In the past few decades there have been consistent efforts to improve maternal survival and also, the consequent demand for accurate estimates of maternal mortality [1]. The very low figures of maternal mortality and the absence of reliable registration system have therefore stimulated an interest in investigating cases of life threatening obstetric morbidity or ‘maternal near-miss’ [2]. All women who have experienced an acute medical condition during pregnancy, intrapartum or postpartum are labelled as ‘near-miss’ or severe acute maternal morbidity (SAMM) cases [3]. Women who survive life-threatening conditions arising from complications related to pregnancy and childbirth have many common aspects with those who die of such complications [4,5].
In India, post Reproductive & Child Health and National Rural Health Mission (RCH & NRHM) review of maternal health status does indeed show a positive trend with respect to provision and utilization of safe motherhood services including facility preparedness for Essential & Emergency Obstetric Care (EOC, EmOC) [6]. In Uttarakhand, a state in Northern India, MMR has registered a downward trend (183 for Garhwals & 190 for Kumayun division, AHS, 2011-12) and rising institutional deliveries (50% AHS, 2011-12) vis-a-vis the structural and strategic changes for quality enhancement [7,8].
The present study was designed to evaluate Quality of Care (QOC) for severe pregnancy complications in terms essentially of critical interventions use in life-threatening conditions (‘near-miss’ criteria) and maternal vital status at all three tiers of health care, i.e., primary, secondary and tertiary care level for prevention and management of severe complications related to pregnancy and childbirth at Doiwala Block of district Dehradun, India.
Materials and Methods
The present observational (cross-sectional) study was carried out over a period of 12 months (June 2012 to May 2013), which included data collection for six months (June 2012 to November 2013) and data analysis for next six months, under the Department of Community Medicine, HIHT University. The present study included all women (937) attending health-care facilities at different levels i.e. Primary, Secondary & Tertiary level in the Doiwala block of Dehradun district, who were either pregnant, in labour, or who had delivered or had aborted up to 42 days ago and arrived at the health-care facility with any of the listed conditions or those who developed any of those conditions during their stay at the health-care facility after taking written informed consent from in charge of the facility [5]. The two PHC were selected out of seven PHC by systematic random sampling technique [7]. There is only one CHC in the block and one tertiary health centre (THC) i.e. Himalayan Institute of Medical Sciences (HIMS) under HIHT University. Data was collected using patient records.
Operational Definition: Maternal ‘near-miss’ has been defined as a severe life threatening obstetric complication requiring immediate medical intervention to prevent expected death of the woman; any pregnant or recently delivered woman, in whom immediate survival of the woman is threatened and who survives just by sheer luck or due to the medical care she received [5,9]. The case identification was done by clinical criteria related to a specific disease entity such as severe eclampsia or haemorrhage; or a specific intervention such as admission to an intensive care unit or procedure such as a hysterectomy or massive blood transfusion; or a method whereby organ system dysfunction such as shock or respiratory distress was identified [10].
Inclusion criteria: Women who were pregnant, in labour, or who delivered or aborted up to 42 days ago arriving at the facility with any of the listed conditions or those who developed any of those conditions during their stay at the health-care facility were eligible.
Exclusion Criteria: Women who developed conditions unrelated to pregnancy (i.e. not during pregnancy or 42 days after termination of pregnancy) were not eligible.
Probability sampling was done using systematic random sampling technique to select health facilities amongst Primary & Community Health Centres (PHC, CHCs) and Tertiary health centre [11]. The facilities sampled were 02 PHCs (Chidderwala and Bhaniyawala) out of 7 PHCs, 01 CHC (Doiwala) and 01 Tertiary facility (Himalayan Hospital, Himalayan Institute Hospital Trust (HIHT) [7].
The minimum sample size for producing near-miss and process indicators has not been formally established. Varying proportion of Severe Maternal Outcomes (i.e. maternal deaths plus ‘near-miss’ cases divided by the number of women giving birth within a given time period) have been used to estimate the sample size at different study setting across countries [9]. However, a sample with at least 20 cases of severe maternal outcome (i.e. maternal deaths plus near-miss cases divided by the number of women giving birth within a given time period) has been assumed to be desirable to produce meaningful results [9].
In the present study a convenient sampling was done to recruit 937 consecutively reporting women fulfilling eligibility criteria (a hundred percent enumeration of eligible study subjects during the study period) for the audit [11].
Statistical Analysis
Software Epi-info was used for data analysis. Data was described in rates, ratios and proportions. Non-parametric test i.e. chi-square tests were employed to ascertain associations between study variables and statistical significance at p-value < = 0.05.
Ethics: Ethical clearance from the Institute Ethics Committee was obtained vide letter number – HIHTU/HIMS/ETHICS/2013/40 dated 30.08.2013. Since no direct contact was required with any patient at individual level but only records were followed at all the selected facilities, no informed written consent was taken from the patients included in the study. However, consent was taken from the In-charges of all the selected Health facilities.
