A Comparative Study of Pre and Post-prandial BP Recordings in Obese and Non Obese Young Adults
Anitha Sequeira1, David Rosario2
1 Assistant Professor, Department of Medicine, Srinivas Institute of Medical Science and Research Center, Mukka, Mangalore, India.
2 Assistant Professor, Department of Ear, Nose and Throat, Srinivas Institute of Medical Science and Research Center, Mukka, Mangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anitha Sequeira, Assistant Professor, Department of Medicine, Srinivas Institute of Medical Science and Research Center, Mukka, Mangalore-575021, India.
E-mail: anitha.sequeira@gmail.com
Introduction
Obesity is associated with varied combinations of abnormalities in the autonomic nervous system. Studies have shown that obese people who have a higher sympathetic tone have higher catecholamine levels. This can predispose to arythmogenesis and sudden death.
Aim
To study pre and post-prandial BP recordings in obese and non obese young adults in the age group of 18 to 45 years.
Materials and Methods
The study was conducted on 50 obese and 50 non obese patients admitted to our hospital over a period of three months. The patients are randomly selected and the BMI is calculated. Both systolic and diastolic blood pressure is measured in supine position of the right arm using digital electronic blood pressure monitor. BP recordings are taken 30 minutes before and 30 minutes after meals. Then fall in BP is recorded.
Results
From this study we found that the mean systolic (pre-prandial 124.36, post-prandial 116.6) and diastolic blood pressure (pre-prandial 78.8 and post-prandial 75.4) is higher in obese than non obese patients. The study was statistically significant which was found by paired t-test (p<0.05).
Conclusion
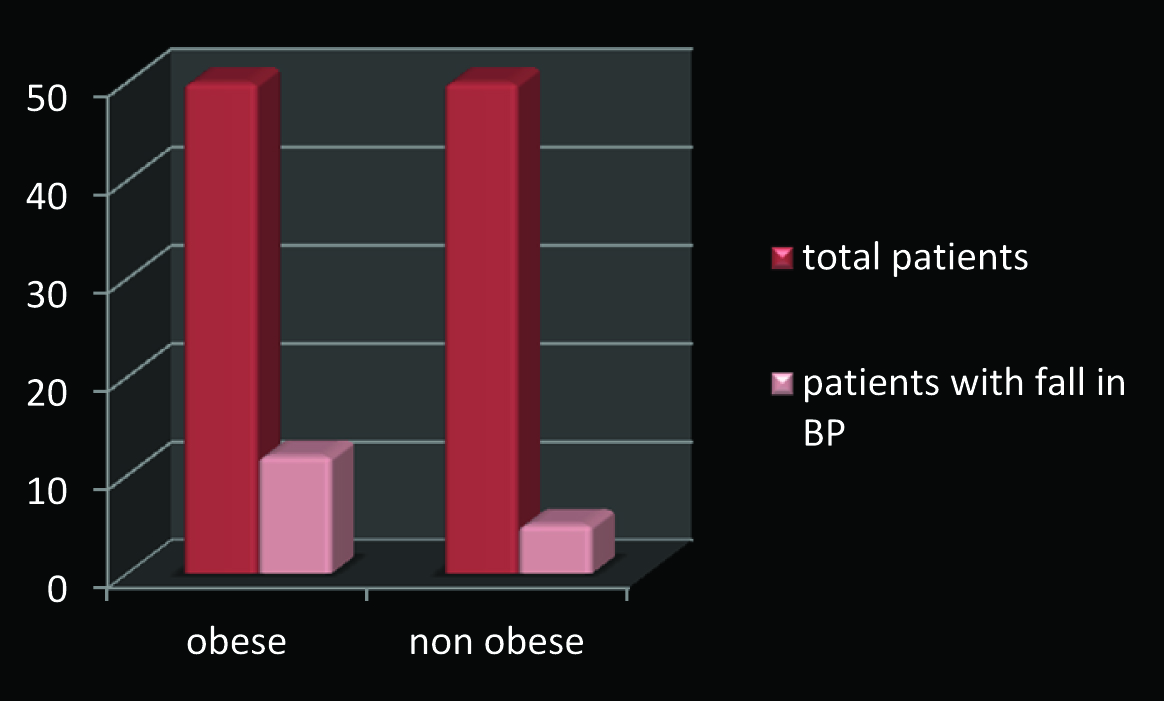
The fall in BP was significantly higher in obese (12 patients out of 50) than non obese (5 patients out of 50) patients. Probably obese patients had reduced cardiac sympathetic tone which caused post-prandial hypotension more than non obese patients.
