Introduction
Functional echocardiography, as opposed to echocardiography as performed by the cardiologist, is the bedside utilization of cardiac ultrasound to take after functional and haemodynamic changes longitudinally. Information reflecting cardiovascular capacity and systemic and pulmonary blood flow in sick preterm and term neonates can be observed utilizing this strategy. Information is lacking on its use in neonatal units in India.
Aim
To characterize the impact of Functional neonatal echocardiography (FnECHO) programme on decision making in a tertiary care centre in India by evaluating its frequency of use, patient characteristics, and indications.
Materials and Methods
Prospective observational study of neonates in a tertiary Neonatal Intensive Care Unit (NICU) in Pune (India) from February 2014 to January 2015. All the neonates undergoing FnECHO during this 12 month period based on clinical findings were included in the study. Data extracted from the review of the clinical notes included gestational age, birth-weight, mode of delivery, Apgar scores, details of respiratory and cardiovascular support, timing of FnECHO and any other clinical diagnosis. The findings of echocardiography were recorded and correlated with the clinical and other laboratory or X-ray findings. If these findings indicated a change in management, it was instituted.
Results
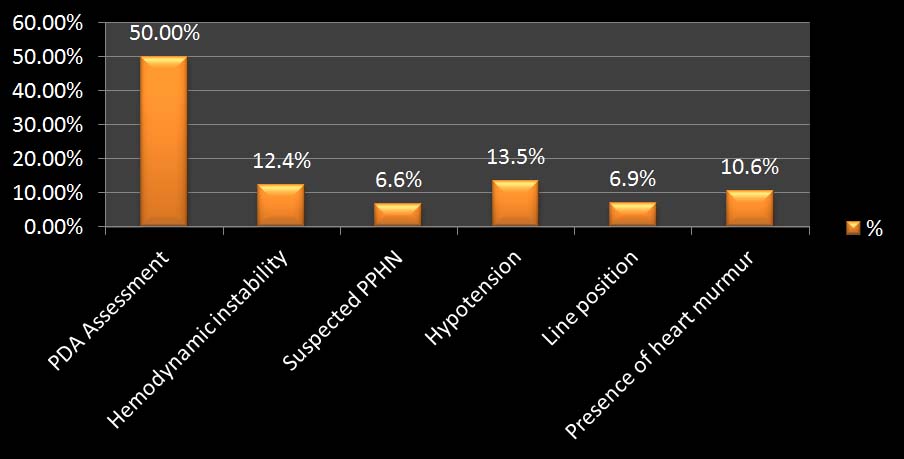
A total of 348 echocardiographic studies were performed in 187 neonates (mean 1.86; SD 2.02). The most frequent indication was Patent Ductus Arteriosus (PDA) assessment (n= 174, 50%), followed by haemodynamic instability (n=43, 12.36%). The results of FnECHO modified treatment in 148 cases (42.50%) in the form of addition and/or change in the treatment or avoidance of unnecessary intervention.
Conclusion
FnECHO is frequently used in the NICU setting and may be a useful tool to guide treatment. PDA assessment and haemodynamic instability are the most frequent indications. To validate its usefulness, well co-ordinated large prospective studies are needed.
Introduction
Boundless utilization of echocardiography in NICUs around the globe has been seen because of scaling down of the innovation and expanding accessibility of ultrasound scanners and gifted professionals [1]. Over the past few years, the role of echocardiography in the Neonatal Intensive Care Unit (NICU) has been changed. Beforehand, just Paediatric Cardiologists were performing the echocardiographic studies in the NICU for diagnosing and monitoring Congenital Heart Disease (CHD) and for the screening of Patent Ductus Arteriosus (PDA) in preterm neonates. All the more as of late, it is watched that neonatologists are likewise intrigued by the echocardiographic evaluation of haemodynamic instability in neonates. As an adjunct in neonatal clinical appraisal of the haemodynamic status, new terms, for example, functional echocardiography (FnECHO) and point of care echo cardiography have been presented [1–4].