Results
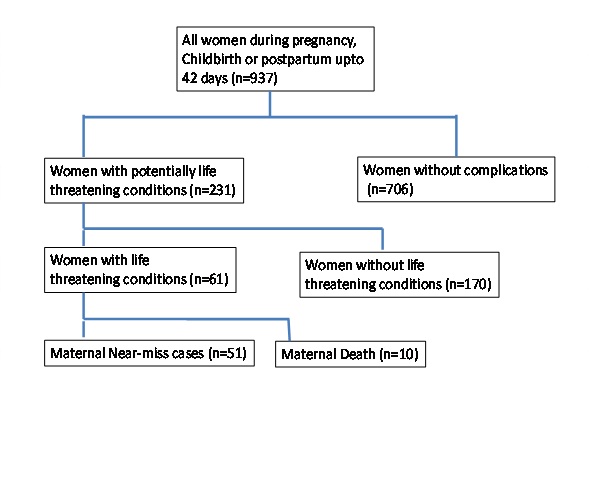
Nine hundred and thirty seven women arriving at the facility with any of the listed conditions or those who developed any of those conditions during their stay at the health-care facility after taking written informed consent from in-charge of the facility were enrolled. It was observed that out of 937 pregnant women 231 (24.66%) had one or more potentially life threatening condition (PLTC), while 75.34% of pregnant women had uncomplicated outcome. All the pregnant women at primary health center (53 cases of 53) had normal outcome. Most of the women with potentially life threatening condition were seen in tertiary health care (78.79%), followed by community health center, and there were no cases reported from primary health center. Out of a total of 51 cases of maternal near-miss cases, 50 (98.04%) were reported from THC and 01 (01.96%) case from community health center (CHC). There were10 maternal deaths occurred in the THC and there were no deaths reported from CHC or PHC. Detailed distribution of cases has been published earlier [11]. Process and outcome indicators related with specific conditions are shown in [Table/Fig-1]. The [Table/Fig-2] shows distribution of various case types in the study population [12]. [Table/Fig-3] depicts intensive care use in women with potentially life threatening conditions in tertiary care hospital.
Process and outcome indicators related with specific conditions. No cases of potentially life threatening conditions reported from primary health center (n=53).
| Indicators | CHC | Tertiary Hospital |
|---|
| 1. Prevention of postpartum haemorrhage |
| Target population: women giving birth in health-care facilities | 424(45.2) | 460(49.1) |
| Oxitocin use | 417(98.3) | 460(100) |
| Use of any other uterotonic | - | - |
| 2. Treatment of severe postpartum haemorrhage |
| Target population: women with severe PPH | 33(67.34) | 70(38.46) |
| Oxitocin use | 33(100) | 70(100) |
| Ergometrine | 26(78.78) | 43(61.42) |
| Misoprostol | 12(36.36) | 17(24.28) |
| Tranexamic acid | - | - |
| Removal of retained products | 03(09.09) | 24(34.28) |
| Balloon or condom tamponade | - | - |
| Artery ligation | 00 | 02(02.85) |
| Hysterectomy | 00 | 03(04.28) |
| Abdominal packing | 00 | 01(01.42) |
| Proportion of cases with SMO | 00 | 23/70 |
| Mortality | 00 | 04(05.71) |
| 3. Anticonvulsants for eclampsia |
| Target population: women with eclampsia | 00 | 19 |
| Magnesium sulfate | 00 | 18(94.73) |
| Other anticonvulsant | 00 | 02(10.52) |
| Any anticonvulsant | 00 | 19(100) |
| Proportion of cases with SMO | 00 | 5/19(26.31) |
| Mortality | 00 | 04 (05.71) |
| 4. Prevention of caesarean section related infection |
| Target population: women undergoing caesarean section | - | 69 |
| Prophylactic antibiotic during caesarean section | - | 51(73.91) |
| 5. Treatment for sepsis |
| Target population: women with sepsis | 03 | 50 |
| Parenteral therapeutic antibiotics | 03(100) | 48(96) |
| Proportion of cases with SMO | 01/03(33.33) | 35/50(70) |
| Mortality | 00 | 06(12) |
| 6. Ruptured uterus |
| Target population: women with ruptured uterus | - | 03 |
| Laparotomy | - | 03(100) |
| Laparotomy after 3 hours of hospital stay | - | 01(33.33) |
| Proportion of cases with SMO | - | 02(66.66) |
| Mortality | - | 00 |
The figure shows distribution of various case types in the study population. (n=number of cases) [12].