DBP-diastolic BP, Post-prandial hypotension, SBP–systolic BP
Introduction
Obesity is a major emerging health problem worldwide [1]. Influence of western culture is shifting the nutritional status of India gradually from undernourishment to obesity [1]. Many studies have shown the relationship between obesity and sudden deaths [1]. Obesity is associated with varied combinations of abnormalities in the autonomic nervous system [1]. Studies have shown that obese people who have a higher sympathetic tone have higher catecholamine levels; however there is also supportive evidence of reduced cardiac sympathetic tone in some studies [1].
After consumption of food, peptides are released in gastro intestinal tract, which leads to local vasodilatation. Hence, there is post-prandial redistribution of blood leading to shifting of large volume of blood into the gastrointestinal tract which in turn causes post-prandial hypotension [2]. In normal individuals, this is well compensated and does not lead to post-prandial hypotension [2]. Post-prandial hypotension is fall in the SBP of > 20mmHg or reduction in the post-prandial SBP < 90mmHg when pre-prandial BP is > 100mmHg within two hours of meal [3]. In healthy and elderly individuals meal ingestion is associated with increase in the HR which serves to prevent significant fall in BP [3]. However, in patients with post-prandial hypotension this response is inadequate to maintain the BP. We hypothesized that food intake may result in a transient decrease in parasympathetic activity causing post-prandial hypotension.
Materials and Methods
This is a comparative cross-sectional study which was conducted on 50 obese and 50 non obese patients in the age group of 18 to 45 years admitted to Srinivas Institute of Medical Sciences and research center over a period of 3 months. The study sample was chosen by random selection method and the BMI is calculated.
The BMI was calculated as
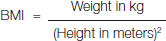
Subjects were classified into two groups based on BMI as follows:
Normal weight: BMI – 18.5 – 24.99 kg/m2 [Table/Fig-1].
Obese : BMI > 30 kg/m2
Classification of obesity based on body mass index
| Category | BMI (kg/m2) |
|---|
| Underweight | <18.5 |
| Normal weight | 18.5-24.9 |
| Over weight | 25-29.9 |
| Obesity (class 1) | 30-34.9 |
| Obesity (class2) | 35-39.9 |
| Extreme obesity (class 3) | >40 |
Both Systolic and Diastolic blood pressure was measured in supine position of the right arm using digital electronic blood pressure monitor. BP recordings are taken 30 min before and 30 min after meals. Then fall in BP is recorded.
Inclusion Criteria
All non obese adults between the age group 18 to 45 years.
All obese adults in the same age group.
Exclusion Criteria
Diabetes.
Alcohol abuse.
Antihypertensive drugs.
Autonomic neuropathy.
Results
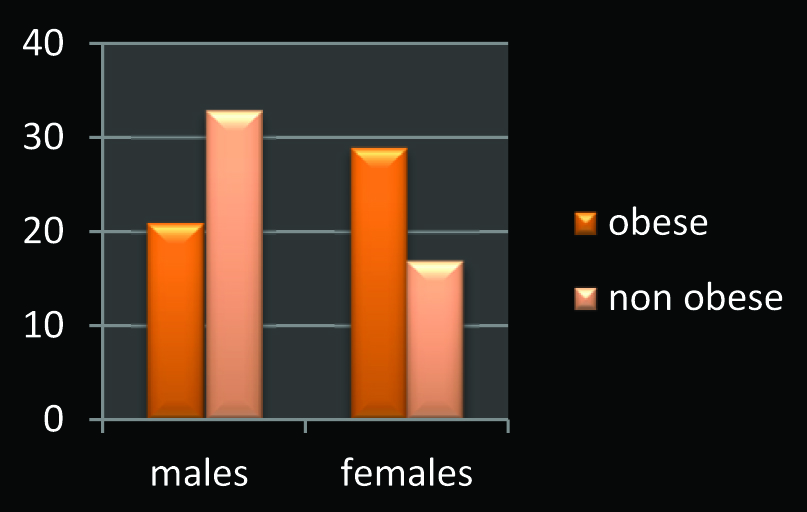
Statistical analysis was done using paired t-test. As depicted in [Table/Fig-2] out of 50 obese patients 21 were males and 29 were females. Out of 50 non obese patients 33 were males and 17 were females.
