Introduction
Managing pilon fractures is still a great challenge for surgeons in terms of reduction and fixation. The soft tissue anatomy and the bony configuration, results in angular and rotational instability and other bony and soft tissue complications.
Aim
To evaluate the results of minimally invasive plate osteosynthesis using locking plates in management of fractures of tibial pilon in terms of radiological fracture union, restoration of ankle function and complications.
Materials and Methods
A total of 18 patients with Ruedi Allgower class I, II & III fresh pilon fractures were taken into this study. All the patients underwent ankle spanning external fixator application on the day of presentation as a first stage. Wound debridement was done in patients with open fractures. Associated distal fibula fractures were fixed in the first stage. The second stage comprised of a definitive plate fixation using the minimally invasive plate osteosynthesis technique. This employed minimal periosteal and soft tissue dissection through a medial approach to the ankle. Postoperatively, all patients were reviewed at week six and 12 when partial weight bearing and full weight bearing mobilization was started respectively. The final review was done at 24 weeks when the final assessment of function was done as per the Mazur’s scoring criteria. Analyses were done using frequency and proportions. Chi-square tests were used to assess the test of association.
Results
Three patients had excellent inference, nine patients had good inference, five patients had fair and one patient had poor inference as per the Mazur’s scoring criteria. Two patients had scar dehiscence as a complication and one patient had a fixed equines deformity of the ankle who was under RuediAllgower class III.
Conclusion
Minimally invasive plate osteosynthesis is an excellent method of treating pilon fractures with very good functional results and minimal complication rate.
Introduction
Fractures of the tibial plafond are called as tibial pilon fractures. They account upto 7–10% of all tibial fractures and 1–5% of lower limb fractures [1]. The fracture is an intra-articular fracture extending into the tibiotalar joint and also proximally into the metaphysis [2]. Axial load on the tibia, with or without an accompanying rotational force is considered the major mode of injury [1].
The soft tissue envelope that covers the distal tibia has a precarious circulation [3]. Hence, the incidence of open fractures are higher and the management of these fractures is a challenge as surgical intervention could worsen the circulation [1,4].
The treatment modality is a matter of controversy. The main objective of operative treatment is to reduce the fracture fragments and promote union with minimal disruption of soft tissue envelope [3]. Open reduction and internal fixation was advocated by Ruedi Allgower in 1969 [3]. But subsequent studies indicated incidence of complications such as non-union, malunion, scar dehiscence etc., [3]. External fixation was considered as an option for management by some surgeon but they noted non-union, malunion, pin track infection etc., with these cases [3].
High-energy pilon fractures showed good functional outcome with initial temporary ankle spanning external fixator application and definitive fixation after 10-14 days after the skin conditions improved [1].
The Minimally Invasive Plate Osteosynthesis (MIPO) technique is being popularised now-a-days. The technique employs a limited exposure of the fracture site, hence, reducing the periosteal elevation and stripping with insertion of the plate across the fracture site thereby improving fracture union and ankle function [2]. Several types of implants have been developed for management of pilon fractures with MIPO technique [2]. We used the distal tibial locking plates (LP) in our study.
Aim
To evaluate the results of minimally invasive plate osteosynthesis using locking plates in management of fractures of tibial pilon in terms of radiological fracture union, restoration of ankle function and complications.
Materials and Methods
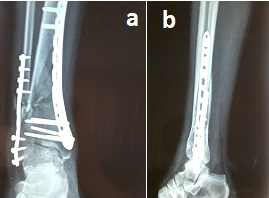
A prospective study was conducted on 18 patients, from October 2012 to September 2014. The ethical clearance was obtained by the ethical committee of our university and consent was obtained from the patients after explaining in detail all the criteria and complications that could occur in the patient’s own language. The inclusion criteria were all skeletally mature patients with fresh intra-articular pilon fractures which satisfied the Ruedi Allgower classification criteria [Table/Fig-1a,b]. Skeletally immature patients and patients with pathological pilon fractures were excluded. Patients with other fractures apart from the pilon fracture which could affect the ankle function were also excluded from the study. A staged surgical protocol was employed for all our patients. The first stage included ankle spanning external fixator application on the day of presentation.
