Prenatal Diagnosis of Umbilical Artery Aneurysm with Good Fetal Outcome and Review of Literature
Neetha M Vyas1, Lakshmi Manjeera2, Supriya Rai3, Sharath Devdas4
1 Associate Professor, Department of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, Nitte University, Mangalore, Karnataka, India.
2 Professor, Department of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, Nitte University, Mangalore, Karnataka, India.
3 Professor, Department of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, Nitte University, Mangalore, Karnataka, India.
4 Postgraduate Student, Department of Obstetrics and Gynaecology, K.S. Hegde Medical Academy, Nitte University, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neetha M Vyas, Ashraya 1st Main, 3rd Cross, Subashnagar, Mangalore-575001, Karnataka, India.
E-mail: nvyas_21@yahoo.com
Umbilical artery aneurysm is a rare condition. Till date, 14 cases are reported and only 4 had good fetal outcome. Umbilical artery aneurysm is associated with high risk of fetal aneuploidy and fetal demise. Though umbilical cord anomalies are rare, they are associated with significant fetal morbidity and mortality. We report a case of umbilical artery aneurysm which was detected at 33 weeks of gestation on ultrasonography as an anechoic cyst close to cord insertion with turbulent blood flow in it. The patient was hospitalized and with intensive fetal surveillance and early delivery, a live born fetus was achieved. Baby’s karyotype was normal. Pathologic examination confirmed umbilical artery aneurysm close to cord insertion.
Fetal morbidity, Trisomy, Umbilical cord anomaly
Case Report
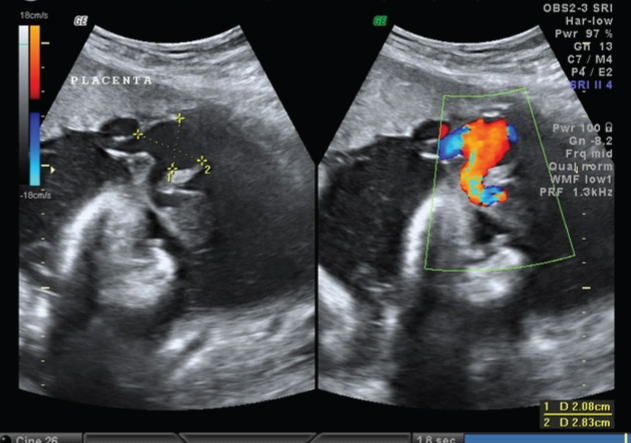
A 22-year-old primigravida at 33 weeks of gestation visited the department of OBG for routine antenatal check up. Prior checkups were done at some other center where ultrasonography done at 20 ad 30 weeks did not show any abnormality. As a routine, growth scan was done in our center which showed a single live fetus of 32 weeks, normal liquor, estimated fetal weight of 1.8kg, placenta was situated in upper segment and near the cord insertion an anechoic cyst of 2x2.8cm in communication with umbilical artery was seen. Doppler showed turbulent blood flow in umbilical artery [Table/Fig-1] with raised indices (S/D – 6.7; RI-0.7 & PI-1.3) and middle cerebral artery indices were normal. Patient was admitted for intensive fetal monitoring.