Women with potentially life-threatening condition are women with ‘severe maternal complications’. This is an extensive category of clinical conditions, including diseases that can threaten a woman’s life during pregnancy and labour and after termination of pregnancy. Women with life-threatening conditions refer to all women who either qualified as maternal near-miss cases or those who died (i.e. women presenting a severe maternal outcome with organ dysfunction). It is the sum of maternal near-miss and maternal deaths
Intensive care use in women with potentially life threatening conditions in tertiary care hospital (n=18).
| Intensive care use | N | rates |
|---|
| Total number of women giving birth | 735 | - |
| ICU admission rate | 18/735 | 02.44% |
| ICU admission rate among women with SMO | 18/61 | 29.50% |
| SMO rate among women admitted to ICU | 18/18 | 100% |
| Proportion of maternal deaths assisted without ICU admission | 3/10 | 30% |
Discussion
Post-partum haemorrhage and its management: Association between use of oxytocin as preventive measure and level of health care was not found to be significant. In an analogous study by Tuncalp et al., conducted at a teaching hospital at Ghana, it was seen that 96.6% of women were given oxytocin for the prevention of post-partum haemorrhage [13]. In a similar study conducted by Jabir et al., from Iraq, the routine use of oxytocin was reported to be 86.36%, while Nelissen et al., from Tanzania reported that only 48% of females received oxytocin as a strategy for preventing post partum haemorrhage [14,15]. The higher rates of use of oxytocin indicate better preparedness by the health care facility to prevent PPH. Treatment of severe post partum haemorrhage by removal of retained products was significantly associated with levels of health care in the present study. Removal of retained products for treatment of PPH in our study (37%) is comparable to similar treatment findings by Tuncalp et al., from Ghana (20%) and by Jabir et al., from Iraq (19.05%) [13,15].
Severe PPH and its management: Further, study findings revealed that there were no associations found between use of oxytocin, ergometrin, misoprostol, removal of retained products, artery ligation, hysterectomy and abdominal packing as treatment of severe post partum haemorrhage of women with SMO and levels of health care. Comparable findings were observed in the study conducted in Srilanka by Ranatunga et al., where 85.7% women with severe PPH were treated with oxytocin [16]. The utility of oxytocin in treating PPH as reported by Jabir et al., (67.86%) was much lower than reported in our study [15]. Analogous results were found by Nelissen from Tanzania who also reported rates of 58% [14]. Tuncalp et al., in their study conducted at a teaching hospital, Ghana found that 62% of women with severe PPH were treated with oxytocin [13].
It can be inferred from the proportion of SMO cases using oxytocin in our study (96%) that status of facility preparedness in management of SMO cases requiring oxytocin was rather more than satisfactory.
In our study, hysterectomy was very sparingly chosen as the treatment of post-partum haemorrhage (5%). This finding is corroborated by Nelissen et al., from Tanzania who had reported rate of around 6% [14]. Higher percentage of 14.9% and 59.52% of hysterectomy as treatment of severe PPH were reported by Tuncalp et al., and Jabir et al., respectively [13,15]. In contradiction to our finding, higher rates might indicate that women with severe PPH arrived very late at the health care facility where conservative treatment could not be instituted and only surgical intervention like hysterectomy would save the women’s life.
Eclampsia and its management: Out of 19 women at the THC that had eclampsia, 18 (94.73%) received magnesium sulphate as primary treatment, and there were two women who in addition to magnesium sulphate received other anticonvulsants. More than a quarter (26.31%) of women with eclampsia developed SMO. It was observed that there were no cases of eclampsia reported from PHC or CHC and no mortality associated with eclampsia. Our findings are corroborated with the findings reported by Tuncalp et al., from Ghana who reported the use of magnesium sulphate in 97.1% of women with eclampsia [13]. Nelissen et al., from Tanzania reported anticonvulsant use which included magnesium sulphate for 93% [14]. Karolinski et al., 2013 from Argentina also reported 86.8% of the cases with eclampsia were treated with magnesium sulphate [17].
Although comparable but slightly lower rate for use of magnesium sulphate alone was reported by Jabir et al., from Iraq (67.44%) of the patients. However, in combination with other anticonvulsants the proportion receiving treatment was 93.02% [15].
Based on current evidence, only a negligible proportion of women with eclampsia would present actual contraindications for magnesium sulfate. Hence, the expected use of the intervention should be nearly 100%. In the present study it can be inferred that almost all the women with eclampsia virtually had received the prescribed anticonvulsant and thus this may not be interpreted as lack of facility preparedness in this regard [9].