Sex distribution of obese and nonobese patients
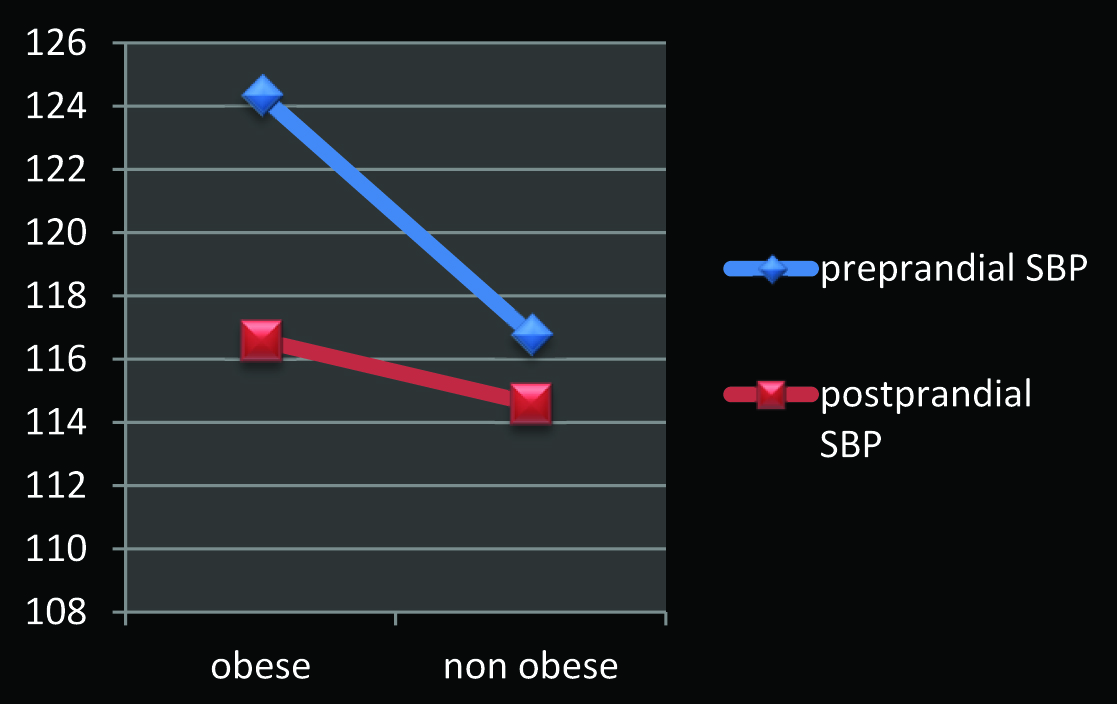
As depicted in [Table/Fig-3,4] mean pre-prandial systolic blood pressure in non- obese and obese were 117.2 and 124.36 respectively whereas the post-prandial systolic blood pressure among non-obese and obese was 114.6 and 116.6 respectively which was found to be statistically significant.
Comparison of pre-prandial and post-prandial SBP between non obese and obese patients
| Group | Mean | SD | T value | p-value |
|---|
| SBP pre-prandial | Non obese | 117.2 | 14.14 | 2.56 | <0.05 |
| Obese | 124.36 | 13.77 |
| SBP post-prandial | Non obese | 114.6 | 14.02 | 0.668 | >0.05 |
| Obese | 116.6 | 15.85 |
| Paired t value & P | T=0.309; p=<0.05 |
Comparison of pre-prandial and post-prandial SBP between non obese and obese patient Graph.
