Extended spectrum β-lactamases (ESBLs) and AmpC β-lactamases are of growing concern to microbiologists for accurate detection and to clinicians for conferring resistance to several antibiotics resulting in treatment failure. They are most commonly produced by Klebsiella spp. and Escherichia coli but may also occur in other gram negative bacteria. Extended spectrum β-lactamases (ESBLs) are typically plasmid-mediated enzymes that hydrolyze penicillins, third generation cephalosporins and aztreonam [1]. They are not active against cephamycins (cephoxitin and cefotetan), but are susceptible to β-lactamase inhibitors (clavulanic acid). AmpC co-production has made ESBL phenotypes more complex. AmpC β-lactamases are cephalosporinases that are poorly inhibited by clavulanic acid and can be differentiated from ESBLs by their ability to hydrolyze cephamycins.
While genes for ESBLs are located on plasmids, genes for AmpC β-lactamases are either plasmid or chromosomally encoded. Chromosomally encoded AmpC are found in Enterobacter spp., Providencia spp., Citrobacter freundii, Morganella morganii, and Serratia marcescens. Expression of chromosomal AmpC may be constitutive or inducible. Plasmid mediated AmpC are found in K. pneumoniae, E. coli, Salmonella spp. and Shigella spp. Plasmid mediated AmpC genes were initially thought to be non-inducible, but inducible Amp Cgenes on plasmids have been reported [2].
Although, in new CLSI interpretive criteria, routine ESBL testing is no longer necessary but can be done for epidemiological and infection control purposes. But European Union Committee on Antimicrobial Sensitivity Testing (EUCAST) recommends that laboratories continue to screen and confirm ESBL production and to change a cephalosporin report from susceptible or intermediate to resistant if the isolate tests positive for ESBL production [3]. But ESBL detection in AmpC co-producing bacteria has become problematic for the microbiologists and to help guide the clinicians the appropriate antimicrobial therapy.
This calls for the urgent need to develop laboratory testing methods that can accurately detect the presence of these enzymes. Molecular methods can accurately detect ESBL but facilities for them are not available in most of the laboratories especially in developing countries. Various phenotypic methods have been recommended for routine use to detect ESBL production in gram negative bacilli. These employ a β-lactamase inhibitor, usually clavulanate, in combination with third generation cephalosporins (3GC) such as ceftriaxone, ceftazidime or cefotaxime [4]. But the inhibitor-based confirmatory test approach is most promising for isolates that do not co-produce an inhibitor-resistant beta lactamase like AmpC.
ESBL detection may be masked by high-level production of AmpC. Further, clavulanate may act as an inducer of high-level AmpC resulting in false negativity in ESBL detection by increasing resistance to the screening drugs. As a solution to this problem, tazobactam and sulbactam which are much less likely to induce AmpC β-lactamases are preferred as inhibitors for ESBL detection [5], and fourth generation cephalosporin i.e. cefepime is better choice as an indicator drug [6]. Cefepime is a more reliable detection agent for ESBLs in presence of AmpC β-lactamases because it is minimally affected by high-level AmpC production, so in this study original double disc synergy test and phenotypic disc confirmatory test was compared with modified double disc synergy test (MDDST) using cefepime as indicator drug and piperacillin-tazobactam as inhibitor for ESBL detection.
Materials and Methods
The study was conducted in the Department of Microbiology, Punjab Institute of Medical Sciences, Jalandhar, India. The study was approved by the ethical committee of the instituition. A total of 245 isolates of Escherichia coli (123), Klebsiella spp. (87), Proteus spp.(20), Enterobacter spp.(9) and Citrobacter spp.(6) obtained over a period of 2 years from January 2013 to December 2014 from urine samples of hospitalized patients were studied.
