Gastrointestinal fistulas are amongst the serious complications encountered in surgical practice which have high morbidity and mortality rates. They appear to be a frustrating cause to prolong the patient’s hospital stay and cost consumptions. They lead to abnormal diversions of gastrointestinal contents, digestive juices, water, electrolytes, and nutrients from one hollow viscous to another or to the skin, causing a wide variety of pathophysiological effects. Review of literature suggests that majority of gastrointestinal fistulas (75- 85%) occur following surgery, most commonly after operations for cancer, IBD (for example, Crohn’s disease, diverticulitis), lysis of adhesions and pancreatitis but sometimes they do occur spontaneously (15-25%) again more commonly in patients with diverticular disease of the colon and other IBDs (Crohn’s disease etc). Spontaneous fistulas have also been commonly reported in cancer patients or those who have received previous radiation therapy. Few less common causes include abdominal trauma such as gunshot wound, stabbing and blunt trauma [1].
Effective and timely therapy is of utmost importance due to the consequent morbidity and mortality associated with gastrointestinal fistulas. With constant advancement, fistulas could be treated in majority of the patients yet the treatment is incredibly complex and multiple therapies are often required. Successful treatment of gastrointestinal fistulas remains a continuing challenge. Treatment options which could shorten fistula closure time are not only highly beneficial but also result in considerable hospital cost savings [2].
Development of a fistula whether postsurgery or spontaneously has several psychological aspects and the knowledge of its associated morbidity can distress the patient greatly. The psychological effect of a drainage bag and malodorous fistula fluid can have an adverse effect on body image, as can pathological changes in the skin at the fistula orifice [3]. Also, postoperative fistula almost invariably lengthens hospitalization and adds on the time taken to return to work and social activities.
Vigilance is required for complications such as fluid and electrolyte disturbances, abscess formation, infection, multi organ failure, sepsis and bleeding [1]. Most common cause of mortality in fistula is sepsis [3] although bleeding due to erosion of a large blood vessel can cause acute blood loss which is often fatal.
Hence, this study was planned to study the aetiology, clinical presentation, morbidity and mortality of enterocutaneous fistula and to evaluate the different surgical intervention techniques for closure of enterocutaneous fistula along with a comparative evaluation of different techniques for management of peristomal skin with special emphasis on aluminum paint, Karaya gum (Hollister) and Gum Acacia.
Materials and Methods
This prospective observational study was conducted in the Department of Surgery, M.L.N. Medical College, Allahabad and its associated hospital (S.R.N. Hospital, Allahabad) for a period of five years from October 2007 – December 2012. Inclusion criteria were patient admitted/referred from outside with enterocutaneous fistula, patient with planned ileostomy and colostomy. Patient with enterocutaneous fistula developed postoperatively. Exclusion criteria were pancreatic fistula, biliary fistula, spontaneous enterocutaneous fistulas e.g. Crohn’s disease.
All the patients were assessed clinically by proper history of the disease, any previous surgery and any chronic illness like tuberculosis/altered bowel habit. Cases were examined, investigations and other information were collected.
Local examination included number of fistula (single/multiple), site and type of fistula, source of fistula (small bowel, large bowel), absence or presence of distal obstruction, direct or indirect fistula, peristomal skin reaction grade (normal, inflamed, excoriation skin ulceration, maceration and extensive skin involvement), surface area involved.
Investigations included routine investigations (Hb, TLC, DLC, RBS, S. Urea, S. Creatinine) S. protein, S. albumin, Arterial blood gas (ABG), S. electrolyte, Arterial pH, Blood Urea nitrogen (BUN), S. bilirubin, SGPT, Fistulogram/Distal loopogram, USG Abdomen and if required CT Abdomen and MRI if required.
Treatment protocol
Low and some medium output fistula were treated conservatively except for indirect or multiple fistula or any other indication for surgery or TPN if required through Central or peripheral venous catheter.
Rest of medium output fistula (not responding to conservative treatment) and High output fistula were treated with definitive surgical procedure as the situation may demand any other intervention techniques.
Peristomal skin care was started from the day one of the operation and application of Aluminum paint/Karaya gum/Gum acacia after random allocation of patients with written informed consent.
Proper advice was given for application of Aluminum paint/Karaya gum/ Gum acacia.
Outcome & follow up were measured with following parameters:
Spontaneous closure after conservative treatment.
Complete cure after surgical intervention.
Recurrence after surgery.
Mortality (30 days hospital mortality).
Cause of death.
