Stellate Ganglion Block (SGB) is an effective technique and may be used to manage upper extremities pain due to chronic regional pain syndrome (CRPS) [1,2]. CRPS is a painful and disabling syndrome with physical changes in the affected extremity.
CRPS has been reported most often in adult population, but it has been reported in paediatric population as well [3]. The sympathetic nervous system plays an important role in sustaining the pain. The incidence of sympathetically mediated pain in CRPS is unknown [4].
Fluoroscopy is a suitable method for identifying bony structures such as C6 and C7 transverse processes. The needle tip should be placed at anterolateral to the longus colli muscle. Also, SGB can be done with ultrasound guidance. Some advantages of the ultrasound guidance includes: facilitating the caudal spread of the injectate, use of a small injectate volume, direct visualization of vascular and soft tissue structures, a more effective and precise sympathetic block [5]. Anterior paratracheal approach previously was the standard technique with serious complication to stellate ganglion block [6]. Fluoroscopic and ultrasound guided block are easy to use and safe methods for SGB [7]. One of the common interventions where the ultrasound guidance is gaining wider acceptance is during the performance of a stellate ganglion block [8]. Stellate ganglion blockade (ultrasound guidance) that recently gained popularity was described in 1995. In comparision with the blind technique, Kapral et al., found that this technique used a lower volume of local anaesthetics and more rapid onsets of Horner’s syndrome [9]. As compared with C7 level, the SGB most commonly done at C6 level because this level is relatively safe and well defined landmarks. However, blockade of SG at this level may result in unsuccessful or fail block. Over all assessments of the different sympathetic blockade by SG have shown that C7-SGB is more effective than C6-SGB [7,10]. Abdi and others described an oblique fluoroscopic approach targeting the junction between the transverse process and the vertebral body at the C7 level (uncinate) to block SG effectively and avoiding vascular injury [11].
The purpose of this prospective study was to evaluate the effectiveness of ultrasound guide SGB by comparing with the fluoroscopic guided SGB in upper extremities CRPS patients in reducing pain and dysfunction of the affected limb.
Materials and Methods
After the approval of ethics committee (reference number: 93-02-30-24632-103514 of Iran University of Medical Sciences on 2014.07.23) and IRCT registration number 2012081410599N1, 14 patients with sympathetic complex regional pain syndrome in upper extremities who were visited in pain clinic of Rasool Akram Teaching Hospital, Tehran Iran were included. Inclusion criteria was as follows: Type1 and 2 CRPS. Exclusion criteria were as follows: anticoagulant therapy, pneumothorax or pneumonectomy an other side, recent MI, glaucoma and cardiac conduction anomaly. Informed consent was signed by all of the patients before performing any procedure.
Patients in a randomized method with block randomization divided in two groups (with ultrasound or fluoroscopic guidance). We had two groups with seven patients in each group.
The purpose of the study is the pain relief and rise the temperature in the affected limb. Fourteen patients with upper extremities sympathetic pain were candidates for stellate ganglion block with block randomization divided in two, 7 patients groups. First group was blocked under fluoroscopic guidance and second group blocked under ultrasound guidance. The final aim after stellate ganglion block was Visual Analogue Scale <3 during minimal daily activities.