The essential objective of FnECHO is to give non-invasive information on the fundamental cardiovascular pathophysiology bringing about haemodynamic unsteadiness. It additionally serves to study the response to treatment in an individual neonate over a period of time. It is difficult to define the most appropriate criteria for the FnECHO. The current indications used for FnECHO have been primarily established on the basis of clinical experience in a growing number of neonatal units and recent observational studies and not on the basis of large clinical studies [5]. It is vital to understand that FnECHO is not expected as a substitute for the assessment of a neonate with suspected CHD by a qualified paediatric cardiologist. On the off chance that basic CHD or critical arrhythmia is clinically suspected in a neonate, the infant ought to be clinically evaluated by a paediatric cardiologist, and echocardiography should be performed by a person trained in paediatric echocardiography and reviewed by a paediatric cardiologist [6–8].
Currently there are no published data on the use of FnECHO in Indian NICUs. In our tertiary NICU, we have been using FnECHO for five years. The present study was undertaken to study the various indications for FnECHO and its usefulness in clinical decision making in a tertiary care centre in India. This is a prospective observational study on the use of FnECHO in an Indian NICU during a 12 month period, in which we sought to analyse frequency and indications of FnECHO use, and effects of FnECHO on the management of neonates.
Materials and Methods
This prospective study was conducted in the Department of Neonatology of tertiary care University Medical College and Hospital, Pune. This is a 40 bedded NICU with annual admission of about 1250 neonates. The study was done over a period of 12 months from February 2014 to January 2015. Every examination was performed at the request of the physicians in charge according to need. Each and every study of FnEHO was performed by neonatologist who bears more than five years experience in neonatal FnECHO. When an ultrasound was done, the results were discussed with the physicians in charge to decide on the therapeutic approach.
Inclusion criteria
All the neonates undergoing FnECHO (as per request of physician in charge) during this 12 month period based on clinical findings.
Exclusion criteria
Prior diagnosed cases of structural cardiac defects by Paediatric Cardiologist.
FnECHO performed on neonates out of the study duration.
Data extracted from the review of the clinical notes included gestational age, birth-weight, mode of delivery, Apgar scores, details of respiratory and cardiovascular support, timing of FnECHO and any other clinical diagnosis. The echocardiographic examination was performed by single user by echocardiographic machines with a neonatal probe (Acuson X 300, Siemens Medical Solutions USA, Inc. Probe: P8-4 Transducer Frequency Bandwidth: 8–4 MHz). Infection control precautions were followed while performing the scans. The first scan included all the standard views (long axis, short axis etc). Follow-up scans included the views as required for the particular indication. The findings of echocardiography were recorded and correlated with the clinical and other laboratory or X-ray findings. If these findings indicated a change in management, it was instituted. The collected data was entered in Microsoft Excel (Microsoft Corp, Redmond, WA, USA) spreadsheet and descriptive statistics were used. The study was approved by the hospital ethics committee.
Results
During the study period, a total of 187 neonates were enrolled in the study on whom FnECHO was performed for various indications. Some neonates required more than one FnECHO study either to monitor response and/or as per need warranted by clinical situation. Thus total of 348 echocardiographic studies were performed in these 187 neonates (mean 1.86, SD 2.02).
[Table/Fig-1] gives the details of the enrolled neonates. More than half of the neonates (67.4%) were male and majority were preterm. The mean gestational age of the neonates in the study was 34.9 weeks (SD±4.8 weeks). The mean birth weight of neonates in the study was 1.90 kg (SD±0.7kg). [Table/Fig-2] describes the distribution of study subjects according to indication of FnECHO. [Table/Fig-3] shows the details of respiratory support that the neonates were receiving at the time of FnECHO scans. [Table/Fig-4] depict the timing of first scan from hospitalization. In 55.4% cases echocardiography was done within 24 hours of admission whereas in only 16.6% cases it was done after 72 hours of admission.
| Variable | No. (n=187) | % |
|---|
| Sex | Male | 126 | 67.4 |
| Female | 61 | 32.6 |
| Gestational age | < 28 weeks | 24 | 12.8 |
| 28-31.9 weeks | 41 | 21.9 |
| 32-36.9 weeks | 48 | 25.7 |
| Term (37 – 41.9) | 71 | 38 |
| Post term (≥ 42 weeks) | 03 | 1.6 |
| Birth weight | < 1 kg | 20 | 10.7 |
| 1-1.499 kg | 51 | 27.3 |
| 1.5-2.499 kg | 70 | 37.4 |
| 2.5 -3.499 kg | 44 | 23.5 |
| ≥3.5 kg | 02 | 1.1 |
Distribution according to indication for FnECHO
*Persistent Pulmonary Hypertension of Newborn (PPHN)
Distribution according to respiratory support.
