A Case of Cervical Spine Tuberculosis in an Infant
SN Singh1, Trilok C Bhatt2, Savit Kumar3, Vikas Chauhan4, Anjali Pandey5
1 Head of the Department and Associate Professor, Department of Radiology, INHS, Kalyani, Gandhigram Po Visakhapatnam, India.
2 Senior Resident, Department of Radiology, INHS, Kalyani, Gandhigram Po Visakhapatnam, India.
3 Senior Resident, Department of Radiology, SCTIMST, Trivandrum, India.
4 Assistant Professor, Department of Radiology, INHS, Kalyani, Gandhigram Po Visakhapatnam, India.
5 Senior Resident, Department of Paediatrics, INHS, Kalyani, Gandhigram Po Visakhapatnam, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. SN Singh, Department of Radiology, INHS Kalyani, Gandhigram PO Visakhapatnam - 530005, India. E-mail : cdrsingh@gmail.com
Tuberculosis of cervical spine is an extremely rare entity in infants with only few case reports available in the literature. The diagnosis is often delayed due to less dramatic effects of paraplegia or quadriplegia in an infant as compared to older paediatric population. Along with clinical and laboratory investigations, imaging plays a crucial role in defining the extent of involvement, evaluation of complications, providing suitable differential diagnosis and monitoring response to treatment. Tuberculosis typically involves the discovertebral complex while involvement of isolated vertebral body or multiple vertebrae without involving the intervertebral discs is much less common. We present such an unusual case of cervical spine tuberculosis in an infant involving a single vertebral body without adjacent intervertebral disc involvement complicated with tuberculous meningitis (TBM) and communicating hydrocephalus. The early medical intervention in this case resulted in early diagnosis, active treatment and resultant near normal recovery.
Tubercular meningitis, Leptomeningeal enhancement
Case Report
An eight-month-old male infant was brought to paediatric department of our hospital with history of fever since 13 days, projectile vomiting since 07 days and drowsiness since 03 days. The fever was of moderate degree and intermittent type, which was followed by projectile vomiting and later the child became drowsy with poor feeding. The child was born out of non consanguineous marriage and had attained all the milestones at the expected rate. The birth of the child was uneventful and was a full term institutional delivery. The child was inoculated with Bacillus Calmette- Guerin (BCG) in neonatal period which was followed by normal reaction and scar.
On examination the child was drowsy but arousable with a heart rate of 120 bpm, blood pressure of 100/70 mm of Hg, respiratory rate of 24 and temperature of 100 degree F. The child weighed 7.5 kgs. The head circumference measured normal for age. The anterior fontanelle was tense, and bulging. Bilateral pupils were equally reactive. Neck rigidity was present with occasional tonic flexion in the upper limbs. The deep tendon jerks were exaggerated bilaterally with bilateral extensor plantar reflex. The neck movements were painful and restricted. There was no lymphadenopathy, papilloedema, muscle wasting or weakness.
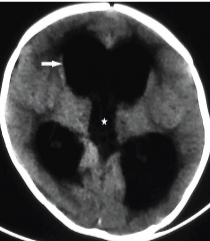
The haemogram showed erythrocyte sedimentation rate of 50 mm in first hour. Mantoux test was positive with an induration of 15 mm in 48 hours. The cerebrospinal fluid (CSF) analysis showed protein of 200mg/dl, glucose of 20mg/dl, cell count of 120 cells per mm3 which were predominantly lymphocytes. The chest radiograph revealed normal lung fields. Ultrasonography of abdomen was unremarkable. A serological test done for HIV was negative. NCCT head showed dilatation of all ventricles [Table/Fig-1]. With a clinical and imaging diagnosis of tubercular meningitis with communicating hydrocephalus an MRI of the brain was performed after placing ventriculo- peritoneal (VP) shunt for CSF drainage.
Axial NCCT section of the brain at the level of third ventricle showing dilatation of lateral (arrow) and third ventricles (star).