Anechoic cyst near the cord insertion to the placenta and doppler showing turbulent flow in it
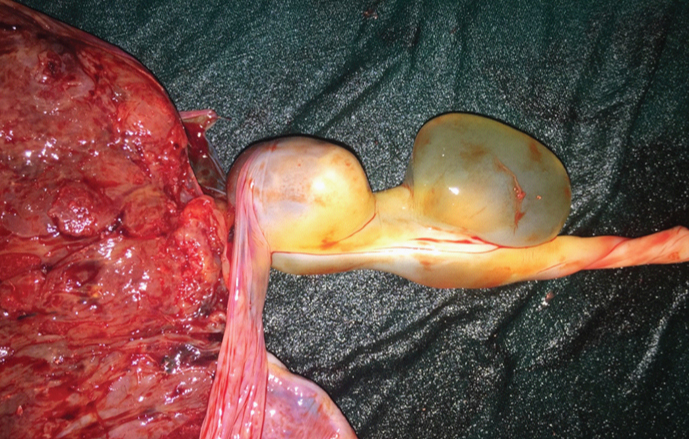
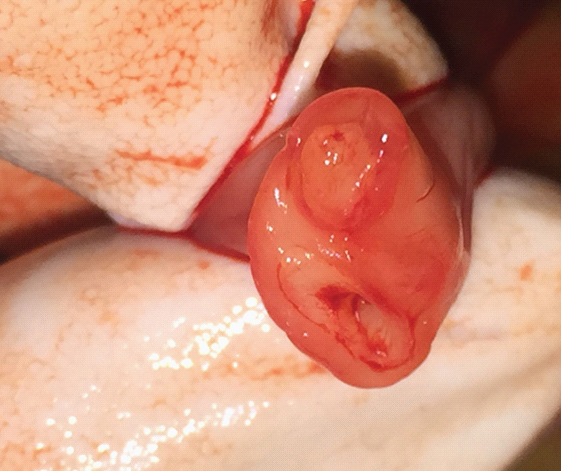
Antenatal corticosteroids were given for fetal lung maturity. Serial ultrasound showed no fetal growth and Doppler assessment showed no changes in umbilical artery indices. Elective cesarean section was done at 36 weeks. A female baby of 1.98 kg was born & baby’s karyotype was normal. Grossly, placenta was triangular in shape with marginal attachment of umbilical cord. Two cystic lesions were noted close to the insertion of the cord to the placenta of 2x2cm each [Table/Fig-2]. Cord length was short around 25cm and two vessel cord was seen on cross section [Table/Fig-3].
Gross picture of umbilical artery aneurysm close to cord insertion and wharton’s jelly (pseudocyst) adjacent to it
Two vessel umbilical cord
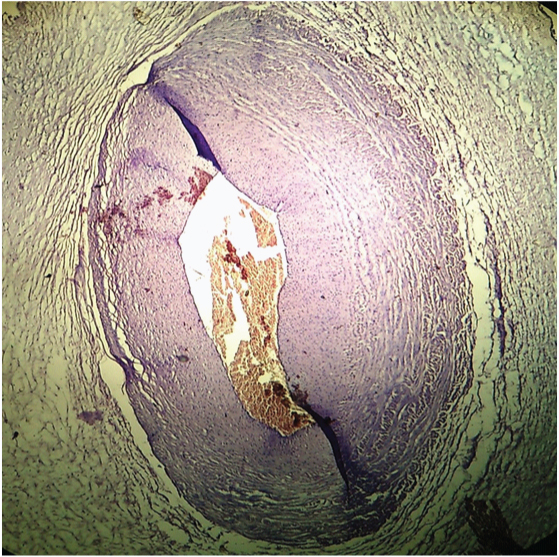
Microscopically, single umbilical artery and single umbilical vein was seen with persistent vitello-intestinal duct. One cystic lesion (closer to placenta) showed focally dilated umbilical artery suggestive of aneurysm [Table/Fig-4] and other cystic lesion adjacent to the aneurysm showed degenerative changes in wharton’s jelly (pseudocyst).
Microscopic picture of umbilical artery aneurysm
Discussion
Umbilical cord anomalies are rare. Most common umbilical cord anomaly is single umbilical artery with incidence of 0.63% in singleton pregnancy [1]. Umbilical artery aneurysm is still rarer and is associated with increased risk of aneuploidy, IUGR and fetal demise. Till date, 14 cases of umbilical artery aneurysm have been reported, out of which only four were live born with normal karyotype [Table/Fig-5] [2–12].
