Fluconazole Resistant Candida Oesophagitis in Immunocompetent Patients: Is Empirical Therapy Justifiable?
Barnali Kakati1, Aarti Kotwal2, Debasis Biswas3, Shantanu Sahu4
1 Associate Professor, Department of Microbiology, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, India.
2 Associate Professor, Department of Microbiology, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, India.
3 Additional Professor, Department of Microbiology, AIIMS, Bhopal, Saket Nagar, Bhopal, India.
4 Professor, Department of Surgery, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aarti Kotwal, Associate Professor, Department of Microbiology, Himalayan Institute of Medical Sciences, Jolly Grant, Dehradun-248146, India.
E-mail: aartiraghuvanshi@yahoo.co.in
Introduction
C. albicans (Candida albicans) is the foremost cause of fungal oesophagitis, however other species such as Candida tropicalis,Candida krusei and Candidastellatoidea have also been implicated to cause this condition. Although, numerous studies have identified risk factors for C. albicans oesophagitis, data for non- C. albicans species is still sparse.
Aim
To determine the aetiology of Candida oesophagitis in our medical centre over a two year period. Additionally, to investigate predisposing conditions for oesophageal candidiasis caused by different Candida species.
Material and Methods
All consecutive patients posted for upper gastrointestinal endoscopy at the endoscopy unit of a tertiary care hospital in north India with findings consistent with oesophagitis were screened for the presence of Candida oesophagitis by performing KOH (potassium hydroxide) examination and culture on SDA (Sabouraud’s dextrose agar). Antifungal susceptibility testing as per CLSI guidelines was performed for fluconazole, a most common empirically prescribed antifungal for the condition.
Results
A total of 1868 patients with no known immune-compromised condition underwent upper gastroscopy at our centre during the study period. The prevalence of Candida oesophagitis was 8.7% (n = 163). C. albicans was recovered from majority of infections (52.1%), followed by C. tropicalis (24%), C. parapsilosis (13.4%), C. glabrata (6.9%) and C. krusei (3.6%). Alarmingly, among the C. albicans isolates 8.6% were resistant to fluconazole.
Conclusion
With rising reports of antifungal drug resistance among the isolates of Candida species, an increasing prevalence of this organism could have an impact on the treatment of Candidal oesophagitis and it should be approached with caution by the clinician.
Antifungal susceptibility testing, Acid suppression therapy, Candidiasis
Introduction
Candida oesophagitis (OC) although, in the absence of predisposing factors is mainly a disease of the old age, possibly related to oesophageal dysmotility disorders, immune-suppression or defective carbohydrate metabolism. This disease is mostly observed in the immune-compromised host especially the debilitated patients who have received broad-spectrum antibiotics, corticosteroids or immune-suppressants [1,2]. However, with the improvement in flexible endoscopes and increase in its use, direct visualization and sample collection has become easier, and thus the diagnosis of new cases has enhanced [3]. The National Hospital Discharge Survey reports a rise in rates of oro-pharyngeal candidiasis by more than 4-fold between 1980 and 1989 in the United States [4].
Although C. albicans (Candida albicans) is the most common species implicated in Candida oesophagitis other Candida species like C. glabrata (Candida glabrata),C. parapsilosis (Candida parapsilosis), C. krusei (Candida krusei),C. stellatoideae (Candida stellatoideae) and C. tropicalis (Candida tropicalis) are often reported to be the causative agents [5]. With growing concerns about the emerging resistance to azoles among C. albicans species, varying susceptibility among the non-albicans species huge importance is being attached to species and drug susceptibility profile of Candida [6].
Although, Candida oesophagitis is a well known entity worldwide but still the published Indian data evaluating OC is scarce. In addition, very little is known about infections caused by species other than C. albicans.
Materials and Methods
In this descriptive study we have attempted to document the prevalence of Candida oesophagitis, predisposing factors, species distribution and susceptibility profile of isolated species over a 24-month period from January 2011 till December 2013 in a single medical centre. Patients posted for upper gastrointestinal endoscopy at the endoscopy unit of a tertiary care hospital in north India during two year period with findings consistent with Candida oesophagitis were included in the study. The study protocol was approved by the institutional ethics committee and proper informed consent was recorded from each of the recruited patients.
A presumptive case of Candida oesophagitis was defined as a patient who had whitish plagues adhered to the mucosa of oesophagus on biopsy, a finding suggestive of Candida oesophagitis. Recurrence of Candida oesophagitis in the same patient was defined as a new episode of Candida oesophagitis one month after the remission and was considered as a new case.
