A Case Report of Metronidazole Induced Neurotoxicity in Liver Abscess Patient and the Usefulness of MRI for its Diagnosis
Shruti Chandak1, Arjit Agarwal2, Arvind Shukla3, Pawan Joon4
1 Associate Professor, Department of Radiodiagnosis, Teerthanker Mahaveer Medical College, Moradabad, Uttar Pradesh, India.
2 Assistant Professor, Department of Radiodiagnosis, Teerthanker Mahaveer Medical College, Moradabad, Uttar Pradesh, India.
3 Professor, Department of Radiodiagnosis, Teerthanker Mahaveer Medical College, Moradabad, Uttar Pradesh, India.
4 Junior Resident, Department of Radiodiagnosis, Teerthanker Mahaveer Medical College, Moradabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:Dr. Shruti Chandak, Associate Professor, Department of Radiodiagnosis, Teerthanker Mahaveer Medical College, Moradabad-244001, Uttar Pradesh, India.
E-mail: chandakshruti@yahoo.com
Metronidazole is a very widely used drug for the treatment of multiple ailments caused by anaerobic bacteria as well as some protozoan parasites. Though its usual side effects are not very serious, yet sometimes it may cause profound adverse effects like neurotoxicity. We present here a case of liver abscess. The patient was treated for a long time with metronidazole and developed sudden onset neurotoxicity which was diagnosed by MRI. The present case also highlights the need of vigilant monitoring of patients on metronidazole for symptoms of neurotoxicity and the usefulness of MRI for diagnosis of the same.
Dentate nucleus, Liver abscess, Metronidazole toxicity, MRI brain
Case Report
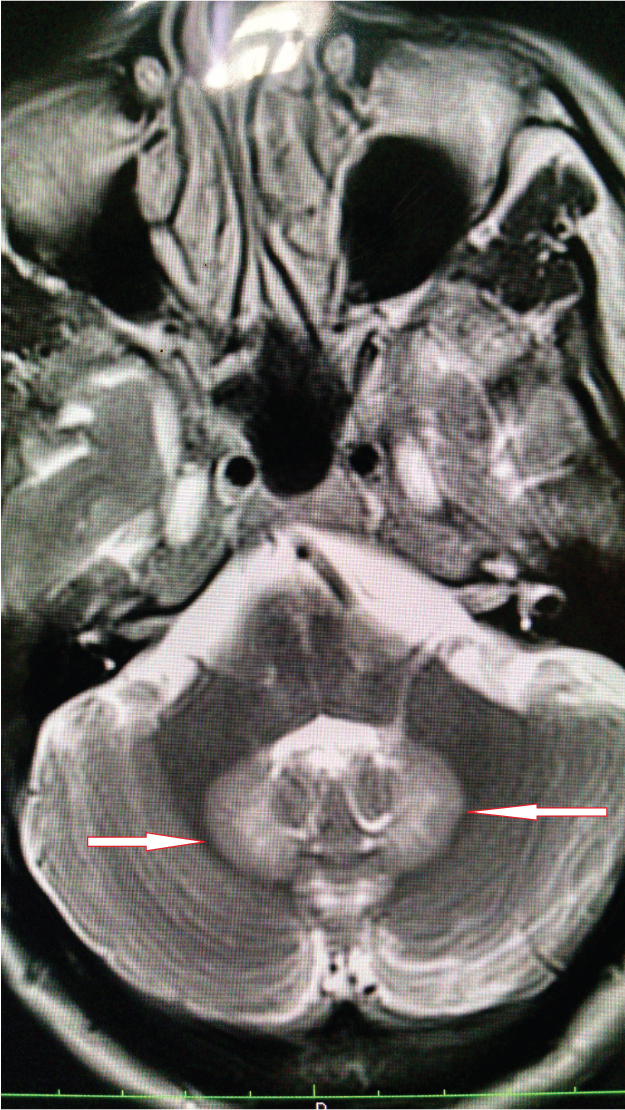
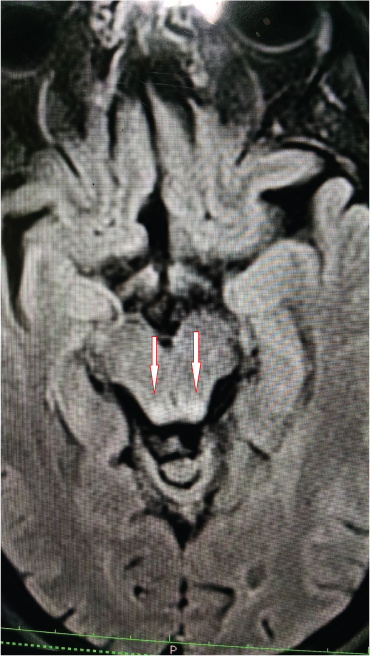
A 45-year-old male patient presented with sudden onset of vertigo, ataxia and slurring of speech since 2 days. The patient was a known case of liver abscess and was treated with percutaneous pigtail catheter drainage elsewhere and oral as well as parenteral antibiotics and was discharged after improvement in symptoms. He was treated with intravenous metronidazole in a dose of 800ml intravenous three times a day for 5 days followed by 800mg orally three times a day for 3 weeks as per his discharge summary. After one month, he came to our hospital with cerebellar symptoms as described above. On examination the patient had staccato speech, restriction of lateral gaze of both eyes and positive cerebellar signs like dysdiadochokinesia and positive Romberg’s sign. The patient was referred to Radiology department for MRI brain which showed symmetrical hyperintensities in bilateral dentate nuclei and tectum on T2W & FLAIR sequences [Table/Fig-1,2, and 3].
