According to World Health Organization (WHO) statistics for 2013, India is the country with the highest burden of TB. In India, an estimated incidence figure of 2.1 million cases of TB out of a global incidence of 9 million and TB prevalence is given as 2.6 million [1]. WHO declared Genitourinary tuberculosis (GUTB) as ‘public health emergency’ in 1993 and still continues to be major public health problem in developing countries like India [2,3].
Urinary TB is mostly asymptomatic. There is a slow renal impairment in these patients due to continuous infection causing destruction of renal mass. Healing process causes fibrosis which leads to renal functional loss and resultant obstruction [4]. Reconstruction of urinary tract which is frequently required for patients with urinary TB poses significant challenges. This paper analyses these challenges. Reconstruction of urinary tract in patients with multifocal calyceal and ureteric involvement has poor outcomes.
To analyse challenges in reconstruction of urinary tract in patients with urinary tuberculosis and renal failure.
Materials and Methods
Thirty-one patients with renal tuberculosis were seen from August 2011 to August 2013 at department of Urology, Seth G.S. Medical College and Kings Edward Memorial Hospital Mumbai, India.
We have taken detailed history and performed thorough clinical examination, urine examination and tubercle bacillus cultures, imaging studies and cystoscopy and histological examinations to arrive at the diagnosis. Patients completed the anti Tuberculous-chemotherapy prior to surgery.
Results
Urinary TB counted for 1.1% of all patients with the history of lower urinary tract symptoms and get admitted to the department. There was a male predominance 18 (58.06%) and mean age was 36.2 years (13 -70 years). Eleven patients (35.4%) had serum creatinine levels above 2 mg/dl (1.5 mg/dl being upper normal range of the laboratory). The duration of symptoms was 3 months to 2½ years (average 7.8 months). Eight patients (25.8%) gave past history of pulmonary tuberculosis. [Table/Fig-1] shows clinical features of the patients.
Main clinical feature in genitourinary tuberculosis.
| Clinical feature | No. of patients | Percentage (%) |
|---|
| Flank pain | 14 | 45.1 |
| Dysuria and frequency | 10 | 32.2 |
| Febrile illness | 9 | 29 |
| Renal failure | 11 | 35.4 |
| Hematuria | 6 | 19.4 |
| Scrotal pain | 2 | 9.5 |
| Urinary fistula | 1 | 4.7 |
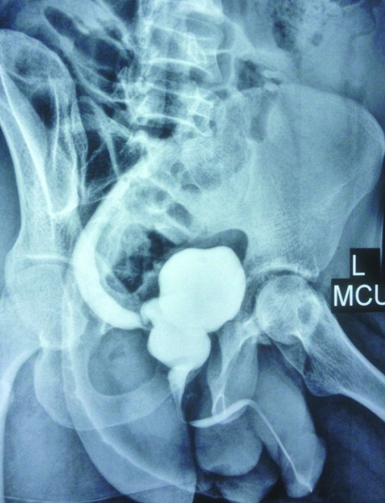
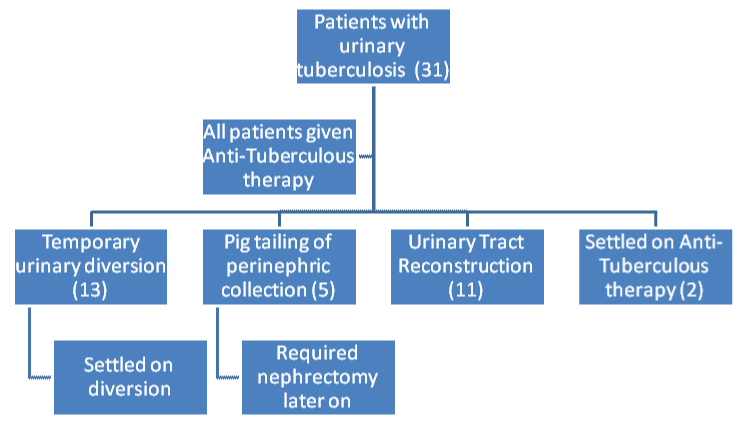
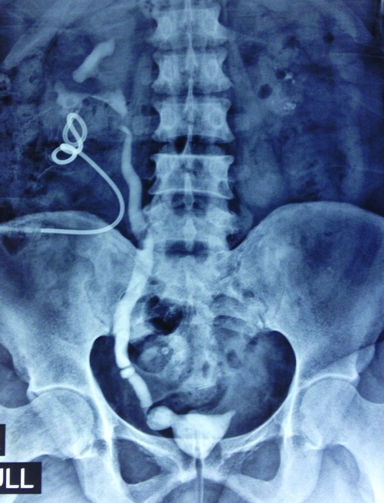
Diagnosis was made on basis of Acid-Fast Bacilli stain, tuberculosis culture, and Tuberculosis-Polymerase Chain Reaction. Radiology revealed involvement of kidney, ureter and bladder varied from non-functioning of kidney, hydronephrosis, calcification [Table/Fig-2], perinephric collection, renal abscess, pelvi ureteric strictures, multiple ureteric strictures, uretero-vesical junction stricture and thimble bladder [Table/Fig-3]. [Table/Fig-4] shows radiological features of the patients. [Table/Fig-5] shows management flow chart of 31 patients.