Direct microscopy was done after keeping the tissue in 10% KOH solution overnight. Samples were inoculated on SDA with chloramphenicol (50mg/L) to prevent bacterial growth and additionally on Hi-Chrom Candida differential agar (CHROM agar) to improvise species identification, based on colored colony morphology. SDA slants and CHROM agar plates were incubated under 37°C for 48 hours. Isolates were further characterized by observing corn meal agar for chlamydospore production refining previous tests obtained with chromogenic media. Identification tests like germ tube test, sugar assimilation profile and sugar fermentation tests were employed for species identification. Differential growth on SDA at 37°C and 42°C for delineation of C. albicans from Candida dubliniensis was also performed.
The recovered Candida isolates were further purified in distilled water and subjected to antifungal susceptibility testing using commercially procured antifungal discs of fluconazole (Hi- media), as per standard CLSI guidelines (document M- 44A). For interpretation of sensitivity or resistance, zone size recommended by disc manufacturers was taken into consideration. A fluconazole disc of 25 μg was used. Standard ATCC strains, viz. C. albicans ATCC 90028, C. parapsilosis 22019 and C. krusei 6258 were used as control. Isolates resistant to fluconazole by disc diffusion method were further tested by broth macrodilution method as per CLSI guidelines (M27 A2) using fluconazole powder procured from Sigma-Aldrich.
Results
Of 1868 patients referred to the endoscopy unit during the study period, 163 (8.7%) had findings compatible with Candida oesophagitis. Ages ranged from 24 years to 92 years, with a mean of 62 years, 95 (58.2%) of them were elderly. Hundred and ten patients (67.4%) were male and 53 (32.5%) females. Candida oesophagitis episodes were more frequent among elderly males (n=82, 50.3%).
Most common symptoms were heartburn (47.6%), odynophagia (23.1%), nausea and vomiting (16.4%) and (11.6%) patients were asymptomatic with the indication of endoscopy being malignancy, diabetes, long term steroid use etc. [Table/Fig-1] depicts the co-morbidities associated with the development of Candida oesophagitis in our study. The most frequent co morbidities were old age (63/95, 66.3%), COPD (Chronic obstructive pulmonary disease) (12/34, 35.3%), diabetes mellitus (6/14,43%), malignancies (0/1), chronic liver disease (0/2). It was noted that not even a single patient of gastro-oesophageal reflux disease had features of Candida oesophagitis.
Conditions associated with the development of Candida oesophagitis
| Associated conditions | Number of patients | Candida oesophagitis |
|---|
| Old age | 95 | 63(66.3%) |
| COPD | 34 | 12(35.29%) |
| Reflux disease | 29 | 0 |
| Diabetes | 14 | 6(42.85%) |
| Malignancy | 1 | 0 |
| Chronic liver disease | 2 | 0 |
COPD: Chronic obstructive pulmonary disease
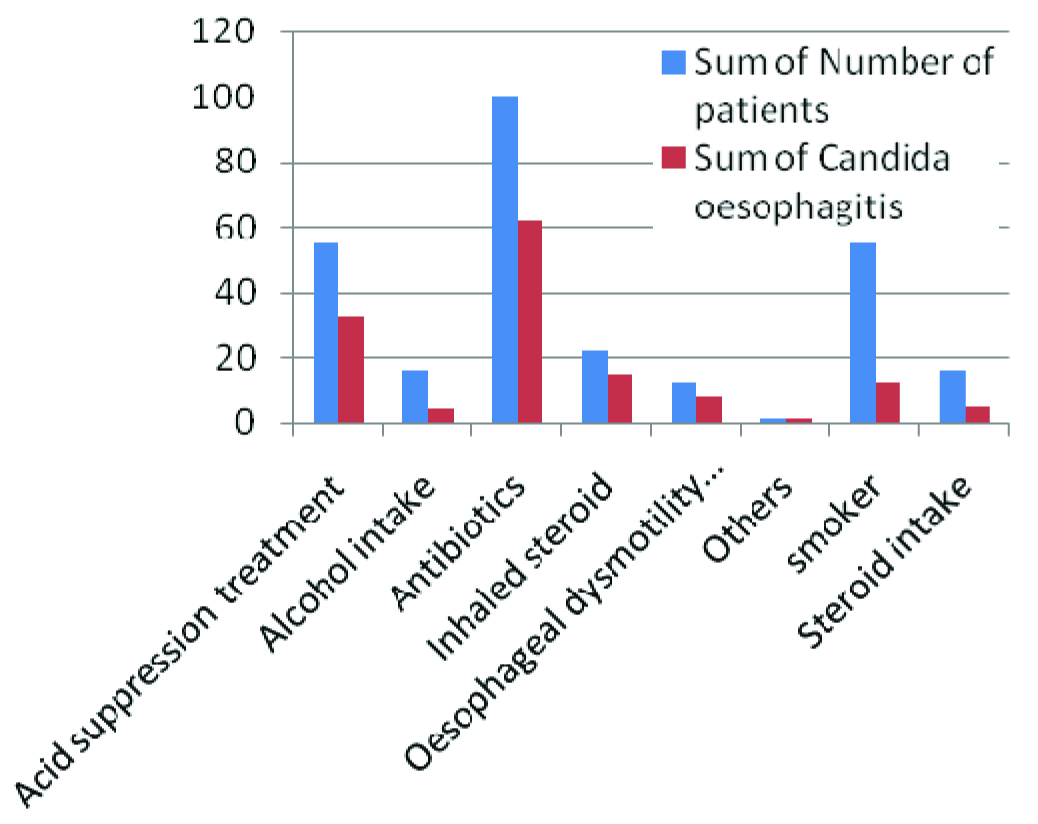
[Table/Fig-2] shows the associations of the risk factors with the Candida oesophagitis. The putative conditions posing a risk of Candida oesophagitis were antibiotic usage (62/100, 62%), alcohol intake (4/16, 25%), acid suppression therapy (32/55, 58.2%) smoking (12/55, 21.8%), and inhaled steroid intake (15/22, 68.2%). Twelve of our patients had oesophageal dysmotility disorders and one patient was HIV positive. C. albicans (n=85; 52.1%) was the species most often isolated from biopsy samples, followed by C. tropicalis (n=39; 24%), C. parapsilosis (n=22; 13.4%), C. glabrata (n=11;6.9%,) and C. krusei (n=6, 3.6%).
