Human speech is characterized by resonance, one among many diverse acoustical aspects that differentiates phonetic segments. During oral sound production coupling of oro-nasal cavity leads to an additional nasal resonance coined as hypernasality [1]. Abnormal resonance, like hypernasality, in subjects with cleft palate often results in poor speech intelligibility, a major concern most commonly met by the Speech Language Pathologist [2]. Over the years perceptual assessment of nasality has constituted to be an indispensable part in speech assessment of individuals with unrepaired and repaired cleft palate [3,4]. In research settings perceptual evaluation has captured reliable evidences in rating resonance changes when the judges are experienced, besides presenting poor intra-judge reliability in clinical setting [5]. However to monitor surgical outcomes and treatment progress incorporating objective repeatable measures must be included in routine assessment protocol. To facilitate this aspect, spectral analysis has proven to act as a boon, in addition to complementing perceptual assessment.
Objective evaluation provides explicit information with respect to certain ranges of nasal resonance that was particularly difficult for listener to resolve. Nasality is evaluated objectively by using simple microphone recordings and analysing those using spectral tools. In the same line of thought recently an algorithm was conceived by the name of VLHR, a quantitative spectral measure that calculates nasal resonance based on the intensity spectrum. The VLHR is defined as the power ratio of the low frequency energy to high frequency energy obtained by dividing the voice spectrum with a specific cut-off frequency i.e., 600 Hz [6]. This acoustic index evidences a direct relationship between the VLHR values and degree of nasality. Hence provides researchers and clinicians a useful tool that helps in monitoring nasal resonance effectively [6–9]. Credited with pioneering works by Lee and colleagues there is little empirical study on the use of VLHR index to quantify nasality [6–9]. Moreover, only a handful of evidence is available in Indian population [10].
Perception of nasality is dependent on listener’s judgment. However, the drawback of perceptual evaluation continue to remain as a hurdle in planning rehabilitation programs, specifically prosthetic and surgical based intervention, that rely upon objective data to undermine the reason for hypernasality. Hence the present study was one attempt to objectively quantify decrease in nasality after surgery. The findings from various studies have revealed speech characteristics, quality and nasalence measures in individuals with cleft palate. Only few studies attempted to investigate the perceptual and nasalence measures before and after cleft palate surgery [11]. However, there are no reported studies of using VLHR index to measure nasality among individuals with cleft palate before and after surgery. Hence in the present study the VLHR index was implemented to measure the nasality for phonation samples. The main objective of the study was to measure and compare the VLHR values for phonation samples of individuals with cleft palate before and after surgery.
Materials and Methods
Subjects
Total of 30 children participated in the study. All were native speakers of Malayalam language within the age range of 8 to 15 years (mean=9.5 years), who underwent cleft palate surgery. Subjects diagnosed of congenital cleft palate and undergone surgery to repair the same participated in the study (heterogeneous group). Subjects were screened for speech, language and hearing loss by an experienced Speech Language Pathologist. Subjects presenting with blocked nose or with nasal congestion as assessed during the oro-motor examination did not participate in the study. The mean pre-operative duration was 2.1 days and the mean postoperative duration was 38.4 days.
Procedure
Speech recording was done with the subjects seated comfortably on chair with back support in a noise free room. They were instructed to produce 3 trials of sustained vowels (/a/, /i/ and /u/) for a minimum of 5 seconds at their comfortable pitch and loudness level. To maintain the input amplitude across subjects, the speech samples were monitored and adjusted to a predetermined level. The samples were recorded in two sessions from each subject using Sony digital recorder ICD–U60 placed 10 cm mouth to microphone distance. The samples were further subjected to perceptual analysis using 6-point scale to rate nasality for all speech samples and spectral analysis to extract VLHR parameter for phonation samples (/a/, /i/, /u/).
Perceptual Analysis
The samples recorded before and after surgery were normalized and randomly numbered. Three Speech Language Pathologists trained in the evaluation of cleft palate speech, listened to these samples separately. They were instructed to indicate the degree of perceived nasality in the speech samples based on the 6-point scale, where grade 0 representing “no nasal resonance” and 1, 2, 3, 4 and 5 representing “mild,” “mild-moderate,” “moderate,” “moderately severe,” and “severe hypernasal resonance” respectively. Earlier studies used similar scale to rate hypernasality [6,12]. They were further instructed not to pay attention to any other parameter of speech (voice, articulation, prosody etc) while they were doing the rating. They could ask for a replay of the sample if required. The ratings were recorded on a scoring sheet given for each sample. Inter and intra judge reliability was determined by making the listeners to mark for 10% of speech samples which they had analysed earlier. Intra judge reliability was calculated for all the three judges using Pearson’s correlation analysis and the coefficients were 0.87, 0.89, and 0.91 respectively. Inter judge reliability was obtained using intraclass correlation and the coefficients were 0.75, 0.80, and 0.87. Thus, inter and intra judge correlation regarding the nasality rating was noted for reliability.