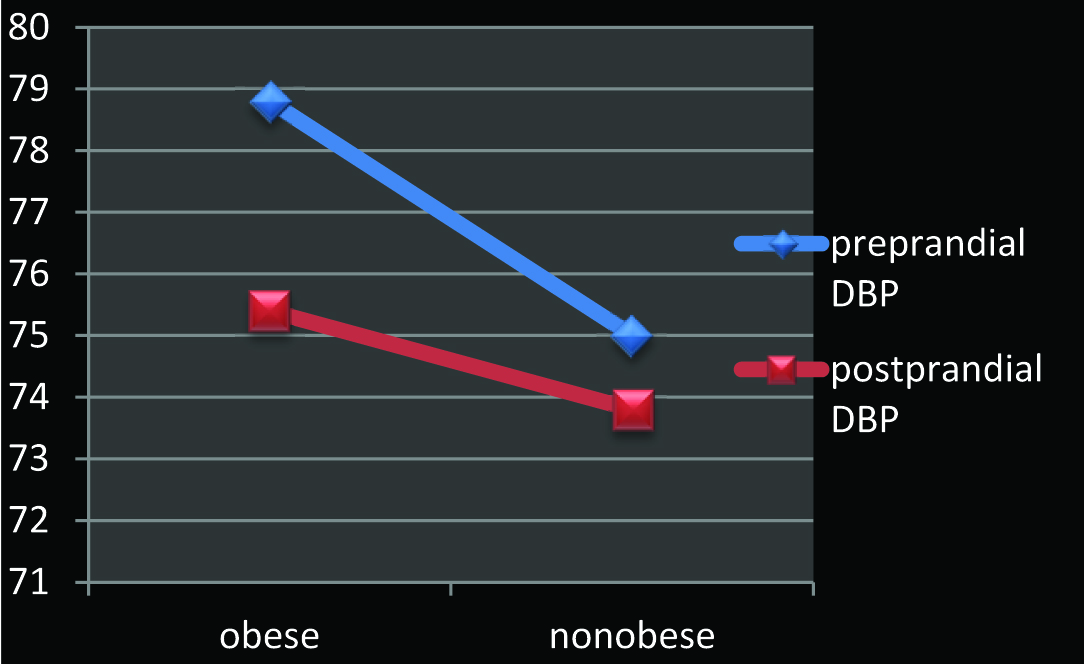
As depicted in [Table/Fig-5,6] mean pre-prandial diastolic blood pressure in non- obese and obese were 75 and 78.8 respectively whereas the post-prandial diastolic blood pressure among non-obese and obese was 73.8 and 75.4 respectively which was found to be statistically significant.
Comparison of pre-prandial and post-prandial DBP between non obese and obese patients.
| Group | Mean | SD | T value | p-value |
|---|
| DBP pre-prandial | Non obese | 75 | 9.52 | 1.6 | <0.05 |
| Obese | 78.8 | 10.81 |
| DBP post-prandial | Non obese | 73.8 | 10.66 | 0.559 | >0.05 |
| Obese | 75.4 | 9.52 |
| Paired t value & P | T=0.309; p=<0.05 | | | |
Comparison of pre-prandial and post-prandial DBP between non obese and obese patients Graph.
As depicted in [Table/Fig-7,8] out of 50 obese patients 12 had fall in blood pressure whereas among 50 non-obese patients 5 had fall in blood pressure.
Patients with fall in BP.
| Total patients | No. of patients with fall in BP |
|---|
| Obese | 50 | 12 |
| Non obese | 50 | 5 |
Patients with fall in BP.
Discussion
From this study we found that the mean systolic and diastolic blood pressure is higher in obese than non obese patients. The study was statistically significant which was found by paired t-test. Thereby the fall in BP was significantly higher in obese than non obese patients. Studies done by Usha et al., and Ambarish et al., have also shown that post-prandial hypotension is significantly higher among obese individuals when compared to non-obese individuals [1,2]. We have hypothesized that there may be a decrease in parasympathetic activity after meals to compensate for the change in blood distribution thereby causing post-prandial hypotension. The studies done by Frenco et al., and Nagai et al., have shown that significant degree of autonomic dysfunction occurs in obese individuals [4,5]. These studies support the hypothesis of our study. In patients who are obese cardiac sympathetic tone is reduced, this has caused post-prandial hypotension more in comparison to non obese patients [6]. Imbalance in cardiac autonomic activity may predispose obese individuals to arrhythmogenesis and subsequently sudden deaths [7].