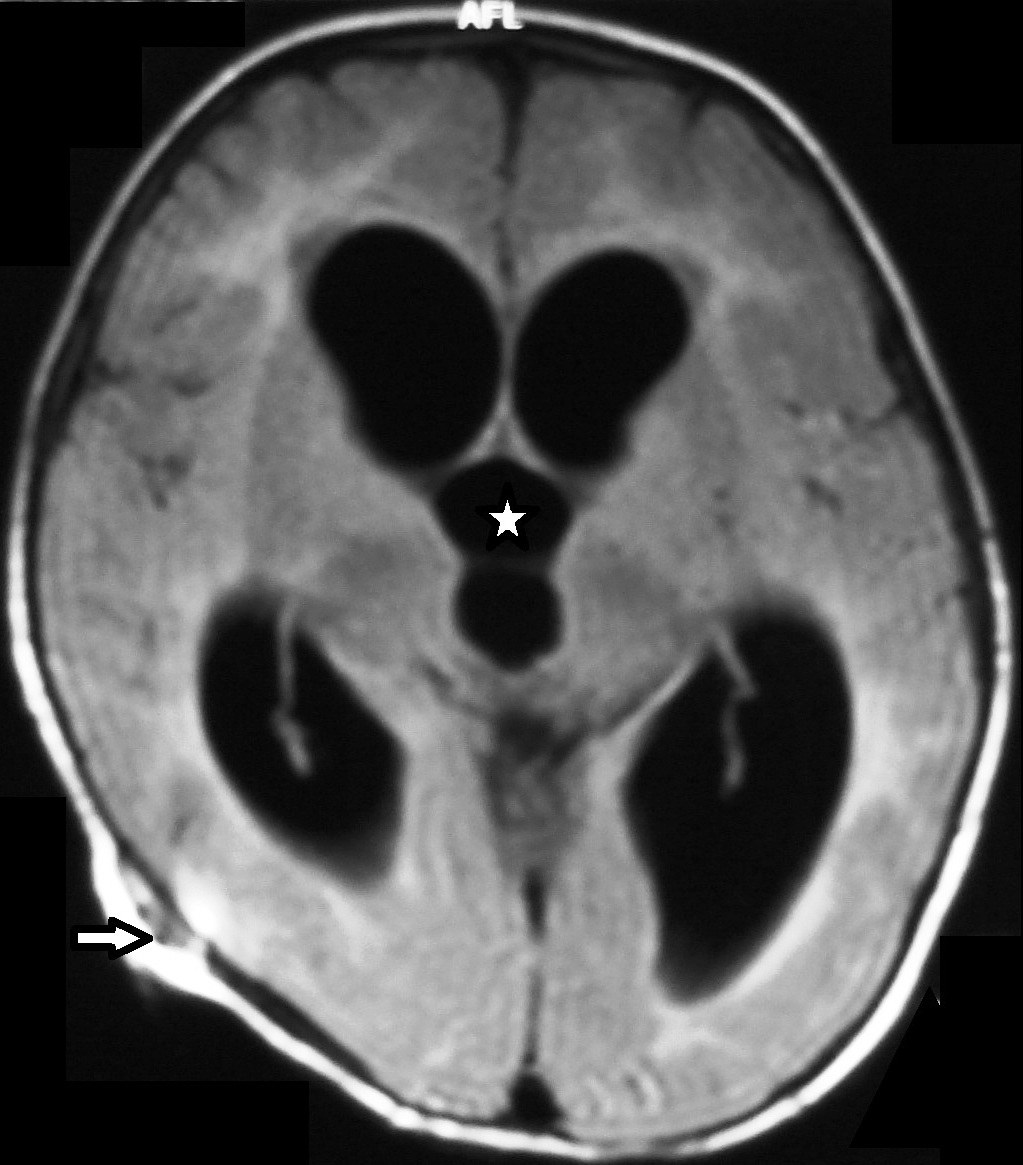
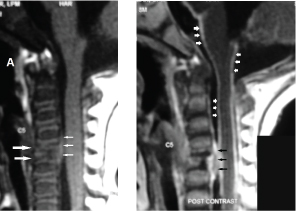
MRI brain [Table/Fig-2] showed gross dilatation of the ventricular system (lateral, third and fourth) with obliteration of the sulci and cisterns. The VSI (Ventricular size index) was 53% with the frontal horn forming an acute angle with the midline septum. There was thickening and intense enhancement of the dura predominantly in the basal region [Table/Fig-3]. The cerebral white and gray matter showed normal morphology and signal intensity. MRI of cervical spine showed collapsed body of CV5 with enhancing soft tissue component which was seen tracking into the extradural space causing significant indentation of the anterior thecal space [Table/Fig-4]. There was associated intense leptomeningeal enhancement around the spinal cord which was extending intracranially.
Axial FLAIR image of the brain showing hydrocephalus (star) with VP shunt track in right parietal region (arrow).
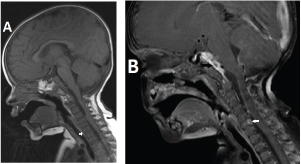
Sagittal precontrast: a) and postcontrast; b) T1W images of the cervical spine showing reduction in height of body of CV5 with enhancing soft tissue component (black arrows) which is seen tracking into the vertebral canal causing significant indentation of the anterior thecal space. Meningeal enhancement of the spinal cord and brain is seen (short white arrows).