Antimicrobial susceptibility testing
The isolates were tested for antimicrobial susceptibility by disc diffusion method according to CLSI guidelines [7]. The following antibiotics were used; cefotaxime (30μg), cefpodoxime (30μg), ceftriaxone (30μg), cephoxitin (30μg), gentamycin (10μg), amikacin (30μg), ciprofloxacin (5μg), norfloxacin (10μg), nitrofurantoin (100μg) cotrimoxazole (25μg), piperacillin/tazobactam (100/10 μg), meropenem (10μg), and imipenem (10μg). All the antibiotic discs were procured from Hi-media, Mumbai.
Test for ESBL production
All the strains showing diameter of less than 27mm for cefotaxime and less than 25mm for ceftriaxone were selected for checking ESBL production.
Phenotypic confirmatory disc diffusion test (PCDDT)
This test was performed as per CLSI guidelines by using control strains of Escherichia coli ATCC 25922 (beta –lactamase negative) and Klebsiella pneumoniae ATCC700603 (ESBL positive). A >=5mm increase in zone diameter for either ceftazidime or cefotaxime tested in combination with clavulanic acid versus its zone diameter when tested alone confirmed ESBL production [8].
Double disk synergy test (disk approximation test)
This test was done by placing a disc of augmentin (20μg amoxicillin + 10μg clavulanic acid) onto Muellor–Hinton agar on which test inoculum was spread and discs of cefpodoxime (30μg), ceftazidime (30μg) and cefotaxime (30μg); were placed around augmentin disc keeping the distance of 16 to 20 mm from it. (centre to centre). The organisms were considered as ESBL positive when there was enhancement of zone of inhibition around any of these cephalosporin discs towards the augmentin disc [8].
Modified double disk synergy test
The original DDST was modified for detecting ESBLs in AmpC co-producers by placing a disc of piperacillin –tazobactam at a distance ranging between 22 and 25mm from cefepime disc. A disc of augmentin was also placed on the surface of MHA with discs of cefpodoxime, ceftazidime, cefotaxime, and cefepime at a distance ranging between 16 and 20 mm from it.
The isolates showing positive test for ESBL production with any of the three confirmatory tests i.e. PDCT, DDST or MDST were taken as ESBL positive.
Detection of AmpC β-lactamases
Modified three –dimensional test (MTDT)
The presence of AmpC β-lactamases was detected by MTDT [9] after initial screening with cephoxitin (30 μg) disc. Isolates which showed cefoxitin zone diameter <18 mm were considered screen positive for AmpC β-lactamase production [10].
Fresh overnight growth of test organism from MHA was taken in a sterile micro centrifuge tube. Peptone water was added and the bacterial mass was pelleted by centrifugation at 3000rpm for 15 minutes. By freezing and thawing the bacterial pellet for approximately 10 cycles, a crude enzyme extract was prepared. A lawn culture of E.coli ATCC 25922 was prepared on MHA plates and cefoxitin disc (30μg) was placed on the surface of the medium. Linear slits 3cm long were cut using sterile surgical blade upto a point 3mm away from the edge of cefoxitin disc. Wells of 8mm diameter were made on the slits at a distance 5mm inside from the outer end of the slit using a sterile Pasteur pipette. The wells were loaded with enzyme extract in 10 increments until the well was full. Approximately 30-40μl of extract was loaded in a well. The plates were incubated at 37°C overnight. Three different kinds of results were recorded. Isolates that showed clear distortion of zone of inhibition of cefoxitin were taken as AmpC producers. Isolates with no distortion were taken as AmpC non-producers, and isolates with minimal distortion were taken as intermediate strains. A known AmpC-positive isolate of Klebsiella pneumoniae was used as reference strain [9].
ESBL and AmpC co-producers
The isolates which were confirmed as AmpC producers by MTDT and also showed positive test for ESBL production with either of the three confirmatory tests i.e. PDCT, DDST or MDST were taken as ESBL and AmpC co-producers.