Summary of reported cases of umbilical artery aneurysm [2–12]
| No. of cases | Reference | Detected UAA | Karyotype | Outcome | Cord | Site of lesion in relation to cord |
|---|
| 1 | Fortune et al., [2] (1978) | After delivery | NA | IUFD | 3VC | Middle |
| 2 | Siddiqi et al., [3] (1992) | 30wk | Male fetus Karyotype-NA | IUFD | SUA | Middle |
| 3 | Jeffery [4] (2001) | NA | NA | IUFD | NA | At placental insertion |
| 4 | Berg et al., [5] (2001) | 34wk | Trisomy 18 | Stillbirth | 3VC | Close to fetus |
| 5 | Mysorekar et al., [6] (2002) | After delivery | 46,XY | Liveborn at 38wk | 3VC | Middle |
| 6 | Sepulveda et al., 1 [7] (2003) | 32wk | Trisomy 18 | Died on 50th day of life | SUA | At placental insertion |
| 7 | Sepulveda et al., 2 [7] (2003) | 30wk | Trisomy 18 | Died on 18th day of life | SUA | At placental insertion |
| 8 | Sepulveda et al., 3 [7] (2003) | 35wk | Trisomy 18 | Died on 1st day of life | SUA | At placental insertion |
| 9 | Weber et al., [8] (2007) | 32wk | 46,XY | IUFD | SUA | At placental insertion |
| 10 | Shen et al., [9] (2007) | 22wk | 46,XY | IUFD | SUA | Close to fetus |
| 11 | Sentilhes et al., [10] (2007) | 22wk | 46,XY | IUFD | SUA | At placental insertion |
| 12 | Hill et al., [1] (2010) | 27wk | 46,XY | Liveborn at 28wk | SUA | At placental insertion |
| 13 | Olog et al., [11] (2011) | 28wk | Karyotype-NA | Liveborn at 31wk | 3VC | At placental insertion |
| 14 | Doehrman et al., [12] (2014) | 21wk | Normal karyotype* | Liveborn at 32wk | 3VC | NA |
| 15 | This case (2015) | 33wk | 46,XX | Liveborn at 36wk | SUA | At placental insertion |
UAA-umbilical artery aneurysm; NA-not available; IUFD-intrauterine fetal demise; 3VC- three vessel cord; SUA-single umbilical artery; *gender NA
Aneurysm of umbilical artery or vein is the least common vascular anomaly of the cord [5]. The vein is more affected compared to the artery [13]. The umbilical vessels are derived embryologically from allantoic blood vessels by 5th week of gestation [7]. But it is unclear when an aneurysm of umbilical vessel occurs. By the case reports reported till date, the lesions were identified by late second trimester (22-27 wk) and mostly in third trimester (30-34 wk) [Table/Fig-5]. Most of the cases had single umbilical artery (8 out of 14 cases) and the same was noticed in our case too. When a umbilical cord possess only one artery and vein, the artery probably undergoes compensatory increase in diameter and this increases with the gestational age due to increase in fetal cardiac output [7]. Probably, that is the reason for detecting more cases of umbilical artery aneurysm in early third trimester. Even in our case, it was detected prenatally at 33 weeks of gestation. This observation demands for meticulous sonographic evaluation of the cord not only during anomaly scans but also during third trimester growth scans.
Wharton’s jelly plays an important role in protecting the cord and preventing aneurysmal dilatation. So aneurysms are commonly located near placenta cord insertion where umbilical vessels branch into chorionic plate and probably loose the protection of wharton’s jelly. In 71% of cases, the lesion is seen at the insertion of the cord either close to placental insertion or close to fetus [Table/Fig-5]. Same was seen in our case, aneurysm was close to the placental insertion and in fact a degenerative wharton’s jelly (pseudocyst) was seen adjacent to the aneurysm. True cysts are lined by epithelium and orginate from embryonic remnants, such as allantois or omphalomesentric duct, whereas pseudocysts are local degeneration or focal oedema of wharton’s jelly and lack an epithelial lining [14].
Intrauterine fetal demise is very common with umbilical artery aneurysm. It could be due to thrombus formation, compression of the dilatated artery on the umbilical vein or due to associated fetal anomaly like trisomy 18 [9]. Out of 14 cases reported, only 4 were live born with normal karyotype. Though in our case the baby’s karyotype is normal (46,XX), the previous reports show a strong association of umbilical artery aneurysm and trisomy 18 [7]. The reason for such an association can be explained by abnormal placental vasculature in trisomy 18. As an observatory point [Table/Fig-5], Umbilical artery aneurysm is associated with trisomy 18 or with male fetus (46,XY). The exact reason of this association with male fetus is not known. In contrast to this finding, in our case it was a female baby (46,XX). With stillbirth of euploid fetus occurring between 26 to 34 weeks [1], it is often difficult to say when the fetus is at greatest risk for intrauterine fetal death and the exact cause for it. Unfortunately, though aneurysm is identified prenatally by ultrasonography, we may fail to prevent fetal demise even with frequent intensive fetal monitoring as the death can occur due to acute nature of thrombosis or due to rupture of the aneurysm.