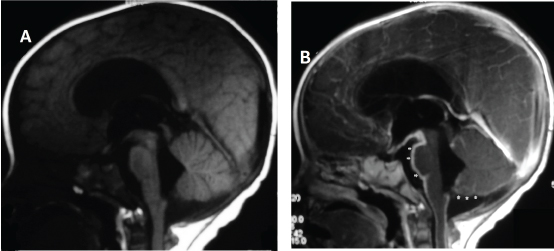
Sagittal precontrast: (a) and postcontrast; (b) T1W images of the brain showing meningeal enhancement along the brain stem as well as cerebellum (arrows).
Based on the clinical, laboratory and imaging findings, a provisional diagnosis of spinal tuberculosis with TBM was made. Image guided tissue sampling from the paravertebral soft tissues was perceived as dangerous by the parents and consent for the same was denied.
Child was empirically started on antituberculous treatment (ATT) and steroids as per Indian Academy of Paediatrics (IAP) recommendations. The infant on follow up showed good recovery. The child gained weight, became alert and afebrile. The MRI repeated after 6 months of treatment showed regression of the hydrocephalus [Table/Fig-5] with significant reduction in enhancing basal exudates, minimal enhancement in pre pontine cistern along with minimally enhancing and collapsed CV5 and resolution of paraspinal collection [Table/Fig-6].
Axial FLAIR image of the brain showing normal morphology and signal intensity of the brain, normal appearance of the ventricular system. VP shunt track is seen right parietal region (down arrows).

Sagittal pre contrast: (a) and post contrast; (b) T1W images of the brain and cervical spine showing resolution of paraspinal soft tissue component and minimal enhancement of the vertebral body (white arrows), enhancing basal exudates is visible in pre pontine cistern (black arrows). No evidence of meningeal enhancement seen.
Discussion
Tuberculosis of cervical spine in infants is a rare entity. Spinal involvement is usually a result of haematogenous spread of Mycobacterium tuberculosis into the vasculature of cancellous bone of the vertebral bodies with the primary site of infection usually being a pulmonary or genitourinary lesion [1]. The unique development of vertebral bodies results in a single artery supplying the consecutive halves of vertebral bodies and the intervening intervertebral disc thus causing the commonly observed disco-vertebral involvement in spinal tuberculosis as a result of haematogenous spread; however this fails to explain the less commonly observed single vertebral involvement or involvement of multiple vertebral bodies without involvement of intervertebral discs. A postulated mechanism is spread of infection via Batson’s paravertebral venous plexus [2] with subsequent intravertebral spread via intraosseous veins.
The minimum time required for osteoarticular tuberculosis to manifest is postulated as one year after the primary infection [3] hence it is extremely unusual to present before one year of age. A series on spinal tuberculosis in paediatric age group reported the minimum age of presentation as 1.9 years [4] with no child less than one year of age in the series. Various other large studies of paediatric spinal tuberculosis have also not reported infantile spinal tuberculosis [5–7].
Diagnosis of spinal TB in infants is often delayed as the effects of early cord compression are subtle as compared to older children and early deficit may go unnoticed by the caregivers [8] hence high level of suspicion, prompt diagnosis and early treatment are crucial to prevent permanent neurological deficit and deformity.
TBM with spinal involvement, which commonly presents as paraplegia, occurs in less than 10% of cases [9]. Vertebral tuberculosis (Pott’s disease) is associated in about a quarter of patients with TBM with spinal involvement and associated fusiform para-vertebral abscesses or gibbus. The presence of extradural cord tuberculomas are the primary cause of non-osseous paraplegia in almost 60% of cases [10].
The role of imaging in evaluation of central nervous system tuberculosis is well established. Magnetic resonance imaging (MRI) with Gadolinium enhancement is the preferred imaging investigation and is the most sensitive test for detecting the extent of leptomeningeal disease [11,12]. The haematogenous spread is usually the primary cause in Tuberculous meningitis, however TBM can also spread secondarily due to rupture of a Rich focus or a direct extension from cerebrospinal fluid (CSF) infection [13–15]. The abnormal meningeal enhancement is the typical finding on a contrast enhanced MRI, which is seen most pronounced in the basal cisterns [15].
The complications of TBM are also readily visualized on MRI. Communicating hydrocephalus caused by blockage of the basal cisterns by inflammatory exudates is the most common complication of tubercular meningitis [16]. Occasionally, noncommunicating hydrocephalus may occur due to the mass effect of a tuberculoma causing the obstruction of CSF flow. Ischemic infarcts and cranial nerve involvement are other common complications [13–16] but their incidence in infants is not known.