Plain X-ray film of abdomen showing bilateral nephrocalcinosis.

Micturating Cystourethrogram (Left oblique film) of the patient showing hour-glass contracture of the bladder with concomitant reflux.
Imaging findings in Urinary TB.
| Imaging findings | No. of patients | Percentage (%) |
|---|
| Distortion, scarring | 4 | 12.9 |
| Hydronephrosis or Hydroureteronephrosis | 15 | 48.3 |
| Calcification | 5 | 16 |
| Fistula on contrast study | 2 | 6.4 |
| Ureteric strictures | 9 | 29 |
| Vesico-Ureteral Reflux | 4 | 12.9 |
| Bladder involvement (Reduced capacity, irregularities) | 6 | 19.3 |
| Simultaneous involvement of kidney, ureter, and bladder | 8 | 25.8 |
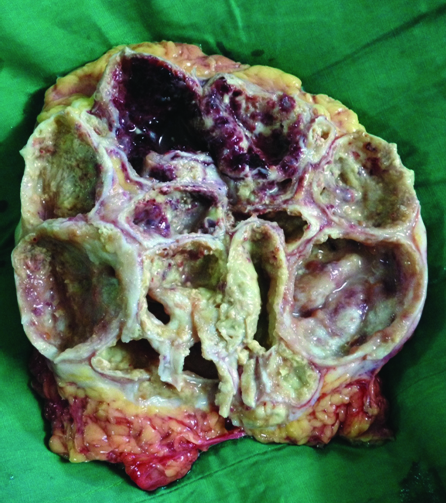
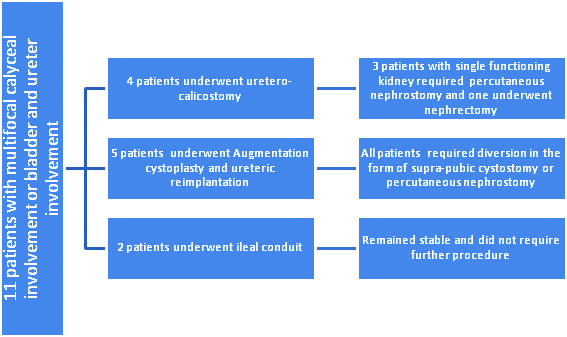
Total 11 patients had far advanced disease in the form of multiple calyceal involvement or simultaneous Kidney, Ureter and Urinary bladder involvement [Table/Fig-6] with nadir creatinine between 2-3 mg/dl after diversion. Four patients underwent ureterocalicostomy procedure and three out of them had single functioning kidney. The surgery failed in all 4 patients. At present, three patients following up with nephrostomy as diversion and serum creatinine around 2.7 mg/dl. One patient with two kidneys required nephrectomy of the diseased kidney [Table/Fig-7] and has one kidney with medical renal disease and serum creatinine was 2.6 mg/dl in the last follow up.
Management flow chart of 31 patients
Nephrogram of the patient showing distorted calyces, contracted drawn-up pelvis, irregular and multiple areas of ureteric narrowing and small contracted bladder.
Cut section pyonephrotic kidney with distortion of calyces.
Five patients with nadir serum creatinine between 2 – 2.5 mg/dl underwent bladder augmentation with ureteral reimplantation. All patients of bladder augmentation had persistently rising serum creatinine in the range of 4-5mg/dl, repeated UTIs metabolic complications for which suprapubic cystostomy (two patients out of five) and /or percutaneous nephrostomies (three patients out of five) was placed and had nadir creatinine of 3mg/dl. Short ileal conduit was done in two patients with serum creatinine more than 2.5mg /dl with longer ureteric involvement to minimize the metabolic complications. Patient with ileal conduit had nadir postoperative creatinine (average- 2.6mg/dl) and were stable and did not require further procedures. The surgical procedures followed in the patients are summarized in [Table/Fig-8].
Discussion
Wilbolz et al., coined the term GUTB which represents tuberculosis that occurs in the kidney, ureter, testis, and epididymis through blood-borne infection [5]. Urinary TB is the term used in this article as we encountered tuberculous involvement of urinary tract only.