Results
A total of 245 isolates obtained from urine cultures included Escherichia coli (123), Klebsiella pneumoniae (87), Proteus spp. (20) Enterobacter spp. (9) and Citrobacter spp (6). All the isolates were screened for both ESBL and AmpC β-lactamase production. Among these, 192 (78.4%) isolates {Escherichia coli (95), Klebsiella pneumoniae (82), Proteus spp. (8) Enterobacter spp. (5), Citrobacter spp (2)} were screen positive for ESBL and 143 isolates (58.4%) {Escherichia coli (78), Klebsiella pneumoniae (56), Proteus spp. (5) Enterobacter spp. (3) and Citrobacter spp (1)} were screen positive for AmpC. Of these192 isolates screened for ESBL, 162 (66.1%) {Escherichia coli (87/123, 70.7%), Klebsiella pneumoniae (65/87,74.7%), Proteus spp. (5/20, 25%) Enterobacter spp. (4/9,44.4%), Citrobacter spp (1/6, 1.7%)} were confirmed positive by either of confirmatory tests used i.e. PDCT, DDST or MDDST [Table/Fig 1]. DDST detected ESBLs in only134 (54.7%) while additional 28 (11.4%) ESBL positive isolates were detected by MDDST. PDCT detected total 145 (59.2%) ESBL positive isolates with cefotaxime and cefotaxime+clavulanate detecting 139 and ceftazidime and ceftazidime+ clavulanate detecting additional 6 isolates. AmpC production was detected in 113(46.1%) isolates by modified three dimensional test {Escherichia coli (63/123, 51.2%), Klebsiella pneumoniae (46/87, 52.8%), Proteus spp. (3/20, 15%) Enterobacter spp. (1/9, 11.1%) and Citrobacter spp (0)} [Table/Fig-1,2]. All the 28 isolates which were additionally detected ESBL producers by MDDST showed positive three dimensional test i.e. AmpC co producers. Hence 28 isolates (11.4%) {Escherichia coli (15), Klebsiella pneumoniae (12), Proteus spp. (1)} were positive for both ESBL and AmpCβ-lactamases [Table/Fig-1] and 64 isolates (26.1%) {Escherichia coli (25), Klebsiella pneumoniae (19), Proteus spp. (12) Enterobacter spp. (3) and Citrobacter spp (5)} were neither AmpC positive nor ESBL positive [Table/Fig-1]. DDST detected ESBL in none of AmpC positive isolates. In MDDST cefepime was the best cephalosporin in detecting ESBL in presence of AmpC production. It showed synergism with amoxicillin-clavulanate in 11 (39.3%) isolates and in 24 (85.7%) isolates with piperacillin –tazobactam [Table/Fig-3]. Third generation cephalosporins -cefotaxime, ceftazidime and cefpodoxime were not able to detect ESBL in AmpC co-producers. Performance of cefpodoxime was poor in detecting ESBL in non AmpC producers also as it showed augmentation with amoxicillin-clavulanate in only 24(17.9%) isolates in DDST while augmentation was seen with ceftazidime in 128 (95.5%) isolates i.e. maximum followed by cefotaxime in118 (88.1%) isolates.