Spinal tuberculosis is characteristically associated with little or no reactive sclerosis or local periosteal reaction, as opposed to pyogenic infections of the spine. Infection usually begins in the anterior part of the vertebral body adjacent to the end plate. The inflammation and subsequent increased vascularity leads to demineralization of the end plate and resultant loss of definition of its dense margins. The infection spreads into the paraspinal soft tissues resulting in a Pott abscess. In a chronic setting it leads to calcification within the abscess – a pathognomonic sign in diagnosis of Pott’s spine [17].
Conclusion
Tuberculosis of cervical spine in infants is a rare entity. Spinal involvement is usually a result of haematogenous spread of Mycobacterium tuberculosis into the vasculature of cancellous bone of the vertebral bodies with the primary site of infection usually being a pulmonary or genitourinary lesion. In the tuberculous process, the spinal meninges may be involved owing to the spread of infection from intracranial meningitis, primary spinal meningitis in isolation or transdural extension of infection from caries of the spine. In our case the spread of infection appeared to be from the caries spine through a transdural extension leading to meningitis and its complication (hydrocephalus). This case also emphasizes the importance of recognizing these cases early in the course of disease, administering active treatment and prevent complications.
[1]. Schirmer P, Renault CA, Holodniy M, Is spinal tuberculosis contagious?Int J Infect Dis 2010 14(8):e659-66. [Google Scholar]
[2]. Garg RK, Somvanshi DS, Spinal tuberculosis: A reviewThe Journal of Spinal Cord Medicine 2011 34(5):440-54. [Google Scholar]
[3]. Starke JR, Tuberculosis. In: Feigin RD, Cherry JD, Demmler GJ, et al, edsText book of Paediatric Infectious Diseases 2009 Vol. 16th edElsevierSaunders:1442-1223. [Google Scholar]
[4]. Govender S, Ramnarain A, Danaviah S, Cervical spine tuberculosis in childrenClin Orthop Relat Res 2007 460:78-85. [Google Scholar]
[5]. Bailey HL, Gabriel M, Hodgson AR, Shin JS, Tuberculosis of spine in children. Operative findings and results in one-hundred consecutive patients treated by removal of the lesion and anterior graftingJ Bone Joint Surg Am 1972 54:1633-57. [Google Scholar]
[6]. Andronikou S, Jadwat S, Douis H, Patterns of disease on MRI in 53 children with tuberculosis spondylitis and the role of gadoliniumPaediatr Radiol 2002 32:798-805. [Google Scholar]
[7]. Mushkin AY, Kovalenoko KN, Neurological complications of spinal tuberculosis in childrenInt Orthop 1999 23:210-212. [Google Scholar]
[8]. Kapoor Sudhir K, Tiwari A, Chaudhry A, An unusual case of craniovertebral junction tuberculosis in an infantSpine 2007 32(23):E678-81. [Google Scholar]
[9]. Thwaites GE, Nguyen DB, Nguyen HD, Dexamethasone for the treatment of tuberculous meningitis in adolescents and adultsN Engl J Med 2004 351:1741-51. [Google Scholar]
[10]. Dastur DK, Neurosurgically relevant aspects of pathology and pathogenesis of intracranial and intraspinal tuberculosisNeurosurg Rev 1983 6:103-10. [Google Scholar]
[11]. Thirunavukarasu SC, Ramachandrappa A, A rare case of intramedullary tuberculoma: Complete resolution after medical treatment and role of magnetic resonance imaging in diagnosis and follow-upAsian J Neurosurg 2012 7(4):223-26. [Google Scholar]
[12]. Sankhe S, Baheti A, Ihare A, Mathur S, Dabhade P, Sarode A, Perfusion magnetic resonance imaging characteristics of intracerebral tuberculomas and its role in differentiating tuberculomas from metastasesActa Radiol 2013 54(3):307-12. [Google Scholar]
[13]. Whiteman ML, Neuroimaging of central nervous system tuberculosis in HIV-infected patientsNeuroimaging Clin N Am 1997 7(2):199-214. [Google Scholar]
[14]. Morgado C, Ruivo N, Imaging meningo-encephalic tuberculosisEur J Radiol 2005 55(2):188-92. [Google Scholar]
[15]. de Castro CC, de Barros NG, Campos ZM, Cerri GG, CT scans of cranial tuberculosisRadiol Clin North Am 1995 33(4):753-69. [Google Scholar]
[16]. Jinkins JR, Gupta R, Chang KH, Rodriguez-Carbajal J, MR imaging of central nervous system tuberculosisRadiol Clin North Am 1995 33(4):771-86. [Google Scholar]
[17]. Joshua B, Christopher JW, Gillian B, Gabriel C, Andrew LH, Rakesh RM, Tuberculosis: A Radiologic ReviewRadiographics 2007 27(5):1255-73. [Google Scholar]