| Respiratory support | No. (n=187) | % |
|---|
| No Support | 52 | 27.8 |
| Hood O2* | 05 | 2.7 |
| CPAP† | 72 | 38.5 |
| SIMV/PSV‡ | 56 | 30 |
| A/C MODE$ | 02 | 1.1 |
(*O2: Oxygen; † CPAP: Continuous Positive Airway Pressure; ‡ SIMV/PSV: Synchronized Intermittent Mandatory Ventilation; $ A/C: Assist Control)
Timing of first scan from hospitalization
| Timing of echo | No | % |
|---|
| Within 12 h | 28 | 14.8 |
| 13 to 24 h | 76 | 40.6 |
| 25 to 48 h | 35 | 18.7 |
| 49 to 72 h | 17 | 9.1 |
| > 72 h | 31 | 16.6 |
When the impact of FnECHO on patient management was considered, following results were noted. A total of 348 echocardiographic studies were performed in 187 neonates (mean 1.86, SD 2.02). Some neonates required more than one FnECHO study either to monitor response and/or as per need warranted by clinical situation. FnECHO results led to treatment modification after 148 echo studies (42.5%). The most common modifications in the management were done in PDA patients. Haemodynamically significant PDA was diagnosed in 26.4% FnECHO. And these cases were managed by ibuprofen.
In 4% FnECHO ibuprofen was stopped before completion of full course or was not started as FnECHO was not suggestive of either haemodynamically significant PDA or it was closed.
Regarding haemodynamic instability, FnECHO led to changes in the management of 8.6% of studies. The changes involved volume expansion therapy (3.4%) and initiation or modification of inotropic therapy (5.2%). Line position was modified after 3.4% of FnECHO studies.
Discussion
The present study was conducted with the objective to study the various indications for FnECHO in a tertiary neonatal unit in India. It was also observed that the incidence of the neonates undergoing echocardiography was more in preterm (60.43%) and in low birth weight (75.4%) neonates [Table/Fig-1]. In a study conducted by AM Groves et al., the author observed that majority of the neonates undergoing echocardiography were low birth weight and preterm [9]. Thus the findings correlate with our study. In 55.61% cases echocardiography was done within 24 hours of admission [Table/Fig-4]. Echocardiography is being utilized progressively on the neonatal unit, and has been indicated to have a high return for both structural and functional cardiac abnormalities [10]. Repeated clinical examinations in the preterm newborn child give data on haemodynamic status which is of pragmatic clinical value [11]. However, such examinations include repeated handling which clashes with the broadly suggested principles of minimal handling of preterm infants [12]. Handling scenes, for example, care procedures and chest radiographs have been demonstrated to affect on both oxygen saturation and blood pressure [12,13].
It was seen that majority of the neonates in the present study undergone echocardiography were on respiratory support [Table/Fig-3]. A total of 38.50% neonates were on continuous positive airway pressure whereas 29.95% neonates were on synchronized intermittent mandatory ventilation plus pressure support ventilation.
In the present study it was observed that most common indication for echocardiography was PDA assessment (50%) [Table/Fig-2]. Following to the PDA assessment, haemodynamic instability (12.4%) and hypotension (13.5%) were the common indications. Various other indications include presence of heart murmur (10.6%), suspected PPHN (6.6%) and line position (6.9%). El-Khuffash et al., in their study noted PDA assessment (51%) as the commonest indication of ECHO [14].
Among the PDA cases majority of the neonates were low birth weight and preterm. According Koch et al., and Furzan JA et al., the incidence of a persistent PDA increases with decreasing Estimated Gestational Age (EGA) and birth weight [15,16]. FG Ramos et al., also observed echocardiography as a sensitive and specific investigation for diagnosing PDA [17].
Premature and Low Birth Weight (LBW) infants additionally constitute a critical gathering of paediatric patients with CHD, in whom remedial cardiovascular surgery is progressively performed early in life [18–20]. Echocardiography is especially imperative for preoperative determination in these patients in light of the fact that indicative heart catheterization in premature and LBW infants is connected with generally high rates of morbidity and mortality [21,22].