Preoperative anteroposterior and lateral radiographs of the right ankle showing RuediAllgower type II pilon fracture

[Table/Fig-2a&b]. Open fractures underwent wound debridement and external fixator application on the day of presentation. The associated distal fibula fractures underwent open reduction and 1/3rd tubular plate fixation on the day of presentation. Proximal fibula fractures were left alone. A minimum of ten days of waiting period was maintained between the first stage and stage of definitive surgery, wherein antibiotics and anti-oedema measures were instituted.
After ankle spanning external fixator application;

1/3rd tubular plating of distal fibula

For the definitive fixation with locking plates, the patient was positioned supine on the operating table with limb in external rotation. The first step was assessing the plate configuration to the fracture geometry under fluoroscopic guidance by placing the plate over the fractured zone. A medial approach to the ankle was employed. The periosteal elevation and dissection was kept to a minimum. The medial distal tibia locking plate was slid in percutaneously under fluoroscopic guidance [Table/Fig-3]. Once the plate was inserted stab incisions were made in the Zones of the locking screws. The screw insertion was done. The soft tissue dissection was kept to a minimum. Skin closure was done. Postoperative radiographs were taken [Table/Fig-4a,b].
Minimally invasive percutaneous plate insertion

Anteroposterior and lateral radiographs of the right ankle after locking plate fixation
Postoperatively, patients were started on active ankle mobilization on postoperative day two. Non-weight bearing crutch mobilization was begun on postoperative day two. Patients were discharged on postoperative day six. Suture removal was done on postoperative day 10 depending on the soft tissue conditions. Non-healing wounds and ulcers were managed with regular dressings and antibiotics. Associated medical problems like diabetes mellitus and hypertension were attended.
The patients were reviewed on a regular basis on postoperative week six, 12 and 24. Patients were assessed for range of motion of ankle, wound condition and fracture healing on radiographs. They were started on partial weight bearing mobilization and ankle pump exercises on week six depending on the radiological assessment of union. On week 12 full weight bearing mobilization was begun depending at the radiological analysis. Final follow up was done on week 24 and functional assessment was made using the Mazur’s score [3,5]. Complications were documented.
Statistical Statistical
Statistical Statistical analyses were done using frequency and proportions. Chi-square tests were used to assess the test of association.
Results
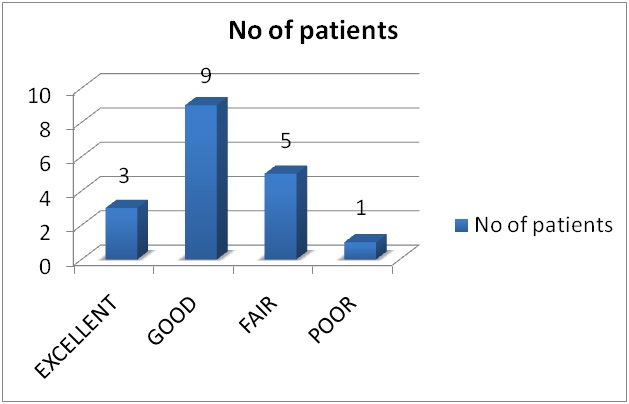
Amongst the 18 patients included in the study 12 were male and 6 were females. A 67% of the patients were under 50 years of age and remaining 33% were over 50 years of age. Amongst the patients under the study 11% of them presented with class I RuediAllgower, 72% class II RuediAllgower, and 17% presented with class III RuediAllgower pilon fractures. Three of the 18 patients had excellent, nine had good, five had fair and one had poor scores [Table/Fig-5].
