A Rare Presentation of Lupus Nephritis Flare up with Posterior Reversible Leucoencephalopathy
S. Hima Mani1, S. M. Shivaprasad2, L. Umesh3
1 Post Graduate Student, Department of Nephrology, Institute of Nephrourology, Bangalore, India.
2 Associate Professor, Department of Nephrology, Institute of Nephrourology, Bangalore, India.
3 Professor and Head, Department of Nephrology, Institute of Nephrourology, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. S. Hima Mani S, D/No 8, Government Doctors Quaters, JLB Cross Road, Behind Regalis Hotel, Mysore -570005, India. E-mail : himamani@gmail.com
Systemic lupus erythematosus (SLE) is associated with various neurologic or psychiatric abnormalities and Posterior Reversible Leuco Encephalopathy Syndrome (PRES) is very rare neurological manifestation in SLE. PRES is associated with various clinical manifestations, like, seizures, visual loss, headaches, vomiting altered mental status and rarely focal neurological deficits. Other predisposing condition associated with PRES is eclampsia, accelerated hypertension, uraemia, transplantation, autoimmune diseases and/or use of immunosuppressive drugs. It is important to recognise PRES since it is a potentially reversible. We describe an unusual case of PRES caused by uraemia during lupus flare up in a patient with biopsy proven class IV lupus nephritis who presented with features of asymmetrical quadriparesis which completely reversed after haemodialysis sessions and treating lupus flare up. In our case she presented with quadriparesis which is a rare presentation and hypertensive encephalopathy was not present.
(HBP) High Blood Pressure, NIH (National Institute of Health), SLE- Systemic Lupus Nephritis
Case Report
A 25-year-old married woman mother of two children with no significant past, family or obstetric history presented with a 2-year history of SLE that included stage IV lupus nephritis, for which she received immunosuppressant’s as per National Institute of Health (NIH) protocol. But after 4 months of initiating the therapy she started taking immunosuppressant’s irregularly and stopped the medication on her own. Current presentation was due to progressive oedema of 1 month duration and subsequently she developed asymmetrical quadriparesis since 2 days which is of upper motor neuron type. Examination revealed Blood Pressure (BP) of 160/98 mm Hg, pedal oedema, facial puffiness, neurological examination revealed quadriparesis with spasticity in limbs, right side spasticity was more than left, hypertonia in all the limbs and extensor plantar response.
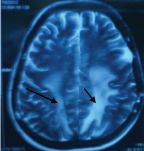
Fundus examination revealed normal and there were no other significant abnormalities in the present case. She had renal failure with uremic symptoms and she also had oliguria with serum creatinine of 6.7mg/dl and received five sessions of haemodialysis. Patient underwent repeat kidney biopsy and it revealed cresentric transformation of class IV lupus nephritis and patient was pulsed with Methyl prednisalone and cyclophospamide. Patient completely recovered from quadriparesis following haemodialysis session, anti oedema and anti hypertensive drugs. Laboratory investigation revealed haemoglobin 7.6gm%, serum creatinine 6.7mg/dl, serum protein 5.8 g/dl, serum albumin 2.9 gm/dl, C3 was low (43mg/dl), C4 was low (12 mg/dl), anti-nuclear antibodies and anti-DNA antibodies were positive, twenty four hours protenuria was 2.4gm /day. MRI revealed bilateral parietal and occipital white matter hyperintensities, which were more pronounced on the left side. Repeat MRI after 10 days revealed complete resolution of the parietal and occipital oedema.
Discussion
Posterior reversible leukoencephalopathy syndrome (PRES) are also called by other names like reversible occipitoparietal encephalopathy, hyperperfusion encephalopathy, posterior leukoencephalopathy, reversible posterior cerebral oedema syndrome or potentially reversible encephalopathy [1].
PRES occurs due to cerebral oedema with diffusion of plasma proteins and cells into the extracellular space. Cerebral oedema occurs due to High BP, direct toxic effect produced by immunosupressive or cytotoxic agents which result in endothelial damage [2–4].
Endothelial dysfunction in SLE occurs due to various reasons like autoimmune damage, ischaemia (thrombosis, vasculitis) or Cytotoxic drugs. Fluid retention and HBP associated with SLE nephritis may predispose for cerebral oedema. Other than SLE conditions commonly associated with PRES are hypertensive encephalopathy, pre-eclamptic toxaemia and eclampsia, renal failure, transfusion, volume overload, use of immunosuppressive or cytotoxic drugs (cyclosporine, tacrolimus, rituximab) intravenous immunoglobulins solid organ transplantation, thrombotic thrombocytopenic purpura, hypercalcaemia, or EPO use, which are commonly encountered in patients admitted in nephrology departments, have also been associated with PRES [5,6]. The clinical presentation of PRES is acute to subacute neurological presentation with features of headache, altered mental status, coma seizures, visual loss and rarely focal neurological signs. HBP is frequent, but not always present. MRI Imaging shows T2-weighted and FLAIR bilateral subcortical and cortical hyperintensities of the white and grey matter with a predominantly posterior distribution, but other areas such as frontal lobes, brainstem, basal ganglia and thalamus can also be involved. The main differential diagnosis of PRES are bilateral ischaemic strokes in the posterior cerebral artery territory, central venous sinus thrombosis, demyelinating disorders, lupus encephalitis, cerebral vasculitis and infectious or metabolic encephalopathy [7–9]. Reversibility of PRES and MRI findings are the main elements to distinguish PRES from other different diagnoses [10]. PRES if treated early it is reversible, delayed diagnosis and treatment may result in incomplete recovery. Results in cerebral infarction, subarachnoid haemorrhage, coma or death have been described. Focal epilepsy could occur in children, cognitive impairment is reported, and white matter oedema can evolve into leukomalacia [11,12]. PRES can also be associated with erythropoietin treatment which is common in dialysis patients [13]. In females pregnancy and the postpartum period often lead to this syndrome when associated with eclampsia, preeclampsia and HELP [14].