Although the disease process in Urinary tuberculosis is slow but it results in caseation and destruction of renal mass. The healing process can lead to stricture, obstruction, secondary calculi and infection causing further renal functional loss and failure [4]. Though often unilateral to start with, cavitary renal TB can cause renal failure in 12% and hypertension in 4-12% of patients [6]. Gupta et al., had reported an incidence of renal failure in 22.4% of patients [7]. Incidence in our study was 35.4%.
Renal TB can result in end-stage renal disease by various mechanisms. We found renal parenchymal damage in form of calcification, destruction of normal renal architecture as principal cause. Other reasons cited are direct insult to renal parenchyma by causing obliterative endarteritis of the intra-renal segmental vessels or secondary renal amyloidosis [8]. There is also the obstruction of pelvi-ureteric junction or multiple infundibular stenosis, which can result in obstructive uropathy [9].
Only 20% to 30% of patients with GUTB have a history of pulmonary infection [10]. Incidence of pulmonary TB in our study was 25.8%. Approximately 75% of renal tuberculosis involvement is unilateral [11]. In our study, 7 patients out of 11 (approx. 13%) had bilateral renal involvement and 4 had single functioning kidneys.
Of the 31 of our patients, 18 were males and 13 females. A male preponderance has been reported in various other studies also [12]. Simon et al., reported dysuria in 34%, haematuria in 27%, flank pain in 10% and pyuria in 5% patients as the most frequent presenting symptoms [13]. Amaresan et al., reported loin pain and haematuria in 33% of their patients while 42% complained of dysuria [4]. In our study, 32% had dysuria and frequency, 19.4% haematuria, 45% loin pain, 35.4% had renal insufficiency and 29% presented as febrile illness. The disease was far advanced at presentation in 11 (35.48%) cases. While reported incidence of renal failure in urinary tuberculosis is 24% [14].
Krishnamoorthy S et al., described various invasive or operative procedures for renal and ureteral TB [14]. They are: (1) drainage for hydronephrosis (ureteric stenting or percutaneous nephrostomy); (2) drainage of abscesses; (3) definitive local treatment of the affected part of the kidney (partial/polar nephrectomy); (4) nephrectomy of the non-functioning tuberculous kidney; and (5) reconstruction of the upper urinary tract (uretero-calicostomy, ureteric reimplantation, ileal ureteric replacement) and bladder augmentation with ileum and ileal conduit.
The patients with urinary tuberculosis have a theoretically benign condition but end up in renal failure due to renal destruction, multifocal calyceal involvement and low compliant bladder. They are subjected to multiple procedures which often have a poor outcome in view of the infundibular stenosis and isolated calyceal obstruction which require separate drainage procedures. Prior to this no study has mentioned urinary tuberculosis together with renal failure in detail. The reasons for failure of ureterocalicostomy in this series are restricture of the anastomosis and multi focal calyceal involvement.
Bladder augmentation with ileum requires at least 25-40 cm segment and leads to metabolic complications of hypokalaemia, hypocalcaemia, hypomagnesaemia and hyperchloraemic metabolic acidosis and frequent urinary tract infections secondary to stasis and clean intermittent catheterization [15]. Three patients out of five who underwent augmentation in this series who finally stabilized on bilateral percutaneous nephrostomy had long ureteric strictures indicating involvement of ureters after surgery. Remaining two patients with no ureteric diseases and augmentation unwilling to do clean intermittent self-catheterization (CISC), later on were kept on suprapubiccystostomy (SPC). The patients who underwent ileal conduit did relatively better and had better ureters. The other segments of bowel which are used include colon and stomach, each having individual metabolic problems but were not used in this series.
None of the patients in these series who were counselled regarding renal replacement in future were willing for transplant and neither had a family support to undergo a transplant. The number of patients with urinary TB requiring renal transplant in this public hospital is nil.
Though counseled for nephrectomy and renal transplant after failure of multiple surgeries patients preferred to continue with nephrostomy or SPC and are lost to follow up. Also, patients with obstructive uropathy who underwent augmentation cystoplasty required secondary diversion post operatively and are unwilling for further treatment. Patients with ileal conduit did not require any further procedures postoperatively. However, the creatinine clearance of < 15 ml/min can be considered as one of the contra indications for augmentation.
Conclusion
Renal TB is an important cause of kidney disease and can lead to end-stage renal disease if not diagnosed early and treated correctly. The short ileal conduit is an easier option for preventing further renal deterioration but with need of external appliance. Augmentation cystoplasty, reconstruction using large segment of bowel predisposes them to metabolic complications and sepsis and need for CISC where in compliance of the patient matters. Use of short segment of ileal conduit with continued drainage at night in creatinine above 2.5 mg % is reasonable option to augmentation.