Post-prandial hypotension is associated with syncope, falls, weakness, angina, dizziness, visual disturbance and Cerebrovascular Accident (CVA) [8]. A strong association between falls and syncope in elderly subjects with post-prandial hypotension has been established [9]. It has been suggested that orthostatic hypotension commonly caused by autonomic function, may contribute to effect of posture on post-prandial fall in BP. It has also been shown that orthostatic hypotension is additive to post-prandial hypotension rather than synergistic [10]. In elderly patients receiving multiple therapies for cardiovascular diseases, orthostatic and post-prandial hypotension should be taken care of.
Limitation
As not much studies are available on post-prandial hypotension among obese and non obese individuals, further study needs to be done in order to understand the pathophysiology and underlying mechanism behind the occurrence of post-prandial hypotension among obese individuals.
Conclusion
From the above study we conclude that post-prandial hypotension was significantly higher in obese than non obese patients. Post-prandial hypotension has received less attention, although it occurs more frequently than orthostatic hypotension and represents substantial cause for morbidity and mortality. However, there are very few studies which have shown correlation of post-prandial hypotension and obesity. Hence there is need for further studies on post-prandial hypotension in various groups.
[1]. Usha RYS, Ramakrishna MR, Manjunath P, Trupti RR, Rangaswamy R, Comparative study of pre-prandial and post-prandial autonomic nervous system response between obese and non obese young women aged 18-25 yearsInt J Pharm Bio Sci 2013 4(3):(B)239-58. [Google Scholar]
[2]. Ambarish V, Barde P, Vyasa A, Deepak K, Comparison between pre-prandial and post-prandial heart rate variability (hrv)Indian J Physiol Pharmacol 2005 49(4):436-42. [Google Scholar]
[3]. Fisher AA, Davis MW, Srikusalanukul W, Budge MM, Poatprandial hypotension predicts all cause mortality in older, low level care residentsJ Am Geriatr Soc 2005 53(8):1313-20. [Google Scholar]
[4]. Frenco R, Bernard S, Andrea C, Tiziana G, Barbara DV, Ivana R, Assessment of cardiac autonomic modulation during adolescent obesityObes Rese 2003 11(4):541-48. [Google Scholar]
[5]. Nagai N, Matsumoto T, Kita H, Moritani T, Autonomic nervous system activity and the state and development of obesity in Japanese school childrenObese Res 2003 11(1):25-32. [Google Scholar]
[6]. Vloet LCM, Pel-Little RE, Jansen PAF, Jansen RWMM, High prevalence of post-prandial and orthostatic hypotension among geriatric patients admitted to Dutch hospitalsJournals of Gerontology A 2005 60(10):1271-77. [Google Scholar]
[7]. Mitro P, Feterik K, Lenártová M, Humoral mechanisms in the pathogenesis of post-prandial hypotension in patients with essential hypertensionWiener Klinische Wochenschrift 2001 113(11-12):424-32. [Google Scholar]
[8]. Narender P, Orshoven V, Jansen PAF, Irene Q, Schoon Y, Oye PL, Post-prandial Hypotension in Clinical Geriatric Patients and healthy elderly: Prevalance related to patient selection and Diagnostic criteriaJournal of Aging Research 2010 [Google Scholar]
[9]. Puisieux F, Bulckaen H, Fauchais AL, Drumez S, Salomez-Granier F, Dewailly P, Ambulatory blood pressure monitoring and post-prandial hypotension in elderly persons with falls or syncopesJournals of Gerontology A 2001 55(9):535-40. [Google Scholar]
[10]. Tanakaya M, Takahashi N, Takeuchi K, Katayama Y, Yumoto A, Kohno K, Postprandial hypotension due to a lack of sympathetic compensation in patients with diabetes mellitusActa Med.Okayama 2007 61(4):191-17. [Google Scholar]