduces postoperative pain and swelling clinically, thereby helping the patient resume normalcy at the earliest.
Limitation
The study had a few limitations. Firstly, aprotinin could have been used in a larger number of patients undergoing surgical removal of mandibular third molar. Secondly, comparative studies with other drugs like corticosteroids to ascertain its efficacy conclusively would have provided a better result.
Conclusion
Within the limitations of the present study it may be concluded that aprotinin proved to have definite benefits for relief of postoperative pain and swelling clinically. A local infiltration of aprotinin is less traumatic than corticosterois which have to be administered through a more invasive parenteral route. Injection of aprotinin noticeably reduces pain and swelling postoperatively. Although the present study was standardized to maximum possible extent more studies should be encouraged in long term therapy of aprotinin in terms of safety, its use in other surgical procedures.
[1]. Susarla S, Dodson T, Risk factors for third molar extraction difficultyJ Oral Maxillofac Surg 2004 62:1363-71. [Google Scholar]
[2]. Shepherd JP, Brickley M, Surgical removal of third molarsBr Med J 1994 309:620-21. [Google Scholar]
[3]. Alexander RE, Throndson RR, A review of preoperative corticosteroid use in dentoalveolar surgeryOral surg Oral med Oral Pathol Oral Radiol Endod 2000 90:406-15. [Google Scholar]
[4]. McGrath C, Comfort MB, Lo EC, Luo Y, Changes in life quality following third molar surgery - the immediate postoperative periodBr Dent J 2003 194:265-68. [Google Scholar]
[5]. Esen E, Tasar F, Akhan O, Determination of the anti inflammatory effects of methylprednisolone on the sequele of third molar surgeryJ Oral Maxillofacial Surg 1999 57:1201-06. [Google Scholar]
[6]. Krekmanov L, Nordenram A, Postoperative complications after surgical removal of mandibular third molarsInt J Oral Maxillofac Surg 1986 15:25-29. [Google Scholar]
[7]. Seymour RA, Walton JG, Pain control after third molar surgeryInt J Oral Surg 1984 13:457-85. [Google Scholar]
[8]. Koerner KR, Steroids in third molar surgery: a reviewGen Dent 1987 35:459-63. [Google Scholar]
[9]. Bailey BM, Zaki G, Rotman H, Woodwards RT, A double-blind comparative study of soluble aspirin and diclofenac dispersable in the control of postextraction pain after removal of impacted third molarInt J Oral Maxillofac Surg 1993 22:238-41. [Google Scholar]
[10]. Forbes JA, Kehm CJ, Grodin CD, Beaver WT, Evaluation of ketorolac, ibuprofen, acetaminophen, and an acetaminophen-codeine combination in postoperative oral surgery painPharmacotherapy 1990 10:94-105. [Google Scholar]
[11]. Brennan PA, Gardiner GT, McHugh J, A double blind clinical trial to assess the value of aprotinin in third molar surgeryBr J Oral Maxillofac Surg 1991 29:176-79. [Google Scholar]
[12]. Markovic A, Todorovic LJ, Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: a clinical trialInt J Oral Maxillofac Surg 2007 36:226-9. [Google Scholar]
[13]. Dakir A, Ramalingam B, Ebenezer V, Dhanavelu P, Efficacy of tranexamic acid in reducing blood loss during maxillofacial trauma surgery–a pilot studyJ Clin Diag Res 2014 8(online):ZC06-8. [Google Scholar]
[14]. Seymour RA, Blair GS, Wyatt FA, Postoperative dental pain and analgesic efficacy. Part IBr J Oral Surg 1983 21:290-97. [Google Scholar]
[15]. Seymour RA, Blair GS, Wyatt FA, Postoperative dental pain and analgesic efficacy. Part IIBr J Of Oral Surg 1983 21:298-303. [Google Scholar]
[16]. Habib S, Matthews RW, Scully C, Levers BG, Shephered JP, A study of the comparative efficacy of four common analgesics in the control of postsurgical dental painOral Surg Oral Med Oral Pathol 1990 70:559-63. [Google Scholar]
[17]. Neupert EA, 3rd, Lee JW, Philput CB, Gordon JR, Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removalJ Oral Maxillofac Surg 1992 50:1177-82. [Google Scholar]
[18]. Ohnishi M, Kawai T, Ogawa N, Double-blind comparison of piroxicam and mefenamic acid in the treatment of oral surgical painEur J Rheumatol Inflamm 1983 6:253-58. [Google Scholar]
[19]. Beierlein W, Scheule AM, Dietrich W, Ziemer G, Forty years of clinical aprotinin use: A review of 124 hypersensitivity reactionAnn Thorac Surg 2005 79:741-48. [Google Scholar]
[20]. Kraut H, Frey EK, Bauer E, Uber ein neues Kreislaufhormon. II. MittleilungHoppeSeylers Z. Physiol Chem 1928 175:97-114. [Google Scholar]
[21]. Landis RC, Haskard DO, Taylor KM, New anti-inflammatory & platelet-preserving effect of aprotininAnn Thorac Surg 2001 72:1808-13. [Google Scholar]
[22]. Landis RC, Asimakopoulos G, Poullis M, Haskard DO, Taylor KM, The anti-thrombotic and anti-inflammatory mechanisms of action of aprotininAnn Thorac Surg 2001 72:2169-75. [Google Scholar]
[23]. Mannucci PM, Haemostatic drugsN Engl J Med 1998 339:245-53. [Google Scholar]
[24]. Kunitz M, Northrup J, Isolation from beef pancreas of crystalline trypsinogen, trypsin, trypsin inhibitor, and an inhibitor trypsin compoundJ Gen Physiol 1936 19:991-1007. [Google Scholar]
[25]. Portenoy RK, Tanner RM, Visual Analogue Scale and Verbal Pain Intensity Scale. In: Portenoy RK and Tanner RM, editorsPain Management: Theory and Practice 1996 5th edOxford University press:300-10. [Google Scholar]
[26]. Holland CS, The development of a method of assessing swelling following third molar surgeryBr J Oral Surg 1979 17:104-14. [Google Scholar]
[27]. Ward TG, Split bone technique for removal of lower third molarBr Dent J 1956 101:297-301. [Google Scholar]
[28]. Mercier P, Precious D, Risks and benefits of removal of impacted third molar. A critical review of the literatureInt J Oral Maxillofac Surg 1992 21:17-27. [Google Scholar]
[29]. Singh V, Alex K, Pradhan R, Mohammad S, Singh N, Techniques in the removal of impacted mandibular third molar: a comparative studyEur J Gen Dent 2013 2:25-30. [Google Scholar]
[30]. Grossi G, Maiorana C, Garramone R, Borgonovo A, Creminelli L, Santoro F, Assessing postoperative discomfort after third molar surgery: a prospective studyJ Oral Maxillofac Surg 2007 65:901-17. [Google Scholar]
[31]. Breytenbach HS, Objective measurement of postoperative swellingInt J Oral Surg 1978 7:386-92. [Google Scholar]
[32]. Pedersen A, Interrelation of complaints after removal of impacted mandibular third molarsInt J Oral Surg 1985 14:241-44. [Google Scholar]