T2W axial image showing hyperintensity in bilateral dentate nuclei
FLAIR axial image showing hyperintensity in bilateral dentate nuclei

FLAIR axial image showing symmetrical hyperintensity in tectum
Follow up MRI done three days after cessation of the drug showed significant resolution of the lesions [Table/Fig-4,5]. The patient was also clinically better and was discharged after doing an ultrasound which showed a resolving liver abscess.
FLAIR axial image taken three days after cessation of drug showing significant resolution of hyperintensity in bilateral dentate nuclei

FLAIR axial image taken two days after cessation of drug showing significant resolution of hyperintensity in tectum

Discussion
Metronidazole, an antiparasitic and antibacterial compound, is one of the world’s most widely used drugs [1]. Liver abscesses are caused by bacterial, parasitic, or fungal infection [2]. Out of these amoebic and pyogenic abscesses are most common. For pyogenic liver abscesses, it is recommended that empirical broad spectrum parenteral antibiotic treatment should be started as soon as an abscess is diagnosed which should include penicillin, an aminoglycoside, and metronidazole. Ninety five per cent of uncomplicated amoebic abscesses resolve with metronidazole alone [2]. Hence metronidazole is the mainstay of antibiotic treatment of liver abscesses. However, inappropriate use of metronidazole in excessive doses can give rise to neurological problems such as ataxia, seizures, peripheral neuropathies, cerebellar signs and symptoms, and encephalopathy [3].
Metronidazole is widely used in the treatment of a variety of infections. Some therapeutic indications require prolonged treatment with metronidazole [4]. It has few adverse reactions, most commonly nausea, dry mouth, vomiting, and diarrhea. Neurotoxicity is rare and includes peripheral neuropathy, headache, dizziness, syncope, vertigo, and confusion. Cerebellar toxicity is a very unusual manifestation of metronidazole therapy [5]. The duration of treatment with metronidazole before cerebellar symptoms manifest is variable, and cumulative doses range from 25 g to 110 g [6].
The imaging findings of metronidazole toxicity were first described by Ahmed et al., as fairly symmetric abnormal signal within supratentorial white matter, including the corpus callosum, and within the cerebellum, including the cerebellar deep gray matter nuclei [7]. It has been proposed that axonal swelling with increased water content causes the MRI changes due to T2 prolongation, hence accounting for the rapid reversibility of the changes upon cessation of the drug [7]. Binding of metronidazole to RNA, DNA and inhibitory neurotransmitters, as well as inducing both vasogenic and cytotoxic ooedema are the speculated mechanisms for neurotoxicity [8]. Genetic susceptibility may play a role [9].
MRI plays an important role in the diagnosis and follow-up of these cases. Increased signal intensity is observed on T2W/FLAIR sequences [3] as seen in our patient. It may also have a prognostic value in predicting the symptomatic improvement. Since our patient had few lesions without involvement of corpus callosum, he improved within three days of cessation of metronidazole. The typical locations of lesions in metronidazole induced encephalopathy are the cerebellar dentate nuclei, tectum, red nucleus, and tegmentum around periaqueductal gray matter, dorsal pons and medulla and splenium of corpus callosum. The lesions are bilaterally symmetrical [8]. The inferior olivary nucleus and the white matter of the cerebral hemispheres are uncommon locations [10]. Our patient had lesions only in the dentate nuclei bilaterally and tectum. The signal intensity changes observed on the diffusion weighted images most likely represent interstitial oedema except for the splenium of corpus callosum where it could represent cytotoxic oedema [11].