Peristomal skin changes after application of Aluminum Paint/Karaya gum/Gum acacia which included skin inflammation, excoriation, ulceration, maceration and extensive skin involvement. Changes were measured in form of skin surface area involved and number of days required for healing.
Daily observation of patients was done until they were discharged. Regular follow up was done on weekly basis, monthly and then yearly for five years.
Results
The study was conducted on 80 patients. 34 (42.5%) patients belonged to age group of 11 – 30 years. The mean age of patients was 32 years with a range of 3-70 years.
Most of the patients were male (74%). The male to female ratio was 2.8:1. Out of 80, 14 patients (17.5%) belong to pediatric age group (3-14 years). There were eight male and six female children.
Most of the fistulas (59%) belonged to the small bowel including both jejunal and ileal fistulas. The second most common fistulas belonged to the duodenum (25%) and rest of the fistulas (16%) belonged to the large bowel. Most of the patients had medium output fistulas (output between 500 & 1000ml). Percentage of patients having low and high output fistula were 25% and 21% respectively.
Most common complications in the patients of enterocutaneous fistula were skin excoriation followed by sepsis, electrolyte imbalance & malnutrition. Some patients had more than one complication. Septicaemia was present in 22 patients out of which 16 patients had other associated complication viz electrolyte imbalance and malnutrition. Electrolyte imbalance was present in 49 patients out of which 33 patients had other associated complication viz septicaemia and malnutrition. Malnutrition was present in 34 patients out of which 26 patients had other associated complication viz electrolyte imbalance and septicaemia. The incidences of electrolyte imbalance, malnutrition, sepsis found in this study were 61%, 42% and 27.5% respectively. Other complications were catheter sepsis, pneumonia (due to immobilization of the patient) and multiple organ failure as a consequence of septicaemia. Patients with fistula discharge from one orifice (usually through main wound) had high spontaneous closure rate (41%) in comparison to multiple (>1) orifice (through main wound and drain site) in which spontaneous closure rate was 37%. However the difference was not statistically significant.
[Table/Fig-1] shows the effect of serum albumin on the outcome. It was found that there is a significant statistical difference between patients with serum albumin > 3.5 gm/dL and with patients with serum albumin < 3.5 gm/dL vis-à-vis spontaneous closure rate and mortality rate.
The effect of serum albumin and the outcome
| S. Albumin | No. of patients | Spontaneous Closure (%) | Mortality (%) |
|---|
| <3.5 | 55 | 17 (40%) | 20 (36.3%) |
| >3.5 | 25 | 15 (60%) | 3 (12%) |
| Total | 80 | 32 (40%) | 23 (28.6%) |
| | x2 = 4.909, df=1p<0.05 (0.026) | x2 = 3.862, df=1,p<0.05 (0.049) |
Patients who had haemoglobin more than 10g% had lower mortality rate (25%) and higher spontaneous closure rate (55%) as compared to patients with haemoglobin less than 10g% but the difference was found to be statistically insignificant.
The spontaneous closure rate for conservative treatment was 65% and surgical treatment was 61%. The mortality with conservative treatment was 24.5% and with surgical treatment was 32.3%, but it was statistically found insignificant. The mean duration of hospital stay mean duration of stay with conservative treatment and surgical treatment were 30 days and 27 days respectively. There were 20 patients with a duodenal fistula, of which 25% underwent a spontaneous closure with conservative management. The mean duration of hospital stay was 32 days for these patients. Ten percent patients underwent surgical intervention for the closure and the mean duration of stay was 31.6 days. The overall mortality in duodenal fistula was 45%. Forty seven patients had small bowel fistula, of which 40% underwent a spontaneous closure with conservative management. The mean duration of hospital stay was 30 days for these patients. Twenty six percent patients underwent surgical intervention for the closure and the mean duration of stay was 29.8 days. The overall mortality in the small bowel fistula was 23%. There were 13 patients with a large bowel fistula, of which 61% underwent a spontaneous closure with conservative management. The mean duration of hospital stay was 22 days for these patients. Twenty three percent patients underwent surgical intervention for the closure and the mean duration of stay was 22.4 days. The overall mortality in the large bowel fistula was 15%.
[Table/Fig-2] shows various surgical procedures undertaken for closure of fistula and their respective outcome. Resection and anastomosis was done in 3 patients out of which, closure was achieved in 2 patients and there was no mortality. Primary repair was done in 6 patients 3 of these patients had duodenal leak. They underwent primary repair with omentopexy/omentopexy with strengthening with serosal patch. Three patients had small bowel leak for which primary repair was done. The closure was achieved in 4 patients who underwent primary repair. Two patients died in this group. Diversion was done in 22 patients especially in distal bowel fistula and closure was achieved in 14 patients. Eight patients died in this group.