In the present study changes in the management was done in 39.6% patients after FnECHO, and the findings were very close to the findings reported by A. Corredera et al., and El-Kuffash with a rate of 36.89% and 41% management changes following the ultrasound examination respectively [14,23]. In our series echocardiography had helped us to confirm the clinical diagnosis and decision making of further treatment line.
Echocardiographic assessment can be broadly divided into functional and structural assessment. Functional echocardiography in the hands of an appropriately trained neonatologist is an open and valuable methodology in the neonatal intensive care unit. This tool permits the neonatologist to evaluate different parameters, e.g. ventricular outputs and SVC flow, ventricular function, pulmonary pressures and ductus arteriosus and execute prompt management as a result. It is the key that there is backing from the Paediatric Cardiologist to counteract misdiagnosis of congenital heart disease and execute further management [24].
The principle debate encompassing execution of echocardiography by a neonatologist is taking into account the potential threat of missing a Congenital Cardiopathy (CC) or making incorrect diagnosis and beginning the wrong treatment in a patient with CC. On the other hand, while this is a genuine peril, as a rule an existing structural cardiopathy is recognized by FnECHO, regardless of the fact that a complete diagnostic assessment is not made [25,26]. Either way, cardiologists and neonatologists must work in close collaboration effort, or a cardiology counsel must be asked for at whatever point there are questions. Adequate training in FnECHO is essential to minimize these risks [26].
According to Maliheh Kadivar et al., echocardiography is an important tool for diagnosis of cardiac abnormalities that can impact the management and outcome of the sick newborn in the intensive care unit. A preliminary echocardiogram performed by the neonatologist under the supervision of a paediatric cardiologist for interpretation and review is an alternate when there is not a cardiologist “in house” [27].
Limitations
There are several limitations to this study, for occurrence, small sample size. This study can’t figure out if restorative decisions would have been distinctive if FnECHO had not been accessible. Then again, besides, the very choice of performing the ultrasound test, or not, also rested with the physician in charge rather than being determined by a study protocol, which could have a considerable impact on the observed frequency of use.
Conclusion
Thus from the above discussion we could conclude that FnECHO is a useful investigation in NICU to diagnose various conditions such as PDA especially in LBW and premature neonates. Though it is not a substitute for thorough clinical examination, it has major impact on decision making in the management of various clinical conditions. However, to validate its usefulness well coordinated large prospective studies are needed.
(*O2: Oxygen; † CPAP: Continuous Positive Airway Pressure; ‡ SIMV/PSV: Synchronized Intermittent Mandatory Ventilation; $ A/C: Assist Control)
[1]. Kluckow M, Seri I, Evans N, Functional echocardiography: an emerging clinical tool for the neonatologistJ Paediatr 2007 150:125-30. [Google Scholar]
[2]. Kluckow M, Seri I, Evans N, Echocardiography and the neonatologistPaediatr Cardiol 2008 29:1043-47. [Google Scholar]
[3]. Sehgal A, McNamara PJ, Does point-of-care functional echocardiography enhance cardiovascular care in the NICU?J Perinatol 2008 28:729-35. [Google Scholar]
[4]. Sehgal A, McNamara PJ, Does echocardiography facilitate determination of haemodynamic significance attributable to the ductus arteriosus?Eur J Paediatr 2009 168:907-14. [Google Scholar]
[5]. Evans N, Gournay V, Cabanas F, Kluckow M, Leone T, Groves A, Point-of-care ultrasound in the neonatal intensive care unit: inter- national perspectivesSeminars in Fetal & Neonatal Medicine 2011 16:61-68. [Google Scholar]