Risk factors associated with the development of Candida oesophagitis
The results of in vitro antifungal susceptibility testing performed by Disc Diffusion technique on the recovered isolates revealed that 8.6% (13 out of 163) of the isolates were resistant to fluconazole [Table/Fig-3]. An alarming finding was that 50% of the isolates of C. krusei were resistant to fluconazole. Whereas resistance among other species varied, with 5/11 (45.4%) of isolates of C. glabrata, 1/39 (2.5%) and 3/85 (3.5%) isolates each of C. tropicalis and C. albicans respectively being resistant to fluconazole. Antifungal susceptibility testing of the resistant isolates by broth macrodilution method revealed 100% concordance with disc diffusion method except in case of one isolate of C. parapsilosis which was sensitive by disc diffusion method but resistant by broth macrodilution method.
Antifungal sensitivity profile of the recovered isolates
| Isolates | Number (%)N=163 | Resistance (%) to Fu |
|---|
| DD | BM |
|---|
| C. albicans | 85(52.1%) | 3(3.5%) | 3 |
| C. tropicalis | 39(24%) | 1(2.5%) | 1 |
| C. parapsilosis | 22(13.4%) | 1(4.5%) | 2 |
| C.glabrata | 11(6.9%) | 5(45.4%) | 5 |
| C.krusei | 6(3.6%) | 3(50%) | 3 |
Fu= Fluconazole; DD-Disc diffusion;BM-Broth macrodilution
Discussion
Our study highlights the finding that Candida oesophagitis previously reported in immunocompromised persons is becoming more common among individuals with intact immune system as well. The frequency of Candida oesophagitis in this study involving 1868 immune-competent patients submitted to upper gastrointestinal endoscopy was 8.72%. An interesting finding was significant association of the condition in elderly. A possible reason to this may be an increase in oesophageal dysmotility, impairment of immunity or defective carbohydrate metabolism with rising age. Many authors have reported this in their studies and have proposed Candida oesophagitis a disease of elderly in the absence of other predisposing factors [7]. The second major association with Candida oesophagitis was found to be COPD. As suggested by Kesten et al., it is explained by the fact that patients of COPD during acute exacerbations are put on a combination of antibacterials and inhaled corticosteroids and usage of antibiotics eliminate bacterial competition for nutrients allowing overgrowth of Candida, inhaled corticosteroids on the other hand lead to mild immune compromise [8]. Interestingly, GERD (Gastro-oesophageal reflux disease) was protective against colonization by Candida with none of the patient of GERD developing Candida oesophagitis.
We also noted that there was significant association of Candida oesophagitis with intake of histamine H2-receptor antagonists or proton pump inhibitors (PPIs) with higher yield in rate of isolation of Candida in patients on these medications. One reason for this might be that these agents raise the local pH of the oesophagus and make the environment more conducive to Candidal growth. As it is a known fact that gastric acidity is an essential barrier for control of most microorganisms, thus its inhibition can allow a number of infections to occur. In addition omeprazole is known to decrease the salivary secretion which can facilitate the growth of Candida in the mouth and can further help in its spread to the stomach [9,10].
