Malignant Melanoma of Nasal Cavity– A Case Report
Richa Bhartiya1, K M Prasad2
1 Associate Professor, Department of Pathology, Patna Medical College & Hospital, Patna, India.
2 Assistant Professor, Department of Pathology, Patna Medical College & Hospital, Patna, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Richa Bhartiya, C/o Shri V K Shrivastava, Bungalow No. 882, Railway Officers’ Colony, North of Shiv Mandir, Danapur (Khagaul)-801105, Patna, India. E-mail : richabhartiya1972@gmail.com
Malignant Melanoma of nasal cavity is an extremely rare tumour and is more aggressive than its cutaneous counterpart. Primary malignant melanoma of nasal cavity arise from melanocytes located in the mucous membrane. Only 0.5% of malignant melanoma arises in nasal cavity. We report a case of malignant melanoma of the nasal cavity in a 51-year-old male who presented with swelling of nose, nasal block and epistaxis. By brush cytology and CT scan imaging, the pre operative diagnosis of malignant melanoma was made which was later confirmed by histopathology examination along with immunohistochemistry by using S100 and HMB 45. Malignant melanoma of nose is rare tumour, with aggressive behavior and poor prognosis. Rarity of this lesion warrants its mention and emphasizes the importance of considering malignant melanoma among the differential diagnosis of tumours of nose and paranasal sinuses.
Cytology, Head and neck Neoplasm, Metastasis, Mucosa
Case Report
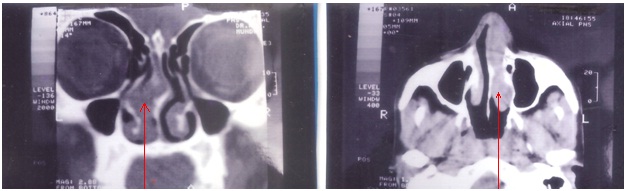
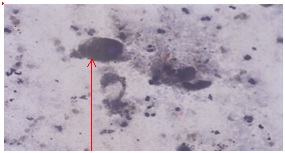
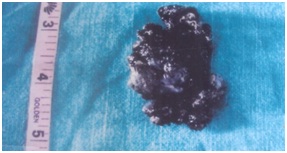
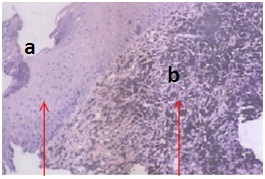
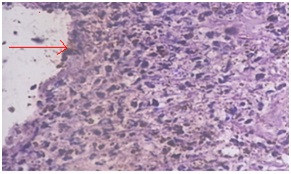
A 51-year-old male presented with nasal swelling, blockage and with occasional nasal bleeding from last 5 months. He noticed that a small swelling, approximately 1.5 cm in diameter, on the left side of nose about a month back which had rapidly increased in size. On examination, a large swelling was noticed on the left side of nose measuring 4x4 cm. The swelling was fleshy bluish-red friable and was completely blocking the nasal passage. Routine Biochemical and haematological investigations were carried out which all were in normal limits. X-ray PNS (Water’s view) showed soft-tissue shadow over the nasal region extending to left maxillary sinus. Chest X-ray showed no abnormality. CT scan findings suggested provisional diagnosis of tumour/necrosed tissue/nasal polyp [Table/Fig-1,2]. Smears were prepared for cytological interpretation by brush cytology and stained with Giemsa and Pap stains. Cytological examination showed adequate cellularity with many single, large pleomorphic undifferentiated malignant cells with moderate to abundant cytoplasm, hyperchromatic nuclei with occasional large nucleoli. The nuclear cytoplasmic ratio was increased. There was both intra and extra cellular pigment led to the provisional diagnosis of malignant melanoma of the nasal cavity [Table/Fig-3]. Later, the patient was subjected to surgery and the resected tumour was sent for histopathological examination. Gross findings consist of multiple brown-black soft tissue pieces together measuring 2.5x2x1 cm [Table/Fig-4]. On microscopic examination, Haematoxylin and Eosin stained section showed hyperplastic squamous epithelium, tumour tissue composed of spindle cells which were medium to large in size arranged in diffuse pattern. The nuclei were pleomorphic, hyperchromatic with prominent nucleoli. Focal collection of lymphocytes was also seen at places. Both intra and extra cellular brown-black pigment was noted. Scattered mitosis and tumour giant cells were also seen. The overlying epithelium was ulcerated and only few intraepithelial atypical melanocytes were seen. The diagnosis of malignant melanoma was made on light microscopy [Table/Fig-5,6], which was later confirmed by Fontana Mason Silver stain and by immunohistochemistry S-100 and HMB 45 antibodies. Postoperative radio-therapy was given to the patient and patient is alive one year after surgery.
