Crescentic Glomerulonephritis Associated with Pulmonary Tuberculosis
K.V. Kanodia1, A.V. Vanikar2, R.D. Patel3, K. S. Suthar4, H. L. Trivedi5
1 Professor, Department of Pathology, Laboratory Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Asarwa, Ahmedabad, India.
2 Professor and Head, Department of Pathology, Laboratory Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Asarwa, Ahmedabad, India.
3 Professor, Department of Pathology, Laboratory Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Asarwa, Ahmedabad, India.
4 Assistant Professor, Department of Pathology, Laboratory Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Asarwa, Ahmedabad, India.
5 Professor, Department of Nephrology and Transplantation Medicine and Director, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Asarwa, Ahmedabad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. KV Kanodia, Professor, Department of Pathology, Lab Medicine, Transfusion Services and Immunohematology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre and Dr. H.L. Trivedi Institute of Transplantation Sciences, Civil Hospital Campus, Asarwa, Ahmedabad, India. E-mail : kamalkanodia@yahoo.com
Tuberculosis of kidney and urinary tract is caused by members of the Mycobacterium tuberculosis complex. Kidney is usually infected by haematogenous spread of bacilli from focus of infection in the lungs. Glomerular involvement in tuberculosis presenting as a rapidly progressive glomerulonephritis is a rare entity. We report a rare case of crescentic glomerulonephritis associated with pulmonary tuberculosis in a 26-year-old man. Patient was treated with corticosteroids, haemodialysis, intravenous immunoglobulin and four cycles of plasmapheresis. He did not respond to 4-drug anti-tuberculosis treatment for renal pathology and was switched over to maintenance haemodialysis. However, he responded to pulmonary TB.
Acid-resistant bacilli, Anti-tuberculous drug, Immunofluorescence
Case Report
A 26-year old man presented with pedal oedema, cough and breathlessness for 15 days and anuria since one day. He had past history of pulmonary tuberculosis in 2004 for which he was treated with anti-tuberculosis treatment (ATT) for 6 months. On examination, he had bilateral pitting pedal oedema (++), pulse rate of 98/minute, and blood pressure of 110/70 mm Hg. On respiratory examination, crepitations and rhonchi were heard in bilateral lung middle zones. Cardiovascular and gastrointestinal system examinations were unremarkable. Investigations revealed haemoglobin, 5.7 gm/dL; white blood cell (WBC) count, 11.46 ×109/L (Neutrophils: 84%, lymphocytes: 11%, eosinophils: 3%, monocytes 2%); platelet count, 2.74 × 109/L; blood urea nitrogen, 219 mg/dL; serum creatinine, 12.26 mg/dl; total serum protein, 6.9 gm/dL; serum albumin, 1.7 gm/dL; serum sodium, 133 mmol/L; serum potassium, 5.34 mmol/L; and serum cholesterol, 99 mg/dL. Urine analysis could not be performed as patient had complete anuria.
Enzyme-linked immunosorbent assays for human immunodeficiency virus (HIV) and hepatitis C virus were negative while hepatitis B surface antigen was positive.
Chest radiograph revealed homogenous opacities in both lungs [Table/Fig-1]. Sputum for acid-resistant bacilli (ARB) was positive. Renal ultrasonography showed right kidney dimension of 10.1×4.4 cm and left kidney dimension of 10.2×4.6 cm, with increased echogenicity and maintained corticomedullary differentiation.