Fluoroscopic Technique: In our practice, fluoroscopy is used to confirm contrast spread and correct placement of the needle by anteroposterior and lateral views. After signing informed consent by the patient, the patient stayed in supine position. A skin wheal is made over the anterolateral aspect of the body of C6 with 1 mL of local anaesthetic with a 25-gauge needle. A 22-gauge B-bevel needle is inserted through the skin wheal to contact the body of C6 in the ventrolateral aspect, it is at the junction of the transverse process with the vertebral body (uncinate process) . The needle tip is positioned deep to the anterior aspect of longitudinal ligament. Lateral to the needle tip is longus colli muscle. The needle should be stabilized with a clamp or haemostat. An extension tube should be attached to the needle and used for injection. After negative aspiration, approximately 1 mL of water-soluble contrast solution (Omnipaque 300, GE healthcare, US) is injected. Dye should spread around the longus coli muscles, but should not spread intravascular, epidural, intrathecal, thyroidal or myoneural. If the aspiration is negative, 0.5 to 1 mL of solution is administered, and the patient is asked to raise the thumb to indicate the absence of adverse symptoms. Repositioning of the needle is necessary, if any paresthesia of the arm or hand be elicited. Blood or cerebrospinal fluid aspiration also needs repositioning of the needle. This finding should always be interpreted as the needle has been placed deeper to the anterior tubercle, adjacent to the C6 nerve root. After correct positioning of the needle, a mixture of 5 ml of bupivacaine 0.25% and 1 mL of of triamcinolone (40 mg/mL) was injected. The patient should be informed properly before starting and reminded during the blockade procedure that talking may cause movement of the neck musculature and that needle dislodging from its proper position and thereby some difficulties.
Ultrasound Technique: In this technique, the patient’s position was the same as fluoroscopic technique so, after signing informed consent the patient stayed in supine position. After preparation of the area, the transverse process of C6 was identified. Under complete aseptic technique, a 22-gauge blunt needle is used, via in-plane technique aimed toward the identified target under continuous ultrasound guidance. The patient should be informed properly before starting the procedure, keep calm and immobile during the blockade procedure because talking may cause movement of the neck musculature and cause needle dislodging from its proper position and thereby can lead to some difficulties. After the skin and subcutaneous tissue penetration and needle stabilization, a linear-array (3 to 12-MHz) is used to verify the correct position of the needle. The needle may be directed toward the thyroid tissue anteriorly and the oesophagus posteriorly. At this point, the needle is withdrawn, it is reinserted obliquely and should then be advanced with real-time US imaging. The needle tip will lie anterior to the longus colli muscle. If the aspiration is negative, 0.5 to 1 mL of solution is administered, and the patient is asked to raise the thumb to indicate the absence of adverse symptoms. Repositioning of the needle is necessary, if any paresthesia of the arm or hand be elicited. Blood or cerebrospinal fluid aspiration also needs repositioning of the needle. After correct positioning of the needle, a mixture of 5 ml bupivacaine 0.25% and 1 mL of triamcinolone (40 mg/mL) was injected. Then weekly pain attacks, VAS (by ruler) before and after procedure, pain intensity, disability improvement and occurrence of any complications were assessed in a timely manner and recorded in the previously prepared questionnaire by the second colleague who was not aware of the patient’s group. In order to defeat patients and investigators from discovering treatment allocation once the study is underway and after the study has concluded we used sealed envelopes from each patient which were selected before entering them in the operation theater, third person who was not involved in the process of investigation was recording the results. We used Double Blinding, (both the participant and the investigator).
The Pain Disability Index (PDI) used for disability assessment which a simple and rapid instrument for measuring the impact that pain has on the ability of a person to participate in essential life activities. PDI can be used to evaluate patients, monitor them over time and to judge the effectiveness of interventions [12].
Disability score measurement performed from zero to seventy by using PDI. It has seven items which are: family and home responsibilities, recreation, social activity, occupation, sexual behaviour, self-care and life-support activity.
The purpose of the study is the pain relieves and rise the temperature in the affected limb. The final aims after stellate ganglion block was VAS<3 during minimal daily activities. VAS was measured by other person who was not aware of the group of the study in the recovery room, one week later and one, three and six month later.
Statistical Analysis
Study data were gathered and included into the SPSS (IBM statistics) 20.0 software. Data remained blinded until all data were collected. Quantitative variables were presented as mean± standard deviation and qualitative variables were presented as count and percentages. Independent sample t-test and chi-square were used for statistical analysis to compare numerical and categorical data, respectively, between the two groups if they had a normal distribution. Data without normal distribution were analysed through nonparametric equivalents of the mentioned tests. Repeated-measures analysis of variance (ANOVA) was used to review the results at different time points. All results of statistical tests lower than 0.05 were assumed as significant results.