CT scan showing non-specific hypodense soft tissue mass in left nasal cavity extending upto left maxillary sinus
Cytosmear shows many single large pleomorphic tumour cells with hyperchromatic nucleus. Black pigment is seen both in tumour cell cytoplasm and in the background (400X Giemsa)
Multiple brown-black soft tissue pieces together measuring 2.5x2x1cm
Showing hyperplastic squamous epithelium (A) along with aggregates of tumour cells (B) in sub-epithelial area [H&E X 100].
Showing dense cellular tumour tissue consisting of spindle-shaped tumour cells with large pleomorphic nucleus. Cytoplasm of the tumour cells show brown-black pigment [H&E X 400].
Discussion
Malignant melanoma of the nasal cavity is an extremely rare tumour. Melanocytes in the mucosa of the upper respiratory tract are the progenitors of the lesion [1]. Ravid and Esteeves [2], reported that Lucke in 1869 recognized melanotic sarcoma as a distinct entity in a 52-year-old male. Batsakis et al., in their review of the topic, reported 531 cases in 1982 [3]. Malignant Melanoma of nasal cavity occurs rarely in India [4]. The first case was reported in India by Kutty and Shreedharan in 1965 [5].
The incidence of malignant melanoma is more in whites than blacks. Less than 1 per one thousand of all malignant tumours are malignant melanomas in head-neck region [6]. Malignant melanoma in head-neck account for 1.7% of all melanomas. The highest incidence of malignant melanoma of nose is between 50 and 70 years [2], whereas male-to-female ratio is 2:1 [6]. In our case, patient is 51-year-old male, which corroborates with the above findings. The first and most prevalent symptom is unilateral nasal obstruction [2], nasal congestion and bleeding are reported to be the commonest symptoms in literature. The less striking symptoms are those of nasal discharge, swelling and deformity of the nose and headache [2]. Pain is a rare symptom but when present it is usually due to pressure and sinus blockage. Duration of the symptom is variable between 3 to 24 months [2]. In our case, patient presented with the symptom of nasal swelling, blockage and epistaxis, which are similar to the symptoms mentioned above. There has been discussion regarding the method used to confirm the clinical diagnosis. According to some studies, incisional biopsy is contraindicated, as this may increase metastatic spread and therefore, reduces survival rate. However, some reports have shown no difference in survival.