Distribution of ESBLs and AmpC in the isolates
| Organisms | Total isolated | ESBL +ve | AmpC +ve | Both ESBl+ AmpC +ve |
|---|
| Escherichia coli | 123 | 87 (70.7%) | 63(51.2%) | 15(12.1%) |
| Klebsiella | 87 | 65(74.7%) | 46(52.8%) | 12(13.8%) |
| Proteus | 20 | 5 (20%) | 3 (15%) | 1 (5.0%) |
| Enterobacter | 9 | 4 (44.4%) | 1 (11.1%) | 0 |
| Citrobacter | 6 | 1 (1.7%) | 0 | 0 |
| Total | 245 | 162(66.1%) | 113(46.1%) | 28(11.4%) |
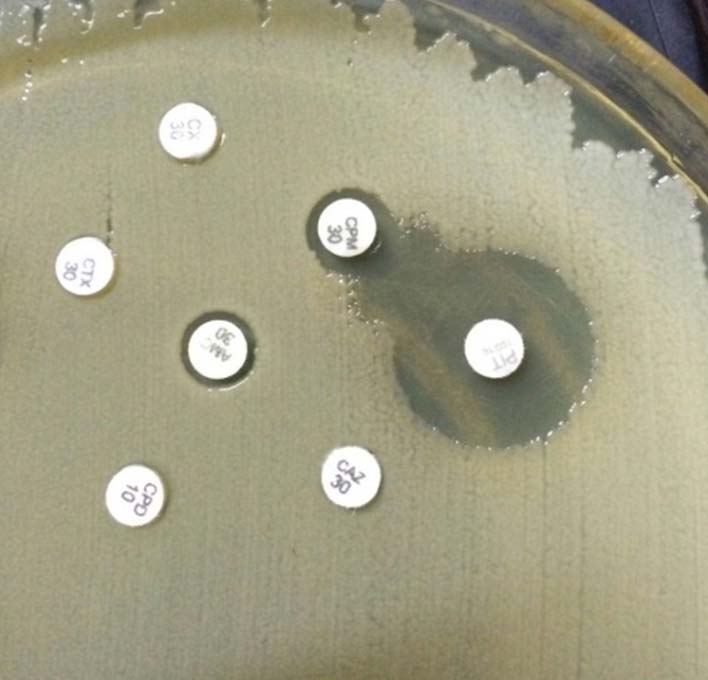
Positive Modified three dimensional test (Enhanced growth of surface organism at the point where slit inserted the zone of inhibition of cefoxitin).

MDDST showing synergism of only cefepime and piperacillin –tazobactum.
Discussion
ESBL producing organisms are of ever increasing concern since their first description more than 20 years ago. Prevalence rate of 35%-85% has been demonstrated in various Indian studies [Table/Fig-4]. A study from Uganda revealed ESBL production in 62% isolates [11]. In Latin America upto 32% of Escherichia coli and upto 58% of Klebsiella pneumoniae isolates are ESBL positive [12]. Systemic infections due to ESBL-producing Enterobacteriaceae were associated with severe adverse clinical outcomes. Primarily characterized in limited bacteria such as Escherichia coli and Klebsiella spp, ESBLs have been spreading and reaching other genera, principally Enterobacter and Proteus spp.
Prevalence of ESBL, AmpC and ESBL + AmpC co-producers in India.
| Place (year of study) | ESBL | AmpC | ESBL+AmpC |
|---|
| New Delhi (2010) [6] | 61.9% | 78.7% | 58.4% |
| Amritsar (2013) [16] | 35.16% | 5.4% | 6.59% |
| Pune (2013) [17] | 40.07% | 14.8% | 9.9% |
| Meerut (2013) [18] | 82.76% | 40% | 84.62% |
| Karnataka (2014) [19] | 85% | 10% | 33% |
| Present study | 66.1% | 46.1% | 11.4% |
Based on their physical properties, more than 300 ESBLs have been identified and they have been found to be inhibited by clavulanic acid, sulbactam and tazobactam. This is the property which helps in their detection in the laboratory. But now, ESBL phenotypes have become more complex due to the production of multiple enzymes including inhibitor-resistant ESBL variants, plasmid-borne AmpC and production of ESBLs in AmpC - producing bacteria. These phenotypes usually exhibit multidrug resistance that is not always detected in routine susceptibility tests. The inability to detect such complex resistance phenotypes is a serious challenge facing clinical laboratories and may have been a major factor in the uncontrolled spread of ESBL-producing organisms and related treatment failures. AmpC- producing organisms can act as hidden reservoirs for ESBLs. So it is important for clinical microbiology laboratories to be able to detect ESBL production in these organisms on a routine basis for epidemiological and therapeutic purposes. AmpC β-lactamases are resistant to β-lactamase inhibitors like clavulanic acid and hence the augmentation in zone diameter in DDST by ESBL producers can be completely masked by AmpC enzymes. In order to detect ESBLs in isolates that co-produce AmpC β-lactamase, modification of DDST by using combination of cefepime and piperacillin-tazobactam or incorporation of inhibitors of AmpC enzyme like boronic acid compounds, cloxacillin and novel inhibitors such as Syn2190 have been recommended [13,14]. The use of cefepime disc in DDST to detect ESBLs in Enterobacter species has also been highlighted by Tzelepi et al [15]. Hence this unique modification of the double-disk test (MDDT) using a combination of cefepime (FEP) and piperacillin-tazobactam (TZP) was evaluated to detect ESBLs and found to be the most sensitive test for ESBL detection in AmpC co-producers (detected 66.1%).