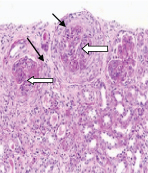
This patient didn’t have high BP, but she had increased disease activity because she had flare up of SLE with renal biopsy revealing cresenteric prolifertive glomerulonephritis (biopsy findings are shown in [Table/Fig-1]) and there was fluid retention which would have triggered PRES in her. This patient had asymmetrical spastic quadriparesis due to PRES (MRI findings of this patient is enclosed in [Table/Fig-2]) but the most common presentation like headache blurred vision and seizures were absent in this case.
Renal biopsy showing Lupus nephitis IV with cresents, activity score 8/24, Chronicity index 2/12. Fibrocellular cresent (black arrow), Global endocapillay proliferation within the glomeruli (white arrow).
MRI- T2/flair hyper intensity in bilateral parieto occipital and fronto parietal region (black arrow) in this patient who was a case of lupus nephritis IV with cresents and PRES.
Immunosuppressants during this episode were given to treat lupus nephritis with flare up of lupus after the occurrence of posterior reversible leucoencephalopathy.
Conclusion
In this patient she completely recovered from quadriparesis within 10 days after haemodialysis sessions and anti oedema treatment. PRES is a rare manifestation of SLE and it could be reversible if the underlying illness is treated completely. Antihypertensive, antiepileptic and haemodialysis is the mainstay of treatment along with supportive care. Hence as it is reversible it has to be recognized and treated at the earliest with proper management.
[1]. Hinchey J, Chaves C, Appignani B, A reversible posterior leukoencephalopathy syndromeN Engl J Med 1996 334:494-500. [Google Scholar]
[2]. Kadikoy H, Reversible encephalopathy syndrome in a patient with lupus nephritis”Saudi J Kidney Dis Trans 2012 23(3):572-76. [Google Scholar]
[3]. El Karoui K, Posterior reversible encephalopathy syndrome in systemic lupus erythematosusndt.oxfordjournals.org/content/23/2/757 [Google Scholar]
[4]. Leroux G, Posterior reversible encephalopathy syndrome during systemic lupus erythematosus: four new cases and review of the literatureLupus 2008 17(2):139-47. [Google Scholar]
[5]. Chen HA, Systemic lupus erythematosus complicated with posterior reversible encephalopathy syndrome and intracranial vasculopathyInt J Rhem Dis 2010 13(4):e79-82. [Google Scholar]
[6]. Kastrup O, Maschke M, Wanke I, Posterior reversible encephalopathy syndrome due to severe hypercalcaemiaJ Neurol 2002 249:1563-66. [Google Scholar]
[7]. El Karoui K, Posterior reversible encephalopathy syndrome in systemic lupus ErythematosusNephrol Dial Transplant 2008 23:757-63. [Google Scholar]
[8]. Stott VL, Hurrell MA, Anderson TJ, Reversible posterior leukoencephalopathy syndrome: a misnomer reviewedIntern Med J 2005 35:83-90. [Google Scholar]
[9]. Brubaker LM, Smith JK, Lee YZ, Haemodynamic and permeability changes in posterior reversible encephalopathy syndrome measured by dynamic susceptibility perfusion-weighted MR imagingAJNR Am J Neuroradiol 2005 26:825-30. [Google Scholar]
[10]. Covarrubias DJ, Luetmer PH, Campeau NG, Posterior reversible encephalopathy syndrome: prognostic utility of quantitative diffusion weighted MR imagesAJNR Am J Neuroradiol 2002 23:1038-48. [Google Scholar]
[11]. Shin KC, Choi HJ, Bae YD, Reversible posterior leukoencephalopathy syndrome in systemic lupus erythematosus with thrombocytopenia treated with cyclosporineJ Clin Rheumatol 2005 11:164-66. [Google Scholar]
[12]. Kur JK, Esdaile JM, Posterior reversible encephalopathy syndrome: an underrecognized manifestation of systemic lupus erythematosusJ Rheumatol 2006 33:2178-83. [Google Scholar]
[13]. Delanty N, Vaughan C, Frucht S, Erythropoietin-associated hypertensive posterior leukoencephalopathyNeurology 1997 49:686-89. [Google Scholar]
[14]. Servillo G, Posterior reversible encephalopathy syndrome (PRES) in critically ill obstetric patientsIntensive Care Medicine 2003 29(12):2323-26. [Google Scholar]