Cytology is certainly a quick and simple method of obtaining a rapid diagnosis although it should be done with care as these lesions are apt to bleed [7]. The cytological findings are cellular smears with single-cell population showing high nuclear cytoplasmic ratios with hyperchromatic nuclei with large nucleoli. Binucleated and multinucleated cells are frequent. The pigment is seen both within the cytoplasm and in the background. Histologically, melanoma is variable in appearance and it may look like anything [8]. On histopathological examination, grossly, the size of the tumour varies from the size of pea to large mass. The primary intra-nasal melanoma is usually polypoidal, obstructive, grayish-black or brown. On microscopic examination, histological picture of mucosal melanoma of nose display greater anaplasia than cutaneous melanoma [2,6]. The primary malignant melanoma of the nose should show junctional changes within the mucosa [2]. Presence of intraepithelial atypical melanocytes favours primary neoplasm and in its absence they must be looked upon as metastatic in nature. Exclusion of sarcoma or undifferentiated carcinoma may be sometimes difficult but familiarity with the characteristic histo-pathological pattern of melanomas of the nose, together with the presence of melanin pigment should be of great aid in this respect. It is important to ascertain that the pigment is melanin not haemo-siderin. This may be done with staining the tissue both with prussion blue and with Masson-Fontana silver stain and later will bring out the melanin pigment more clearly even when present in the smallest amount. The immuno-histo-chemical stains, S-100 and melanoma-associated antigen HMB 45 are confirmatory. Our case stained positive for melanin by Fontana silver stain and shown positivity for S100 and HMB 45. Taking a histological biopsy however be avoided as far as possible as it may lead to dissemination of tumour cells into circulation. As a part of treatment, tumour was resected and postoperative radio-therapy was given to the patient after healing of the wound and patient is alive one-year after surgery. The usual clinical course of malignant melanoma is marked by local recurrence following excision in the adjoining structures and frequently by metastasis to the lymphnode and viscera [2]. Different chemotherapeutic regimes have been tried but all with unsatisfactory results. Despite aggressive treatment, including surgery, radiation & adjuvant therapy, 5-years survival rate is between 20 and 46% [9]. Other poor prognostic factor include: advanced age, obstructive symptoms, tumour size >3 cm, location in paranasal sinuses and nasopharynx, vascular invasion into skeletal muscle and bone, high mitotic count, marked cellular pleomorphism and distant metastasis [10].
Conclusion
The primary malignant melanoma of the nose is extremely rare entity and it must be differentiated from other tumours of the nose and paranasal sinuses. Early diagnosis and surgical treatment of the melanoma of the nose offer the only possible hope of survival and therefore, attention must be paid to the minor nasal symptoms at the earliest.
[1]. Manolidis S, Donald PJ, Malignant mucosal melanoma of the head and neck: review of the literature and report of 14 patientsCancer 1997 80:1373-86. [Google Scholar]
[2]. Ravid JM, Esteeves JA, Malignant melanoma of the nose and paranasal sinuses and juvenile melanoma of the noseArch Otolaryngol 1960 72:431-44. [Google Scholar]
[3]. Batsakis JG, Regezi JA, Soloman AR, Rice DH, The pathology of the head and neck tumours; mucosal melanomasPart B in head and neck surgery 1982 4:404-18. [Google Scholar]
[4]. Grewal DS, Lele SY, Mallya SV, Baser B, Bahal NK, Rege JD, Malignant Melanoma of nasopharynx extending to the nose with metastasis in the neckJournal of Postgraduate Medicine 1994 40(1):31-33. [Google Scholar]
[5]. Kutty MK, Shreedharan T, Malignant Melanoma of the nasal septumJ Laryngol 1965 79:249-52. [Google Scholar]
[6]. Berthelsen A, Andersen AP, Jensen S, Hansen HS, Melanomas of the mucosa in the oral cavity and the upper respiratory passagesCancer 1984 54:907-12. [Google Scholar]
[7]. Maru YK, Munjal S, Gupta Y, Brush cytology and its comparison with histopathological examination in cases of diseases of the noseJournal of Laryngology and Otology 1999 113(11):983-87. [Google Scholar]
[8]. Gupta S, Singh PA, Misra V, Jain S, Malignant melanoma of maxillary sinus: A rare entityJournal of Clinical and Diagnostic Research 2009 3:1801-04. [Google Scholar]
[9]. Lietin B, Montalban A, Louvrier C, Kemeny JL, Mom T, Gilain L, Sinonasal mucosal melanomasEur Ann Otorhinolaryngol Head Neck Dis 2010 127:70-76. [Google Scholar]
[10]. Medhi P, Biswas M, Das D, Amed S, Cytodiagnosis of mucosal malignant melanoma of nasal cavity: A case report with review of literatureJournal of Cytology 2012 29(3):208-10. [Google Scholar]