Results
We studied 14 patients with upper limb CRPS. The patients randomly divided into two groups. Seven patients were undergone stellate ganglion block with fluoroscopic guidance and seven patients undergone stellate ganglion block with ultrasound guidance. The data represent a meaningful statistical difference in terms of the weekly pain attacks in fluoroscopic and ultrasound groups before the block until six months after block, p-values were 0.002, 0.001 respectively.
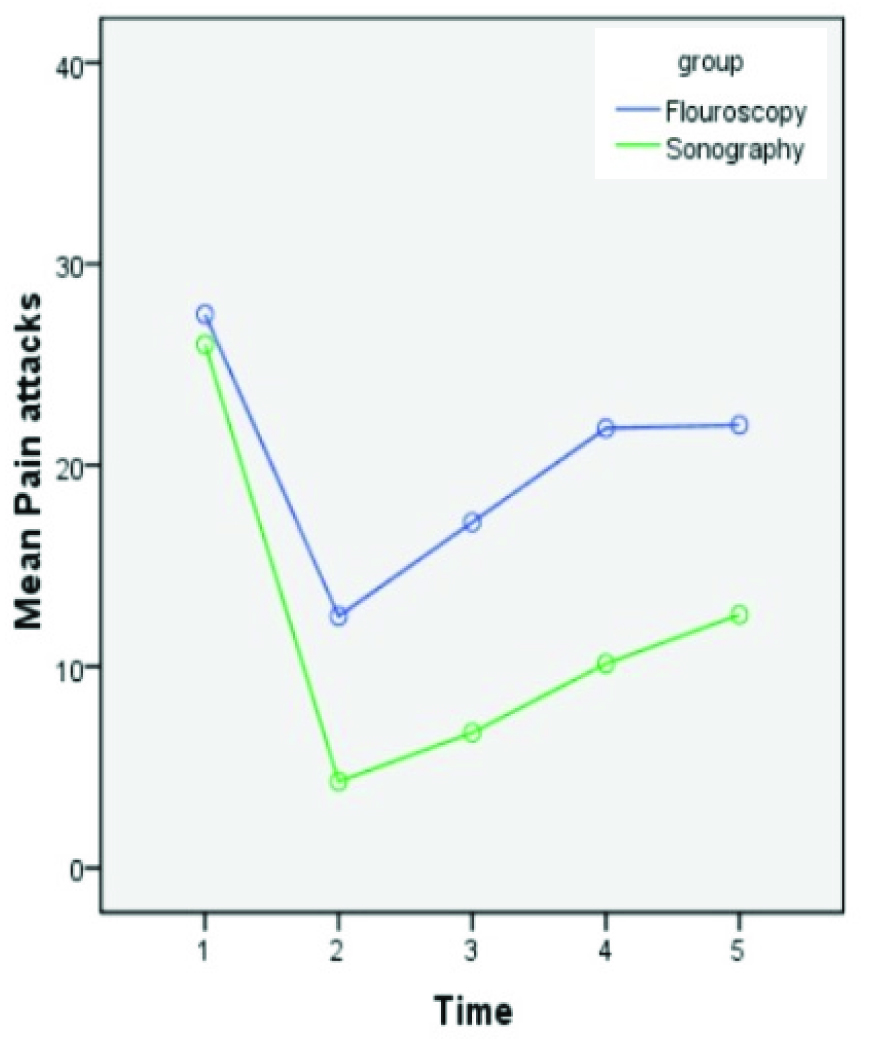
In evaluating the differences between the two groups in terms of the weekly pain attacks, data showed the next p-values: before blocks P-value = 0.33, P-values one week, one, three and six month after the block were 0.061, 0.059, 0.04 and 0.089 respectively. These data represent no meaningful statistical difference between the two groups in terms of the weekly pain attacks [Table/Fig-1].