In our study the commonest species isolated was C. albicans (n=85, 52.1%), followed by C. tropicalis (n=39, 24%), C.parapsilosis (n-22, 13.4%), C. glabrata (n=17, 6.9%) and C. krusei (n=6, 3.6%). Similar findings have been reported by authors with C. albicans being the commonest species identified in patients with Candida oesophagitis world over [11–14]. What is alarming is that 8.6% of our isolates were resistant to fluconazole. As fluconazole is a drug of choice for the treatment of Candida oesophagitis, its irrational and empirical use might be the reason of high fluconazole resistance. This is similar to data published in recent years in which azole resistance has been found to be higher among isolates of Candida isolated from Candida oesophagitis [12,15].
Conclusion
Candida oesophagitis among immunocompetent is becoming a common entity and fluconazole is empirically prescribed in these group of patients. The finding of 8.6% of fluconazole resistance among the Candida isolates in the present study underscores the importance of routine testing of antifungal susceptibility among Candida oesophagitis patients. Other antifungals like ketoconazole and voiconazole which could not be included in the present study due to financial constraints should also be tested for efficacy against the resistant isolates.
COPD: Chronic obstructive pulmonary disease
Fu= Fluconazole; DD-Disc diffusion;BM-Broth macrodilution
[1]. Baher PH, McDonald GB, Oesophageal infections: risk factors, presentation, diagnosis, and treatmentGastroenterology 1994 106:509-32. [Google Scholar]
[2]. Simon MR, Houser WL, Smith KA, Oesophageal candidiasis as a complication of inhaled corticosteroidsAnn Allergy Asthma Immunol 1997 79:333-38. [Google Scholar]
[3]. McCloy RF, EndoscopyCurr Opin Gastroenterol 1987 3:967-70. [Google Scholar]
[4]. Banerjee SN, Emori TG, Culver DH, Gaynes RP, Jarvis WR, Horan T, Secular trends in nosocomial primary bloodstream infections in the United States, 1980–1989 National Nosocomial Infections Surveillance SystemAm J Med 1991 91:86S-89S. [Google Scholar]
[5]. Naito Y, Yoshikawa T, Oyamada H, Oesophageal candidiasisGastroent Jap 1988 23:363-70. [Google Scholar]
[6]. Kotwal A, Biswas D, Sharma JP, Gupta A, Jindal P, An observational study on the epidemiological and mycological profile of Candidemia in ICU patientsMed Sci Monit 2011 17(11):663-68. [Google Scholar]
[7]. Weerasuriya N, Snape J, Candida oesophagitis in elderly patients: risk factors, prevention and managementDrugs Aging 2008 25(2):119-30. [Google Scholar]
[8]. Kesten S, Hyland RH, Pruzanski WR, Kortan PP, Oesophageal candidiasis associated with beclomethasone dipropionate aerosol therapyDrug Intell Clin Pharm 1988 22(7-8):568-69. [Google Scholar]
[9]. Karmeli Y, Stalnikowitz R, Eliakim R, Rahav G, Conventional dose of omeprazole alters gastric floraDig Dis Sci 1995 40:2070-73. [Google Scholar]
[10]. Kochhar R, Talwar P, Singh S, Mehta SK, Invasive candidiasis following cimetidine therapyAm J Gastroenterol 1988 83:102-03. [Google Scholar]
[11]. Kliemann DA, Pasqualotto AC, Falavigna M, Giaretta T, Severo LC, Candida oesophagitis: species distribution and risk factors for infectionRev Inst Med trop S Paulo 2008 50(5):261-63. [Google Scholar]
[12]. Maninder J, Usha AJ, Isolation, characterization and antifungal susceptibility pattern of Candida species causing oropharyngeal candidiasis in HIV positive patientsCommun Dis 2008 40(3):177-81. [Google Scholar]
[13]. Lunel FV, Koeleman JG, Spanjaard L, Trends in fungaemia and antifungal susceptibility in the NetherlandsNeth J Med 2006 64(7):236-42. [Google Scholar]
[14]. Narain S, Neonatal systemic Candidiasis in a tertiary care centerInd J Med Microbiol 2003 21:56-58. [Google Scholar]
[15]. Nadagir SD, Chunchanur SK, Halesh LH, Yasmeen K, Chandrasekhar MR, Patil BS, Significance of isolation and drug susceptibility testing of non-Candida albicans species causing oropharyngeal candidiasis in HIV patientsSoutheast Asian J Trop Med Public Health 2008 39(3):492-95. [Google Scholar]