Caesarean sections: Out of 69 caesarean sections performed at THC 51 (73.91%) had received antibiotic pre-operatively for prevention of caesarean section related infections. In an analogous study by Tuncalp et al., from a teaching hospital, University of Ghana, it was found that 96.9% women undergoing caesarean section were given prophylactic antibiotics [13]. In other two comparable although study by Jabir et al., from Iraq and Nelissen et al., from Tanzania women undergoing caesarian section who received prophylactic antibiotics were 60.75% and 66% respectively [14,15]. Regarding antibiotic use it can be observed that in our study scenario there was optimum/expected use of prophylactic use of antibiotic for women undergoing caesarean sections.
Sepsis: Regarding the management of women who developed sepsis all the women with sepsis at CHC and 96% of cases at the tertiary hospital received parenteral antibiotics. There were 70% cases at the THC which had associated Severe Maternal Outcome (SMO). In comparable studies conducted by Jabir et al., and Nelissen et al., the rates of antibiotic usage in cases of sepsis were reported as 100% and 93% respectively [14,15]. However, in a study by Tuncalp et al., from Ghana only 40% of women with sepsis were reportedly treated with antibiotics [13].
Women (100%) receive antibiotics as per protocol. Findings from the present study suggest that that there may not have been any gap in terms of facility preparedness & management of almost all women (96%) with sepsis. As regards the findings from the study at Ghana, such low rate of antibiotic usage may be because the country is essentially resource poor in terms of health care infrastructure and delivery.
Ruptured uterus: There were three cases at the tertiary hospital that had ruptured uterus and all of them (100%) underwent laparotomy. There was no associated mortality.
Analogous finding by Nelissen et al., from Tanzania reported that 100% of women with ruptured uterus had undergone laparotomy; however, the case fatality rate was 5% [14]. In another similar study by Jabir et al., from Iraq, 96.5% women with ruptured uterus had undergone laparotomy with a 10.34% mortality rate [15]. Tuncalp et al., also reported that 85.7% of women with ruptured uterus were intervened with laparotomy after three hours of hospital stay with no mortality [13].
Intensive care use: As regards the critical interventions and women with SMO, in the present study [Table/Fig-3] that blood products were used in 34 (66.66%) and 07 (70%) of cases of ‘near-miss’ and maternal death respectively. Interventional radiology was not used as critical intervention at any of the health care facilities in women with severe maternal outcome. Laparotomy was performed in 06 (11.76%) and 01 (10%) cases of ‘near-miss’ and maternal death respectively. A considerably high number of women had fatal outcome among those who received intensive care and a statistically significant difference was found with the ‘near-miss’ – thus showing a positive association of ICU admission with severe maternal outcome.
In a similar study by Ranatunga et al., from Srilanka, it was observed that women with ‘near-miss’ receiving critical interventions with regard to admission to intensive care unit was maximum i.e. 91 (100%), followed by laparotomy in 22 (24.8%) women. None of the women in his study settings had received interventional radiology as a critical intervention [16]. Shreshta et al., from Kathmandu, Nepal, found ICU admission in 28% and blood transfusion in 24% of women with ‘near-miss’ [18]. In a study conducted by Shen et al., from Kwaloon, China among the women with near-miss morbidity or mortality, 31 (40%) were admitted to the ICU and 32 (49.2%) were given blood products within 30 min, which, as life support procedures, were necessary to prevent death [19].
Data related to underlying causes and associated conditions (all health facilities) of women with PLTC in the present study reveal that eliciting and managing such causes and associated conditions by the care givers/facilities in anticipation of ‘near-miss’ cases among women with SMOs needs to be addressed.
It can be inferred from the findings of the present study and corroborated by findings of other cited references that indicators of pregnancy outcome i.e. end of pregnancy interventions, caesarean section rate, pre-term births, peri-natal deaths etc can be effective and reliable measures by the care givers/facilities for management of Severe Maternal Outcomes (SMOs) adopting the WHO ‘near-miss’ approach.
Strength of the study: The distinguishing feature of the present study in comparison to the above cited studies is the significant association that the morbidity conditions had with levels of care. As discussed earlier, available published literature did not consider ‘level of health care delivery’ as a study variable.
Limitation
The convenience sampling approach was realistic and made this study feasible. Second, this study is largely based on information obtained from medical records. In order to reduce the chances of recording bias, information from medical records was complemented with information obtained directly from the assisting staff (if relevant information was missing and in case of doubt). Third, the study population is essentially provided by THCs which tend to concentrate the more severe cases.
Conclusion
Application of WHO ‘near-miss’ tool indicates good quality of maternal care in rural healthcare setting in Uttarakhand, North India, who would have otherwise died due to obstetrics complications had proper care not been provided to them in time. Throughout the world majority of the maternal deaths are preventable, as solutions to prevent or manage pregnancy and delivery related complications are well known. Improvement in the maternal health can be achieved only if barriers that limit access to quality maternal health services are identified and addressed at all levels of the health system. The purpose of the WHO near-miss approach is to reduce preventable morbidity and mortality by using of evidence-based practices.