The mean weekly pain attacks before and after the block until six months lfollow up (1-5, one before the block and 2-5 one week and one, three and six months after the block respectively)
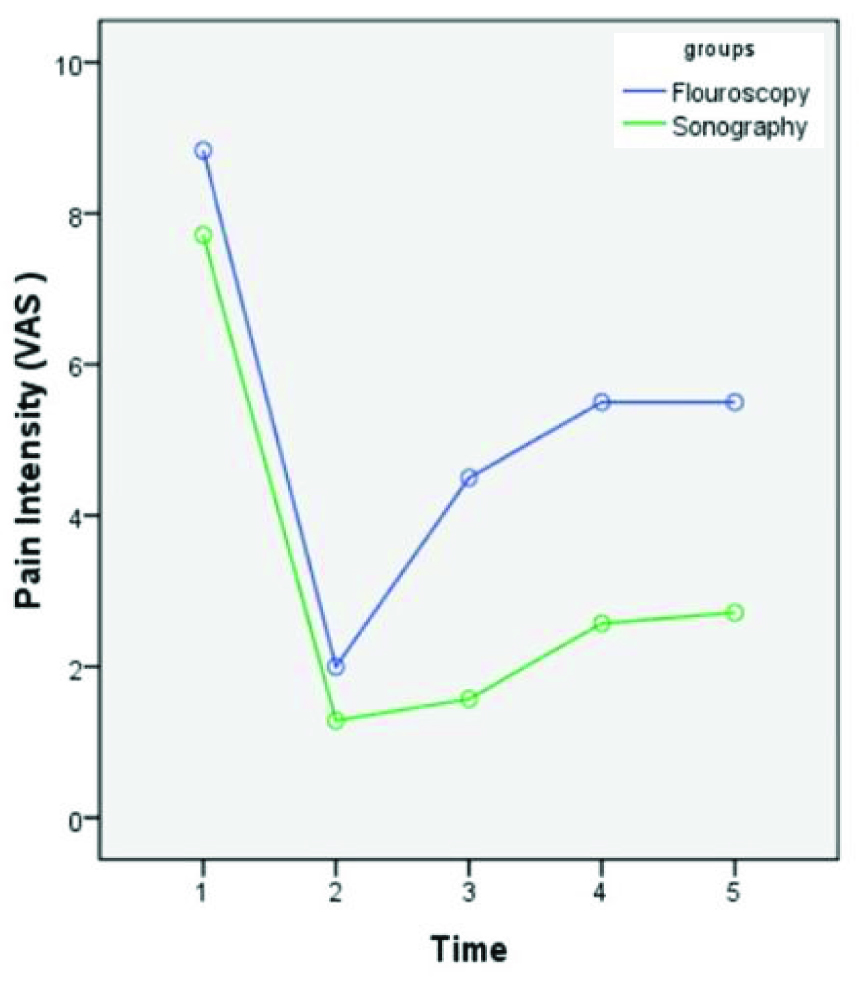
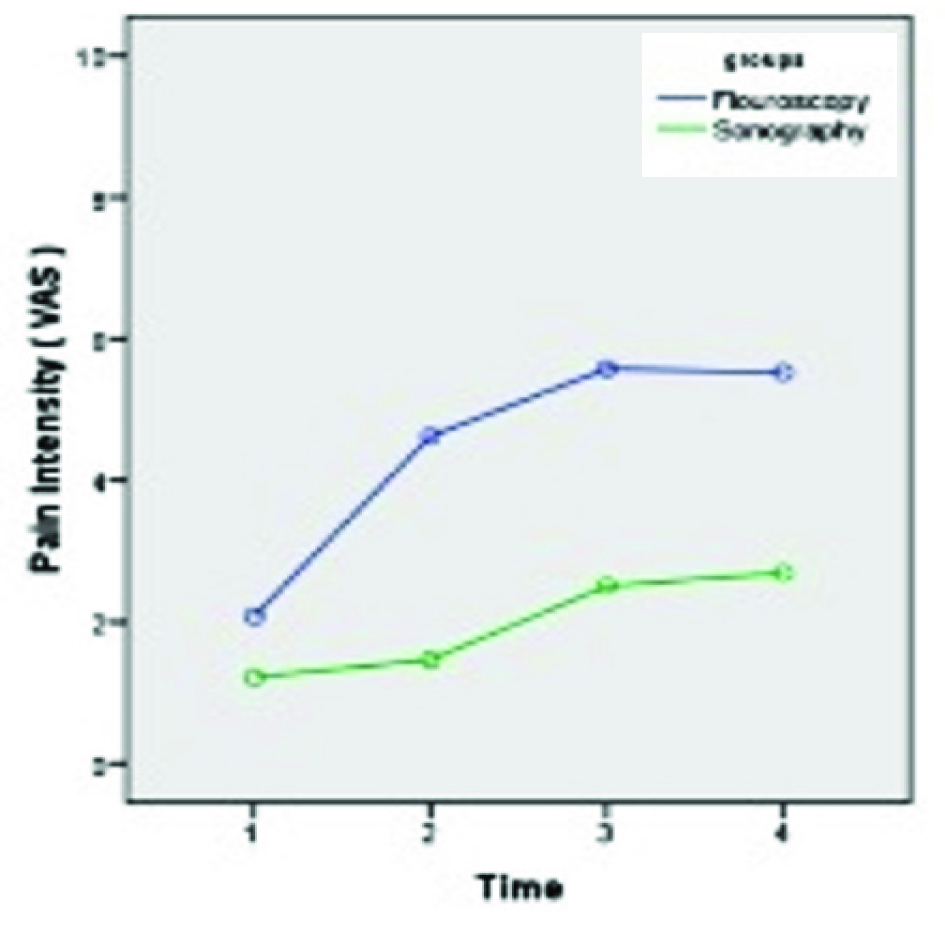
The data represent no meaningful statistical difference between the patients of any group in terms of the pain intensity (p-value = 0.61). There was a borderline correlation between the two groups from one week to six months after block (p-value = 0.06). These data represent a meaningful statistical difference among patients of any group and between the two groups in terms of the pain intensity, p-values were 0.001, 0.031 respectively [Table/Fig-2,3].
The pain intensity before and after the block until six months later (1-5, one before the block and 2-5 one week and one, three and six months after the block respectively)
The pain intensity during attacks after the block until six months later followup (1-4, one week and one, three and six months after the block respectively)
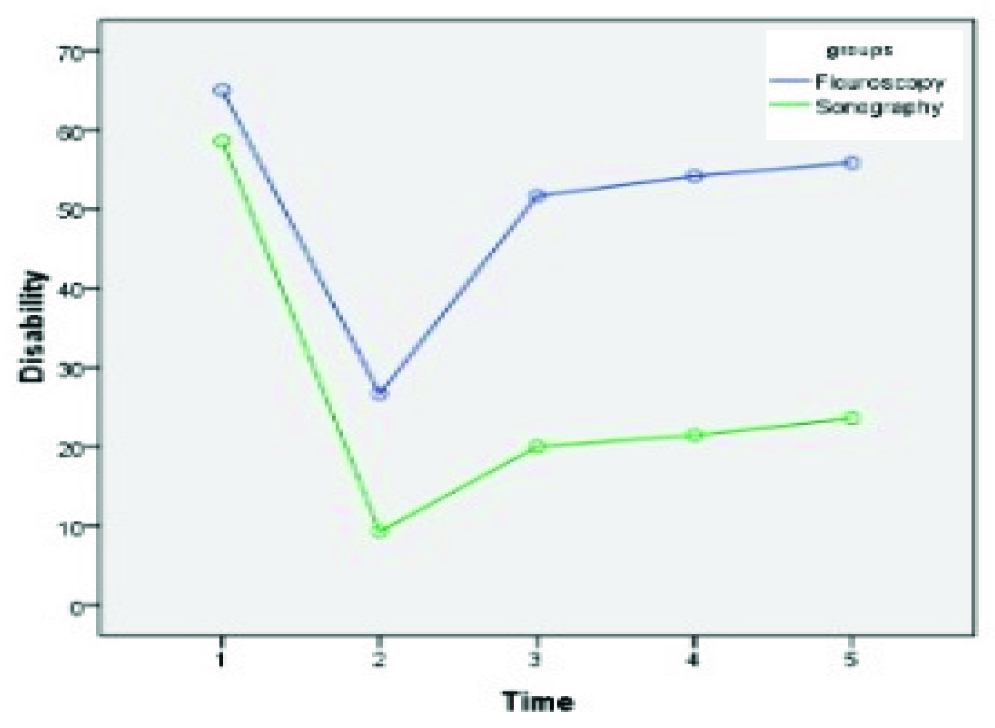
Disability improvement: The mean score of PDI before the blocks in the fluoroscopy group was 45 out of 70 and in the sonography group was 42 out of 70 (p-value =/0.08). By examining the difference between the mean score of disability from the time before the block until six months later, p-value was 0.001. There was a meaningful statistical difference between two groups at the same time (p-value = 0.05). Though reducing the mean score of disability and continuation of this reduction was better seen in sonography group [Table/Fig-4].