Types and outcomes of the surgical procedures.
| Type of surgery | No. of patients | Closure | Recurrence | Mortality |
|---|
| Resection anastamosis. | 3 | 2 | 1 | 0 |
| Primary repair | 6 | 4 | 0 | 2 |
| Diversion (ileostomy/ colostomy) | 22 | 14 | 0 | 8 |
| Total | 31 | 20 | 1 | 10 |
Among three resection anastamosis done in small bowel fistula, closure was achieved in 2 patients and recurrence in 1 patient who was treated conservatively and cured. No mortality was found within this group. Primary repair was done in 3 patients with duodenal fistula and 3 patients with small bowel fistula. In duodenal fistula primary repair was done as omentopexy in 2 patients and omentopexy with serosal patient strengthening in one patient. One patient died with duodenal fistula in which primary repair was done with omentopexy. In small bowel fistula primary repair was done in all 3 patients. One patient died in this group.
[Table/Fig-3] shows the different types of nutrition during management of enterocutaneous fistula. Partial TPN was given in 14 patients and 42.9% patients had spontaneous closure and 28.6% patients achieved closure after surgical procedure (adequate TPN could not be afforded by the patients due to financial problem). The patient who had enteral feeding did not have spontaneous closure rate while 50% closure rate was achieved after surgical procedure (because all the enteral feed started after a surgical intervention like feeding jejunostomy). The patients who had oral feeds had 39.4% spontaneous closure rate and 36.4% closure was achieved after surgical procedure.
Correlation between different type of nutrition and the outcome of enterocutaneous fistula.
| Nutrition | No. of Patient | Spontaneous Closure (%) | Surgical Closure (%) |
|---|
| TPN | 14 | 6 (42.9%) | 4 (28.6%) |
| Enteral feed | 8 | 0 (0%) | 4 (50%) |
| Oral Feed | 33 | 13 (39.4%) | 12 (36.4%) |
[Table/Fig-4] shows the effect of different type of modalities (Karaya gum (Hollister kit) Gum Acacia and Aluminum Paint) on different type of skin complications/changes. The application of all the modalities shows good results for protection prior to any skin changes. Karaya gum showed some failure rates with inflamed skin (2 out of 6) and excoriated skin (1 out of 1). Aluminum paint also had some failure rate with inflamed (1 out of 4), excoriated (1 out of 1) and ulcerated (1 out of 1) skin. Gum acacia was found to be good over inflamed and excoriated skin.
Effect of different type of modalities on different type of skin, Complication/Changes.
| Skin changes | Karaya gum | Gum acacia | Aluminum paint |
|---|
| No. of patient | Healing/protection | Failure | No. of patient | Healing/protection | Failure | No. of patient | Healing/protection | Failure |
|---|
| No reaction | 16 | 15 | 0 | 7 | 7 | 0 | 10 | 15 | 0 |
| Skin inflammation | 6 | 4 | 2 | 7 | 7 | 0 | 4 | 3 | 1 |
| Excoriation | 1 | 0 | 1 | 4 | 4 | 0 | 1 | 0 | 1 |
| Ulceration | 0 | 0 | 0 | 2 | 2 | 0 | 1 | 0 | 1 |
| Maceration and extensive skin involvement | - | - | - | - | - | - | - | - | - |
[Table/Fig-5] shows the cost comparison of different modalities used in skin care. Gum Acacia has much lower cost in comparison to Karaya Gum and Aluminum paint. So Gum Acacia is good modality for patients of lower socio economic status [Table/Fig-6,7 and 8].
Cost comparison of different modalities used in skin care
| Modalities | Karaya Gum | Gum Acacia | Aluminum paint |
|---|
| Cost (Rs.)Per 100 gm. | 450 | 10 | 35 |
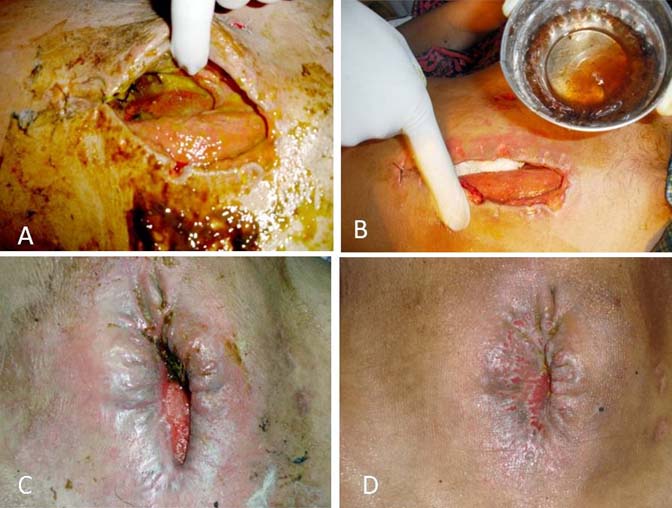
Shows effect of gum acacia on medium output small bowel fistula 1: a) At time of Admission; b) After 1 week; c) After 4 week; d) after 8 weeks.