Acoustic Analysis
The recorded phonation samples were fed directly into the Praat software [13] (Version 5.1.43) digitally and sampled at 44 kHz. Spectral analysis was performed on the samples using the Praat script [8], which extracts the VLHR parameter. Only mid stable portion of minimum 3 seconds was selected to extract the VLHR parameter. Further, VLHR parameter was calculated by dividing the voice spectra into a low frequency power (LFP) section and a high frequency power (HFP) section using 600 Hz cut-off frequency. This is controlled by the Praat script loaded and saved on the dynamic menu of software. LFP was defined as the summation of the power spectrum from 50 Hz to 600 Hz and HFP was defined as the summation of the power spectrum from 600 Hz to 8063 Hz [6,8]. The extracted VLHR values were represented in dB unit.
Statistical Analysis
The mean rating score for nasality for pre and postoperative speech samples were computed from each subject. The mean and standard deviation values of VLHR for phonation samples (/a/, /i/, /u/) extracted from Praat software were also averaged. The data was subjected to statistical analysis using SPSS (Version 17). Analysis of Variance was used on the data to determine the significant difference for all phonation samples recorded across pre and postoperative sessions.
Results
Perceptual Analysis
Overall mean hypernasality rating score was obtained by taking the average of the three judges rating on 6-point scale. Of these, higher mean rating scores were noted for speech samples collected after surgery compared to that of scores obtained for speech samples before surgery. Speech samples in the pre-operative condition were perceived to have varying levels of hypernasality that was scored between moderately severe to severe hypernasality i.e., ranged between 4 to 5, and in postoperative condition rating scored between mild to moderate hypernasality i.e., ranged between 0 to 3.
Acoustic Analysis
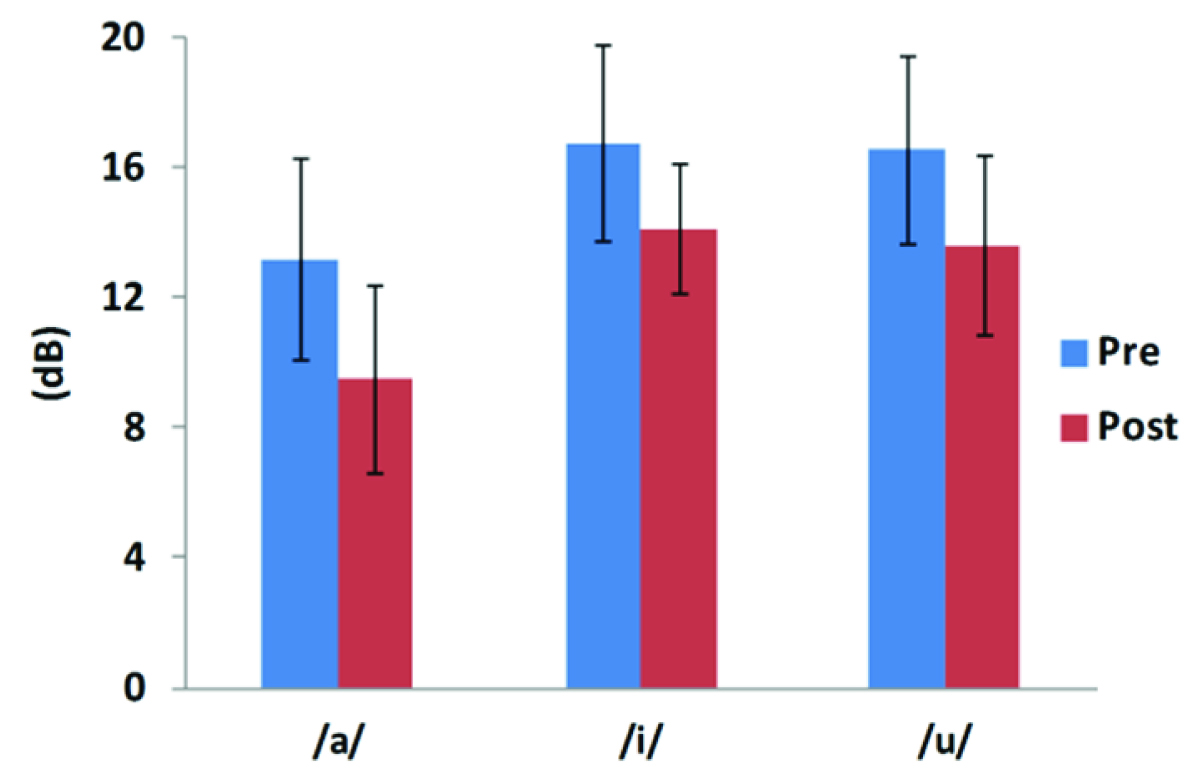
[Table/Fig-1] displays the mean and standard deviation (SD) values of VLHR across pre and postoperative conditions. Postoperatively the VLHR values were lower compared to that of pre operative VLHR values. Results showed that high front vowel /i/ had the highest VLHR value followed by high back vowel /u/ and low mid vowel /a/ for both the conditions. The changes in mean with SD of VLHR analysis are represented in [Table/Fig-2]. Results of ANOVA indicated significant difference between pre and postoperative conditions for /a/ phonation {F (1, 58) =22.92, p=0.000}, /i/ phonation {F (1, 58) =15.96, p=0.000} and /u/ phonation {F (1, 58) =14.71, p=0.000}.