The mean disability score before and after the block until six months later (1-5, one before the block and 2-5 one week and one, three and six months after the block respectively).
Basal and half hour after block temperature in affected limb, in the fluoroscopic group (measured by contact thermography) was 32°c and 34.7°c respectively. (p-value = 0.93). In the ultrasound group, the mean basal and half hour after block temperatures of affected limb (measured by contact thermography) was 32°c and 34.65°c respectively. (p-value = 0.84)
These data represent a meaningful statistical difference between the patient of fluoroscopic and ultrasound group in mean basal and half hour after block temperatures of affected limb (p-value = 0.026).
The temperature differences of upper arms: Although the mean differences in temperature elevation in upper arms in ultrasound group was more obvious, but there is not meaningful statistical differences between them. (p-value = 0.27). The occurrence of any possible unpleasant effects was as follows in [Table/Fig-5]. By using χ2 test for statistical analysis, a meaningful correlation between groups, with p-value 0.007 was seen and this means that the two groups in terms of the complication are statistically different. Sex and age distribution between two groups was as follows in [Table/Fig-6,7]. The mean age in fluoroscopic and ultrasound groups was 47.71 and 51.14 respectively. There was no meaningful correlation between two groups (p-value 0.71).
Possible unpleasant effects
| Unpleasant Effects | Fluoroscopic Group | Ultrasound Group |
|---|
| Eyes and nasal congestion | 6 | 1 |
| Horner Syndrome | 2 | 1 |
| Nasal congestion | - | 1 |
| Eye congestion | - | 1 |
| Hoarseness | 3 | - |
| Hypotension | 3 | 2 |
| Hyperemia of the forearm and hand | 3 | 1 |
| Dysrhythmia | 1 | - |
| myosis | - | 1 |
Sex distribution between two groups
| group | Sex | Frequency | percentage |
|---|
| Flouroscopic | male | 3 | 42.9 |
| female | 4 | 57.1 |
| Ultrasound | male | 3 | 42.9 |
| female | 4 | 57.1 |
Age distribution between two groups
| group | Mean age | Standard deviation | p-value |
|---|
| Fluoroscopic | 47.71 | 18.2 | 0.71 |
| ultrasound | 51.14 | 16.26 | |
Discussion
Stellate ganglion block (SGB) is an effective technique used to manage upper extremities pain due to chronic regional pain syndrome (CRPS) [12]. Two image guided SGB are fluoroscopic and ultrasound guided block. This technique is now the practical and appropriate choices for SGB and are easy to use and also provide safety [7]. Ultrasound guidance for pain interventions is becoming widely recognized as a useful imaging tool. One of the common application of this machine which is gaining significant acceptance is during the administration of a stellate ganglion block [8].