Shows effect of gum acacia on high output duodenal fistula: a) At time of admission; b) After 2 weeks; c) 4 weeks after secondary suturing.

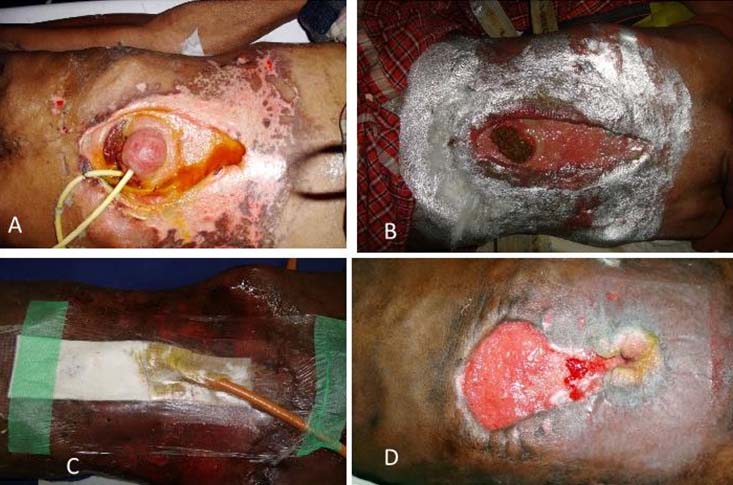
Aluminum paint application: a) High output duodenal fistula with; b) Aluminum paint application in excoriated skin; c) Condition after 2 weeks with Opsite dressing (used for holding the catheter); d) Condition after 4 weeks.
In pediatric age group (3-14 years), out of 14 patients, three (21.5%) had low output fistula, ten (71.5%) had medium output while one (7%) had high output fistula. We applied gum acacia in seven, karaya gum in five and aluminium paint in two patients. However, four patients (29%), one high output fistula and three medium output fistula expired during the study period. [Table/Fig-9] shows the outcome of various modalities, in terms of healing achieved, in pediatric as well as in adult age group.
Outcome of various modalities for skin care in enterocutaneous fistula.
| Different modalities used | | | Outcome (Healing) |
|---|
| Gum Acacia | Pediatric | 5 | 5(100 %) |
| Adult | 15 | 15 (100 %) |
| Total | 20 | 20 (100 %) |
| Karaya Gum | Pediatric | 3 | 3 (100 %) |
| Adult | 20 | 17 (85 %) |
| Total | 23 | 20 (86.9 %) |
| Aluminium paint | Pediatric | 2 | 2 (100 %) |
| Adult | 14 | 11 (78.5 %) |
| Total | 16 | 13 (81.2 %) |
Partial TPN was given in five children (three patients with gum acacia and two patients with karaya gum). Surgical intervention in form of secondary suturing was done in two patients who belonged to gum acacia group.
Discussion
In this study it is noted that most of the enterocutaneous fistulas (ECF) occurs following surgery. Ahmad et al., did his study in 70 patients of enterocutaneous fistula and concluded that most of the fistula developed postoperatively {68 (97%) out of 70 patients} [4].
Eni et al reviewed 54 patients with ECF and reported the age ranged from 1 to 58 years with two peaks of incidences at 20-29 years and 40-49 years [5].
In our study most of the fistulas belonged to the small bowel (59%) in comparison to duodenal (25%) and large bowel fistula (16%). LaBerge et al., in their study reported the various sites of fistula [6]. Out of total 53 patients they studied, maximum number of cases had small bowel fistula (51%). There were four cases each from esophagous (7.5%) and stomach (7.5%), five from duodenum (9.4%) while ten (18.8%) from colon. Colonic-small bowel anastomosis (3.7%) and Hartmann pouch (1.8%) accounted for least number of cases.
Most of fistulas (54%) in our study belonged to the medium output fistula (between 500 – 1000 ml) and the rate of high and low output fistula was 21% and 25% respectively. LaBerge et al., reported the incidence of high output fistula and low output fistula as 55% and 45% respectively [6].