Mean with SD of VLHR values for pre-operative and postoperative condition.
| preoperative | postoperative |
|---|
| Mean (±SD) in dB | Mean (±SD) in dB |
|---|
| /a/ | 13.19 (±3.11) | 9.49 (±2.87) |
| /i/ | 16.76 (±3.00) | 14.13 (±1.97) |
| /u/ | 16.54 (±2.88) | 13.62 (±2.78) |
Mean with SD VLHR values in dB for preoperative and postoperative conditions
Discussion
As expected the results of the present study indicated that, the perceived hypernasality scores reduced for phonation samples collected after surgery compared to that of samples collected before surgery. Perceptual analysis results are consonance with the findings of earlier studies [11,14], where they reported reduced hypernasality in children who underwent primary palatal surgery. In the present study, the postoperative scores ranged from 0 to 3 (no nasal resonance to mild to moderate degree). This wider distribution in nasality rating scores, were mainly because of individualistic variations in the velopharyngeal sphincter functioning after surgery. Despite of these factors, the children with cleft palate surgery showed reduced hypernasality scores and attending speech therapy will further enhance the benefits after surgery and consequently improve their communication effectively.
The results, supporting findings of previous studies [15,16], showed that the high vowel /i/ had significant higher VLHR value compared to vowel /u/ and /a/ in both the conditions. The higher VLHR values obtained are attributed to the articulatory postures observed during these vowel productions. Apparently the low mid vowel /a/ is an open vowel, hence this is expected to give rise to a relatively little oral airflow resistance. Therefore leading to maximum transmission of energy via the oral cavity and thus relatively lowers VLHR values compared to vowel /i/ and /u/ values [7]. The results also support the findings of other researchers [17] who reported greater degree of nasality on high vowels because of increased physiological demand on the velopharyngeal closure mechanism. This leads to a more tight seal between posterior pharyngeal wall and velum thereby limiting flow of acoustic energy into nasal cavity.
Between the three vowels, literature is suggestive of increased oral impedance during production of vowel /i/. Apparently, this creates scope for resistance in oral airflow and facilitates increased nasal airflow. Based on these views, the transpalatal nasalance theory was put forth that reviews higher nasal scores for vowel /i/ [17]. Adding to these views are the shared resonance properties of vowel /i/ and nasal cavity. The acoustic feature of vowel /i/ characterizes a first formant frequency at close proximity to nasal murmur created by soft palate [17]. This information sheds light on greater degree of sound variations in nasal cavity. On the contrary, vowel /a/ is a low vowel that is produced with an open mouth approach that has relatively less oral impedance. This continuingly increases the acoustic power spectrum and vocal intensity at the level of oral cavity [18].
Recently, studies were carried out to measure hypernasality using VLHR in different clinical population like subjects with nasal decongestion, palatal fistula and velopharyngeal [6–8]. These studies reported significantly increased VLHR after decongestant treatment, higher VLHR values in nasalized sounds than oral sounds and high correlation of VLHR index with perceptual rating and nasalence scores. Comparison between earlier works and the present study is challenging due to differences in method adopted. However, on the other hand studies suggest that presence of nasal resonance consists of increased low frequency energy i.e., nasal formant and decreased high frequency energy i.e., anti resonance of nasal voices because of velopharyngeal inadequacy [19,20]. Based on these assumptions, the VLHR values obtained in our cleft palate subjects are in consonance with the results of earlier studies.
Despite these remarks perceptual assessment remains as a gold standard approach for evaluating nasality [3]. However, perceptual assessment becomes more challenging in complex populations like cleft palate due to varying components of voice like pitch, loudness and resonance imparting a great influence on the signal perceived by the listener.
Limitation
Further the results of this study must be considered in the context of following limitations. The samples analysed in the present study were only phonation samples (/a/, /i/, & /u/). Future work is necessary to test the VLHR in different CVC combinations, passage reading, and connected speech. Also, the effect of different type and approach of surgery to correct cleft palate can be studied objectively.
Conclusion
This study is an attempt to use spectral measure VLHR, to note nasality in children with cleft palate before and after surgery. Results revealed that the VLHR values were lower for cleft palate subjects postoperatively. The reduced VLHR values postoperatively, may be attributed to the properties of decreased low frequency energy of nasal voice in cleft palate subjects after surgery. Hence, we conclude that VLHR parameter is sensitive enough to detect nasal voices in cleft palate subjects. Further research can be carried out on a larger sample of individuals with cleft palate to establish the validity of using VLHR and determining its efficacy as a definitive tool for clinical setup. Specifically, studies can be carried out to note the treatment outcome before and after speech therapy in children and adults.