Bar graphs showing the distribution of patients as per the inference noted after modified Mazur’s scoring of ankle function
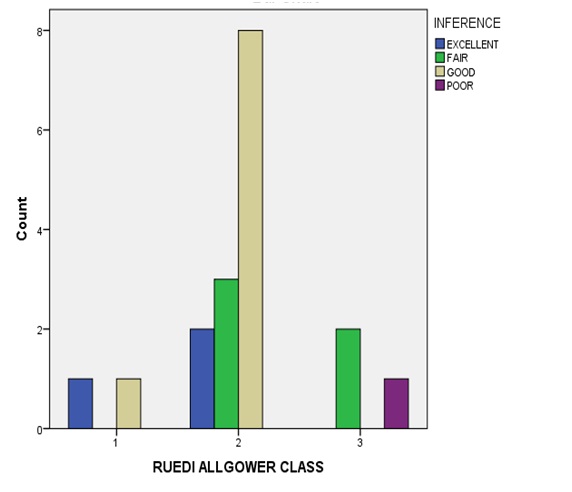
Of the two patients under Ruedi Allgower class I, one patient had excellent score and one had good score [Table/Fig-6]. Of the 13 patients under class II RuediAllgower, two patients had excellent score, eight had good score and three patients had fair score [Table/Fig-6]. Of the three patients who presented as RuediAllgower class III, two patients had fair score, one patient had poor score [Table/Fig-6]. Two patients had scar dehiscence as a complication and one patient had a fixed equines deformity of the ankle with a non-healing ulcer [Table/Fig-7] over the surgical site as a complication who was under RuediAllgower class III.
Bar graphs showing Ruedi Allgower class 1,2,3 with respective patients under each class and modified Mazur scores
a) Of the two patients under Ruedi Allgower class I, One patient had excellent inference and one patient had good inference.
b) Of the 13 patients under class II Ruedi Allgower, Two patients had excellent inference Eight patients had good inference and three patients had fair inference.
c) Of the three patients who presented as RuediAllgower class III, none had excellent or good inference. Two patients had fair inference and one patient had poor inference.
Wound slough formation over surgical site with non-healing ulcer formation

Fifteen of the 18 fractures united at 12 weeks, in three patients union was noted in the final review at six months. No malunion, non-union or failure of implant was noted.
Discussion
Metaphyseal fractures of the tibia are often associated with significant soft tissue injury. The key point in management of this injury is to recognize the importance of the soft tissue component [2].
The final result of any operative intervention of pilon fractures is dependent on the severity of injury and stability of reduction with soft tissue conditions [6].
The biological fixation technique for pilon fractures is technically beneficial for fracture fixation. It reduces the injury to the soft parts and also does not compromise on the vascularity around the fracture site [6].
Ruedi TP and Allgower M published a classification for intra-articular fractures of distal tibia in 1979 [7,8].
The classification is
Type I: Intra-articular fracture of the distal tibia without significant displacement.
Type II: Intra-articular fracture of the distal tibia with significant displacement but minimal comminution.
Type III: Fracture of distal tibia with severe comminution and significant intra-articular displacement.
Two of the 18 patients presented with Ruedi Allgower class I pilon fractures. Thirteen patients presented with class II. Three patients presented with class III pilon fractures. Class II pilon fractures were the majority in presentation.
Sirkin et al., published a staged protocol in management of pilon fractures [9]. The same protocol was employed in our series.
Mazur et al., published a scoring system which was used to assess the ankle function. It provided inferences which corresponded to the score for ankle function which was graded as excellent, good, fair and poor [3,5]. The same scoring system was used to assess the ankle function in our patients. There were 12 male and six female patients showing male preponderance which is comparable to the study conducted by Bahari, et al., who reported 31 male and 11 female patients in their study [10].
A 67% of our patients were under 50 years of age hence, we noted that majority of the pilon fractures occurred in the younger age group which is comparable to studies by Yip WH, et al., Who noted an average age of 37.7 years in their cases [3].