The SGB is administrated at C6 most commonly because this level is relative safe with well defined landmarks. Because of specific anatomical position of stellate ganglion, inadvertent placement of the needle into the vertebral artery, thyroid, neural tissues, or oesophagus can occur with the fluoroscopic or blind approach. Fluoroscopy is a reliable method for identifying boney structures, while ultrasound may identify the vertebral vessels, thyroid gland and vessels, nerve roots and the oesophagus and may prevent inadvertent placement of the needle into these structures. Nauroze et al., mentioned that real-time ultrasound imaging prevented inadvertent injury to the oesophagus as well as the thyroid gland and vessels. This may be particularly useful in the patient with asymptomatic pharyngoesophageal diverticulum (Zenker diverticulum) [13]. In the current study we found less unpleasant effects such as dysrhythmia, nasal congestion and hoarsness in the US guided group.
The primary goal of this study was to evaluate the effects of US or fluoroscopic guided SGB treatment on CRPS management. Pain reduction and functional improvement of upper extremity occured in both groups. In the recent years by introducing the US machine in the regional anaesthesia and pain management field and with widespread effectiveness of this tool in medical practice there are growing tendency toward, using this device especially in pain management and with the algorhythmic approach to the chronic pain syndromes there are lots of effort for choosing safer equipment’s both for the physician and the patient, so using appropriate interventions according to enough evidences have found better acceptance [14,15].
For enhancing the accuracy of SGBs to prevent the serious side effects different imaging devices are used [16]. Computerized tomography and MRI are considered to be time-consuming and expensive. Fluoroscopy has gained popularity, but this technique still cannot prevent improper injections into other important anatomical structures. Unfortunately up to now, there are limited studies on the efficacy of US in the setting of performing SGB.
In one study performed by Yucel et al., stellate ganglion blockade under fluoroscopic guidance successfully decreased VAS and increased ROM of wrist joints in patients with CRPS [17]. These findings are comprable with the results of our study.
In one study, performed by Yoo et al., they reported that US-guided SGB successfully relieved pain in patients with CRPS following stroke, as indicated by a significant reduction in VAS values for all patients following the block [4]. Their finding is comparable with the results of the current study. This study is one of the limited studies which exist regarding the usefulness of US guided SGB in CRPS patient’s treatment.
In other study by Jung in 2011, lesser volumes of local anaesthetics for US guided SGB has been evaluated and found that using 4 ml of local anaesthetic can be effective, this is compatible with our results which we had better outcome in US group by using 5 ml of local anaesthetic [18].
So to sum up, US-guided stellate ganglion block may improve the efficacy and safety of the procedure by direct visualization of the related anatomical structures and accordingly the risk of vessels or vital organ injury may be minimized. Also, ultrasound guidance will allow direct monitoring of the spread of the local anaesthetics. It is speculated that US guided SGB minimizes the chance of intravascular injection, minimizes the chance of oesophageal perforation and probably reduces the volume of local anaesthetics needed to cover lower cervical through upper thoracic areas.
Limitation
The major limitation of our research was the low sample size. We recommend further research with large sample size in an other academic center.
Conclusion
According the above mentioned data, in comparison with fluoroscopic guidance, stellate ganglion block under ultrasound guidance is a safe and effective method for upper extremities CRPS with lower complication and better improvement in patient’s disability score.
Finally, we stated the need for further studies.