The differential diagnosis of bilateral symmetric T2 hyperintense lesions in dentate nuclei is methyl bromide intoxication, maple syrup urine disease and enteroviral encephalomyelitis [3].
The diagnosis of metronidazole encephalopathy is made by MRI findings in conjunction with clinical findings and treatment history of patient. With cessation of metronidazole treatment, the imaging findings and clinical symptoms resolve [12]. Metronidazole should be used with some caution and with clear indications especially during prolonged courses and when prescribed in relatively large doses [13]. Since patients with liver dysfunction are more prone for the neurotoxicity of metronidazole, physicians should pay attention to this possible neurological side effect [14].
Conclusion
It is very important to monitor patients who are on high dose metronidazole therapy for a long time for neurotoxicity. MRI is an indispensable tool for the diagnosis of the same. It is also very important to keep in mind the neurotoxicity of the drug and prevent unjudicious use as much as possible.
[1]. Khalil WK, Mahmoud MA, Zahran MM, Mahrous KF, A sub-acute study of metronidazole toxicity assessed in Egyptian Tilapia zilliiJ Appl Toxicol 2007 27(4):380-90. [Google Scholar]
[2]. Krige JEJ, Beckingham IJ, Liver abscesses and hydatid diseaseBMJ 2001 322(7285):537-40. [Google Scholar]
[3]. Kalia V, Vibhuti Saggar K, Case report: MRI of the brain in metronidazole toxicityIndian J Radiol Imaging 2010 20(3):195-97. [Google Scholar]
[4]. Kapoor K, Chandra M, Nag D, Paliwal JK, Gupta RC, Saxena RC, Evaluation of metronidazole toxicity: a prospective studyInt J Clin Pharmacol Res 1999 19(3):83-88. [Google Scholar]
[5]. Kim H, Kim YW, Kim SR, Park IS, Jo KW, Metronidazole-induced encephalopathy in a patient with infectious colitis: a case reportJournal of Medical Case Reports 2011 5:63 [Google Scholar]
[6]. Chakrabarti S, Pan K, Metronidazole-induced encephalopathy: an uncommon scenarioNZMJ 2014 127(1393)ISSN 1175 8716 [Google Scholar]
[7]. Ahmed A, Loes DJ, Bressler EL, Reversible magnetic resonance imaging findings in metronidazole-induced encephalopathyNeurology 1995 45:588-89. [Google Scholar]
[8]. Iqbal A, Tripathi K, Rai M, Dwivedi AN, Clinical and imaging perspective and unanswered questions in a case of metronidazole induced encephalopathyAnn Indian Acad Neurol 2013 16(4):569-71. [Google Scholar]
[9]. Chacko J, Pramod K, Sinha S, Saini J, Mahadevan A, Bharath RD, Clinical, neuroimaging and pathological features of 5-nitroimidazole-induced encephalo-neuropathy in two patients: Insights into possible pathogenesisNeurol India 2011 59:743-47. [Google Scholar]
[10]. Kim E, Na DG, Kim EY, Kim JH, Son KR, Chang KH, MR Imaging of Metronidazole-Induced Encephalopathy: Lesion Distribution and Diffusion-Weighted Imaging FindingsAJNR 2007 28:1652-58. [Google Scholar]
[11]. Mulcahy H, Chaddha SKB, MRI of Metronidazole-Induced EncephalopathyRadiology Case Reports. [Online] 2008 3:239 [Google Scholar]
[12]. Reaven L, Reaven R, Kouo T, Shin R, Metronidazole Toxicity: A Case Serieshttp://www.neurology.org/cgi/content/meeting_abstract/78/1_MeetingAbstracts/P04.15 [Google Scholar]
[13]. Gupta AK, Agarwal MP, Avasthi R, Bhadoria DP, Rohatgi N, Metronidazole-Induced NeurotoxicityJAPI 2003 51 [Google Scholar]
[14]. Yamamoto T, Abe K, Anjiki H, Ishii T, Kuyama Y, Metronidazole-Induced Neurotoxicity Developed in Liver CirrhosisJ Clin Med Res 2012 4(4):295-98. [Google Scholar]