Umbilical cord aneurysm can be missed easily on routine prenatal sonographic examinations if not thoroughly looked for it. Serial ultrasound assessment of the fetus with single umbilical artery regardless of presence or absence of coexisting anomalies is warranted so as to detect lethal cord anomalies. Sepulveda [15] proposed a systemic approach to the assessment of the umbilical cord during second trimester scan by assessing four characteristics of the umbilical cord like: 1) evaluation of the number of vessels; 2) measurement of umbilical cord area; 3) assessment of placental umbilical cord insertion site; 4) determination of the coiling pattern.
Conclusion
Umbilical cord anomalies are associated with significant fetal morbidity & mortality. Hence, careful prenatal assessment of umbilical cord in sonography is a must. If an anechoic cyst is detected in the umbilical cord, doppler will play a critical role to differentiate vascular from non-vascular lesions. If multiple congenital fetal anomalies are detected, prenatal karyotype has to be done. In isolated umbilical cord aneurysm with otherwise structurally normal fetus, close fetal surveillance and delivery at the earliest is recommended.
UAA-umbilical artery aneurysm; NA-not available; IUFD-intrauterine fetal demise; 3VC- three vessel cord; SUA-single umbilical artery; *gender NA
[1]. Hill AJ, Tomas H, Strong J, Elliot JP, Perlow JH, Umbilical artery aneurysmACOG 2010 116(2):559-62. [Google Scholar]
[2]. Fortune DW, Ostor AG, Umbilical artery aneurysmAm J Obstet Gynecol 1978 131:339-40. [Google Scholar]
[3]. Siddiqi TA, Bendon R, Schultz D, Miodovnik M, Umbilical artery aneurysm: prenatal diagnosis and managementObstet Gynecol 1992 80:530-33. [Google Scholar]
[4]. Jeffrey I, Intrapartum asphyxia and birth trauma. In: J Keeling, editorFetal and neonatal pathology 2001 London (UK)Springer Verlag:237-59. [Google Scholar]
[5]. Berg C, Geipel A, Germer U, Gleckner-Hofmann K, Gembruch U, Prenatal diagnosis of umbilical cord aneurysm in a fetus with trisomy 18Ultrasound Obstet Gynecol 2001 17:79-81. [Google Scholar]
[6]. Mysorekar V, Dandekar C, Sundari N, Umbilical artery aneurysm; report of a rare caseSingapore J Obstet Gynecol 2002 33:51-53. [Google Scholar]
[7]. Sepulveda W, Corral E, Kottmann C, Illanes S, Umbilical artery aneurysm: prenatal identification in three fetuses with trisomy 18Ultrasound Obstet Gynecol 2003 21:292-96. [Google Scholar]
[8]. Weber MA, Sau A, Maxwell DJ, Mounter NA, Third trimester intrauterine fetal death caused by arterial aneurysm of the umbilical cordPediatr Dev Pathol 2007 10:305-08. [Google Scholar]
[9]. Shen O, Reinus C, Baranov A, Rabinowitz R, Prenatal diagnosis of umbilical artery aneurysm: a potential lethal anomalyJ Ultrasound Med 2007 26:251-53. [Google Scholar]
[10]. Sentilhes L, Vivet-Lefeure A, Patrier S, Lefebvre-Lacocuille S, Umbilical artery aneurysm in a severe growth-restricted fetus with normal karyotypePrenat Diagn 2007 27:1059-61. [Google Scholar]
[11]. Olog A, Thomas JT, Peterson S, Cattanach S, Large umbilical artery aneurysm with a live healthy baby delivered at 31 weeksFetal Diagn Ther 2011 29:331-33. [Google Scholar]
[12]. Doehrman P, Derksen BJ, Perlow JH, Clewell WH, Umbilical artery aneurysm: a case report, literature review, and management recommendationsObstet Gynecol Surv 2014 69:159-63. [Google Scholar]
[13]. Nathalie MA, Vandevijer MD, Ralf HM, Connie CT, Aneurysm of umbilical vein: case report and review of literatureEuropean J of Obstet Gynecol Reproduct Biology 2000 89:85-87. [Google Scholar]
[14]. Sepulveda W, Gutierrez J, Sanchez J, Cecilia BE, Schnapp C, Pseudocyst of the umbilical cord: Prenatal sonographic appearance and clinical significanceObstet and Gynecol 1999 93:377-81. [Google Scholar]
[15]. Sepulveda W, Amy E, Wong E, Gomez L, Alcalde J, Improving sonographic evaluation of the umbilical cord at the second – trimester anatomy scanJ Ultrasound Med 2009 28:831-35. [Google Scholar]