[6]. Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, Functional neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for trainingEuropean Journal of Echocardiography 2011 12:715-36. [Google Scholar]
[7]. Mertens L, Helbing W, Sieverding L, Daniels O, Guidelines from the Association for european paediatric cardiology: standards for training in paediatric echocardiographyCardiol Young 2005 15:441-42. [Google Scholar]
[8]. Sanders SP, Colan SD, Cordes TM, Donofrio MT, Ensing GJ, Geva T, ACCF/ AHA/AAP recommendations for training in paediatric cardiology. Task Force 2: paediatric training guidelines for noninvasive cardiac imaging endorsed by the American Society of Echocardiography and the Society of Paediatric EchocardiographyJ Am Coll Cardiol 2005 46:1384-8. [Google Scholar]
[9]. Groves AM, Kuschel CA, Knight DB, Skinner JR, Cardiorespiratory stability during echocardiography in preterm infantsArch Dis Child 2005 90:86-87. [Google Scholar]
[10]. Moss S, Kitchiner DJ, Yoxall CW, Evaluation of echocardiography on the neonatal unitArch Dis Child Fetal Neonatal Ed 2003 88:F287-91. [Google Scholar]
[11]. Kluckow M, Evans N, Relationship between blood pressure and cardiac output in preterm infants requiring mechanical ventilationJ Paediatr 1996 129:506-12. [Google Scholar]
[12]. Murdoch DR, Darlow BA, Handling during neonatal intensive careArch Dis Child 1984 59:957-61. [Google Scholar]
[13]. Omar SY, Greisen G, Ibrahim MM, Blood pressure responses to care procedures in ventilated preterm infantsActa Paediatr Scand 1985 74:920-24. [Google Scholar]
[14]. El-Khuffash A, Herbozo C, Jain A, Lapointe A, McNamara PJ, Functional neonatal echocardiography (FnECHO) service in a Canadian neonatal intensive care unit: a 4-year experienceJ Perinatol 2013 33:687-90. [Google Scholar]
[15]. Koch J, Hensley G, Roy L, Brown S, Ramaciotti C, Rosenfeld CR, Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or lessPaediatrics 2006 117:1113-21. [Google Scholar]
[16]. Furzan JA, Reisch J, Tyson JE, Laird P, Rosenfeld CR, Incidence and risk factors for symptomatic patent ductus arteriosus among inborn very-low-birth-weight infantsEarly Hum Dev 1985 12:39-48. [Google Scholar]
[17]. FG Ramos, CR Rosenfeld, Roy L, Koch J, Ramaciotti C, Echocardiographic predictors of symptomatic patent ductus arteriosus in extremely-low-birth-weight preterm neonatesJournal of Perinatology 2010 30:535-39. [Google Scholar]
[18]. Reddy VM, Hanley FL, Cardiac surgery in infants with very low birth weightSemin Paediatr Surg 2000 9:91-95. [Google Scholar]
[19]. Bacha EA, Almodovar MA, Wessel DL, Surgery for coarctation of the aorta in infants weighing less than 2 kgAnn Thorac Surg 2001 71:1260-64. [Google Scholar]
[20]. Reddy VM, McElhinney DB, Sagrado T, Parry AJ, Teitel DF, Hanley FL, Results of 102 cases of complete repair of congenital heart defects in patients weighing 700 to 2500 gramsJ Thorac Cardiovasc Surg 1999 117:324-31. [Google Scholar]
[21]. Simpson JM, Moore P, Teitel DF, Cardiac catheterization of low birth weight infantsAm J Cardiol 2003 87:1372-77. [Google Scholar]
[22]. Rhodes JF, Asnes JD, Blaufox AD, Sommer RJ, Impact of low body weight on frequency of paediatric cardiac catheterization complicationsAm J Cardiol 2000 86:1275-78. [Google Scholar]
[23]. Corredera A, Rodríguez MJ, Arévalo P, Llorente B, Moro M, Arruza L, Functional echocardiography in neonatal intensive care: 1-Year experience in a unit in SpainAn Paediatr (Barc) 2014 81(3):167-73. [Google Scholar]
[24]. Hunter L, Patel N, Echocardiography and the neonatologistPaediatrics and child health 2011 21(6):254-57. [Google Scholar]
[25]. Skinner JR, Echocardiography on the neonatal unit: a job for the neonatologist or the cardiologist?Arch Dis Child 1998 78:401-02. [Google Scholar]
[26]. Whitehall J, Echocardiography by a neonatologistArch Dis Child 1999 80:580-81. [Google Scholar]
[27]. Kadivar M, Kiani A, Kocharian A, Shabanian R, Nasehi L, Ghajarzadeh M, Echocardiography and Management of Sick Neonates in the Intensive Care UnitCongenit Heart Dis 2008 3:325-29. [Google Scholar]