In comparison phenotypic disc confirmatory test detected ESBL production in 59.2% while DDST detected ESBL production in 54.6% and was found to be least sensitive. Similar high sensitivity of MDDST and false negative ESBL results using DDST and PDCT have been reported in earlier studies [8,14].
Although there are no CLSI guidelines for phenotypic methods to screen and detect AmpC, several methods have been developed for detection of AmpC. Reduced susceptibility to cefoxitin is taken as indicator of AmpC production. However, reduced susceptibility to cefoxitin can also be due to reduced outer membrane permeability. A positive three dimensional test with cefoxitin demonstrates hydrolysis of cefoxitin and differentiates between AmpC production and reduced outer membrane permeability. In our study 58.4% isolates were cefoxitin resistant while three dimensional test was positive in 46.1%. Interestingly, MDDST was positive in all the 28 isolates showing positive three dimensional test i.e. AmpC and ESBL co- producers. Cefepime was the best cephalosporin in detecting ESBL in presence of AmpC as it is less affected by AmpC β-lactamases. Cefotaxime and ceftazidime were not able to show any potentiation of zones in presence of β lactamase inhibitor in AmpC co-producers as the AmpC β-lactamase gave a resistant zone to the cephalosporin.
Different prevalence rates of AmpC producing strains (10-80%) have been reported in different Indian studies which can be due to different geographic locations, antimicrobial susceptibility pattern and different detection method (phenotypic or genotypic) [Table/Fig-4]. Enterobacteriaceae co-producing AmpC β-lactamases and extended-spectrum β-lactamases (ESBLs) are also increasingly being reported from India [Table/Fig-4] and abroad. A study from Turkey reported prevalence of ESBL in 46% isolates, only AmpC in 3% isolates and production of both these in 38% isolates [13].
ESBL production coexists with resistance to several other antibiotics. ESBLs are encoded by plasmids, which also carry resistant genes for other antibiotics. Co-resistance to quinolones and aminoglycosides is common. We found such associated resistance with co-trimoxazole (84.2%), gentamycin (79%) and flouroquinolones (90-93%). Sensitivity to imipenem 87% and piperacillin –tazobactum was 80%.
Limitation
Unfortunately, our study was limited by the fact that final confirmation of isolates by genotypic methods could not be carried out due to limited resources. Optimum identification of ESBL producing isolates is essential to formulate policies for empirical antimicrobial therapy, especially in high–risk units where infections due to these organisms are common. While ESBLs are susceptible to β-lactamase inhibitors, AmpC β-lactamases are resistant to clavulanic acid and variably resistant to sulbactam and tazobactam. The drug of choice remains carbapenems in AmpC producers. It also helps in monitoring the development of antimicrobial resistance and in the implementation of proper hospital infection control measures.
Conclusion
The frequency of ESBLs can easily be underestimated in clinical isolates using the current CLSI recommended methods i.e. DDST and PDCT since these organisms often produce multiple β-lactamases. In such situations, where AmpC β-lactamases can interfere with clavulanate synergy, the modification of double disc synergy tests that combine piperacillin-tazobactum with cefepime may increase the possibility of ESBL detection.