However, we found that sepsis was the most common cause of death in our study as it was the main cause of multiple organ failure and renal failure; this was also seen by W Fazio et al., [7].
Most of the patients in our study were treated conservatively (61.3%) and surgical treatment was given in 38.7%. The closure rate for conservative and surgical closure was found to be 65.3% & 61.3% respectively and found statistically insignificant (p>0.05). LaBerge et al., treated 53 patients with enterocutaneous fistulas conservatively. Conservative management resulted in spontaneous fistula closure in 57% [6]. Alhan et al., did a retrospective study during a period of nine years and reported the outcome of conservative treatment with total bowel rest and parenteral nutrition, and in 56.5 percent of the cases spontaneous closure occurred within an average of 29.6 days. Mean duration of stay was 30 days for conservative treatment and 22 days for surgical closure over all mean duration of stay was 29 days [8]. Ahmad et al., did their study on 70 patients of enterocutaneous fistula and reported that the mean duration of hospital stay for all patients was 25.9 days [4].
The present study revealed that the surgical intervention is associated with high mortality rate (32.3%) in comparison to the conservative treatment (24.5%), but it was found statistically insignificant (p>0.05).
The role of fistula orifice whether single (through main wound) or multiple (through main wound and drain site) was found insignificant in this study (p>0.05). The level of haemoglobin also did not appear to have any significant difference. However, we did found that there was a significant statistical difference in the outcome of spontaneous closure between patients with serum albumin >3.5gm/dL and patients with serum albumin <3.5gm/dL vis-à-vis spontaneous closure rate and mortality rate. Vector W Fazio et al., found that hypoalbuminaemia and anaemia was strongly associated with increased mortality rate of ECF [7].
Different types of nutrition were given during management of enterocutaneous fistulas. Partial TPN was given in 14 patients and 42.9% patients had spontaneous closure and 28.6% patients achieved closure after surgical procedure (adequate TPN could not be afforded by the patients due to financial problem). The patient who had enteral feeding had 0% spontaneous closure rate and 50% closure rate was achieved after surgical procedure (because of the enteral feeds started after a surgical intervention like feeding jejunostomy). The patients who had oral feeds had 39.4% spontaneous closure rate and 36.4% closure was achieved after surgical procedure.
The surgical procedures done for the closure of enterocutaneous fistula were resection and anastomosis, primary repair and diversion (defunctioning stoma). All the surgeries were done as early surgery within two weeks from the primary surgery on appearance of fecal matter in the wound. Most of the patients with distal bowel fistulas were treated with surgical intervention as a diversion or defunctioning stoma in our study. However, good surgical outcome has also been reported to be achieved by resection anastamosis [9]. Twenty two patients managed with this surgical intervention and 14 patients successfully achieved closure of fistula. Eight patients died in this group. During follow up, ileostomy closure was done in only 3 patients successfully who had achieved better nutritional status. The advantage of defunctioning stoma was that it helped in closure of enterocutaneous fistulas distal to the defunctioning stoma and it allows the early oral feed to the patients which helped to improve the nutritional status of the patients.
The different agents were used and evaluated for their role in peristomal skin care. Review of literature does not show much literature regarding comparison between modality of care for peristomal skin. Different material used for peristomal care are betel leaf [10,11], petrolatum jelly [12], glycerine hydrogel based wound dressing [13], and Acacia Senegal or Gum acacia [14].
We found that application of Karaya Gum (Hollister Kit), Gum Acacia and Aluminum Paint gave almost similar outcome since the difference in their outcome was not found to be statistically significant (p>0.05), but role of Gum Acacia was found to be good with inflamed, excoriated and ulcerative skin in comparison to Aluminum Paint as efficacious as Karaya Gum but at a much lower cost.
Conclusion
Postoperative fistulas are the most common aetiology of enterocutaneous fistula. Malnutrition, sepsis and electrolyte imbalance are the most common contributory factors to increase morbidity and mortality in enterocutaneous fistula. Septicaemia followed by multiple organ failure appears to be most common cause of death in patients with enterocutaneous fistula.
Most of the patients of enterocutaneous fistula were managed conservatively but surgical management remains the treatment of choice in distal bowel fistula and had good role in decreasing mortality and hospital stay as well.
Skin care around stoma or wound done with Karaya Gum, Gum Acacia and Aluminum Paint has almost equal efficiency in management of skin excoriation. However Gum Acacia was found to be cost effective option for low socioeconomic status people particularly in developing countries like India.