Three of our patients had excellent scores, nine had good, five had fair and one had poor scores which were comparable to the study by Yip WH, et al., who reported to excellent to good results in six patients [3]. When the Ruedi Allgower class was compared to the Mazur’s score, class I had excellent to good score and class III had fair to poor scores. This indicated that RuediAllgower class was inversely proportional to the inference from the Mazur’s scores.
In the current series, there were 2 of 18 cases of skin slough and one patient had fixed equines deformity of the ankle, which compareable with the study by Zhang ZD et al., who has a reporting rate of 9% [8]. Zhang ZD et al., conducted a case control study on minimally invasive percutaneous locking compression plate internal fixation for treatment of type II and type III pilon fractures’ and concluded that MIPO was an effective in treatment of type II and III pilon fractures and resulted in less invasion, faster bone union with quicker recovery in ankle functions [8].
Borens O et al., conducted a study on ‘Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases’ from 1999-2001 and concluded that minimally invasive surgical technique including new low profile plate can decrease soft tissue problems while leading to fracture healing [11].
Yip WH et al., concluded in their study entitled ‘Early Experience of Metaphyseal Plating by the Minimally Invasive Plate Osteosynthesis Technique for Closed Distal Tibial Fractures’ and concluded that the results were encouraging and MIPO was a rational treatment for management of these fractures [3].
Conclusion
Minimally invasive plate osteosynthesis facilitates early mobilisation of the patient which helps in healing of the fracture. It promotes early union as it does not disturb the anatomy and physiology of vascularity at the fracture site with early return to activities. It has acceptable complication rate.
[1]. Egol KA, Wolinsky P, Koval KJ, Open reduction and internal fixation of tibial pilon fracturesFoot Ankle Clin 2000 5(4):873-85. [Google Scholar]
[2]. Serban Al, Obada B, Turcu R, Anderlik St, Botnaru V, Distal tibial fracture treated by minimally invasive plate osteosynthesis after external fixation Retrospective clinical and radiographic assessmentARS MedicaTomitana 2014 1(76):44-49. [Google Scholar]
[3]. Yip WH, Lee KB, Shen WY, Early experience of metaphyseal plating by the minimally invasive plate osteosynthesis technique for closed distal tibial fracturesHong Kong J Orthop Surg 2006 10(1):22-27. [Google Scholar]
[4]. McCann PA, Jackson M, Mitchell ST, Atkins RM, Complications of definitive open reduction and internal fixation of pilon fractures of the distal tibiaInt Orthop 2011 35(3):413-18. [Google Scholar]
[5]. Teeny Steven M, Wiss Donald A, Open reduction and internal fixation of tibial plafond fractures variables contributing to poor results and complicationsClinicalorthopaedics and Related Research 1993 292:108-11. [Google Scholar]
[6]. Gupta RK, Rohilla RK, Sangwan K, Singh V, Walia S, Locking plate fixation in distal metaphysealtibial fractures: series of 79 patientsInt Orthop 2010 34(8):1285-90. [Google Scholar]
[7]. Ruedi T, Matter P, Allgower M, Intraarticular fractures of the distal tibial endHelv Chir Acta 1968 35:556-82. [Google Scholar]
[8]. Zhang ZD, Ye XY, Shang LY, Xu RM, Zhu YZ, Case-control study on minimally invasive percutaneous locking compressionplate internal fixation for the treatment of type II and III pilon fracturesZhongguo Gu Shang 2011 24(12):1010-12. [Google Scholar]
[9]. Sirkin MS, Plating of Tibial pilon fracturesAm J Orthop 2007 36(12suppl):13-17. [Google Scholar]
[10]. Bahari S, Lenehan B, Khan H, John MP, Minimally invasive percutaneous plate fixation of distal tibia fracturesActa Orthop Belg 2007 73:635-40. [Google Scholar]
[11]. Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL, Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 casesArch Orthop Trauma Surg 2009 129(5):649-59. [Google Scholar]