Chest radiograph revealing homogenous opacities in both lungs

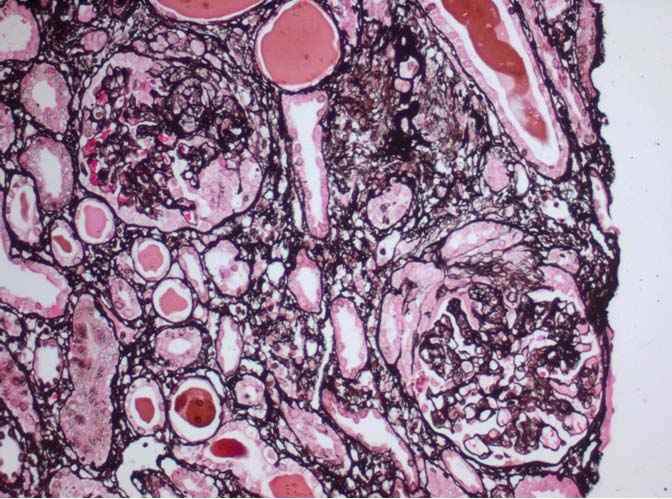
Renal biopsy was performed and after paraffin embedding, 3-μm-thick sections were prepared and stained by haematoxylin and eosin (H&E), periodic acid Schiff, Jone’s silver methenamine, and Gomori’s trichrome stains. Histopathologic examination [Table/Fig-2] showed single core of renal tissue containing 5 glomeruli with associated tubules and vessels. All the glomeruli revealed well developed circumferential cellular crescents compressing or pushing the capillary tufts towards the centres/ vascular poles. Capillary lumina were partially obliterated and infiltrated by occasional leucocytes. Capillary membranes were thickened, wrinkled and duplicated. There was mild mesangial hypercellularity with matrix accentuation. Bowman capsules were thickened. Tubules were moderately degenerated and focally atrophied. Some of the tubular lumina were filled with protenacious and cellular casts. Interstitium was moderately prominent for focal oedema and overlying scattered leucocytic infiltration. Blood vessels were unremarkable.
Photomicrograph of renal biopsy revealing glomeruli with well-developed circumferential cellular crescents compressing or pushing the capillary tufts towards the centres/ vascular poles. Capillary membranes were thickened/wrinkled/duplicated (JSM, X400)
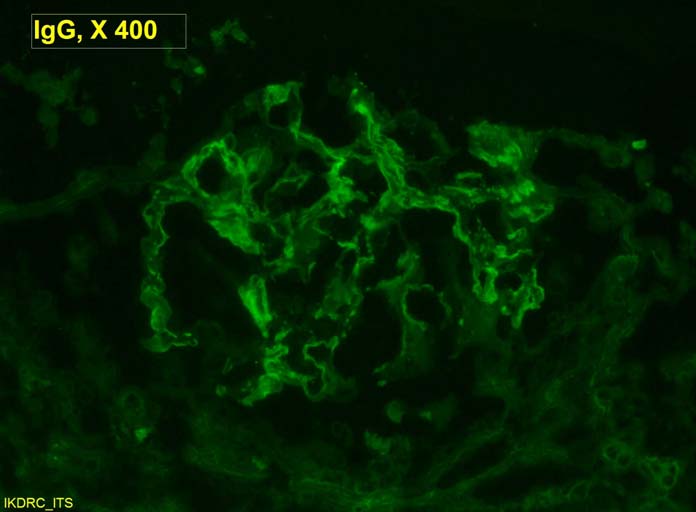
Congo red stain did not reveal birefringent amyloid fibrils. Immunofluorescence (IF) studies [Table/Fig-3] showed linear fluorescence (+2/+3) across 80-90% of glomerular capillary walls on staining with anti-human IgG and fibrinogen antisera and negative for IgM, IgA, C3 and C1q. In view of crescents, he was further investigated for vasculitis markers. Antinuclear antibody, anti-double-stranded deoxyribonucleic acid, anti-neutrophil cytoplasmic antibodies (c-ANCA/p-ANCA), anti-glomerular basement membrane (Anti-GBM) antibody, Coombs’ test, cryoglobulins and C-reactive protein were all negative and serum complement components (C3 and C4) were also normal. He was therefore diagnosed as a case of ANCA- negative crescentic glomerulonephritis associated with pulmonary tuberculosis.
Immunofluorescence studies showing linear fluorescence (+ 2/+3) across 80% to 90% of glomerular capillary walls on staining with anti-human IgG antiserum (IgG X400)
He was treated with corticosteroids, haemodialysis, Intravenous immunoglobulin and four cycles of plasmapheresis. Four-drug ATT was also started. However he did not recover and hence he had to be instituted on maintenance haemodialysis after one month of follow up.
Discussion
Tuberculosis of kidney/ urinary tract is caused by members of the Mycobacterium tuberculosis complex [1]. The kidney is usually infected by haematogenous spread of bacilli from focus of infection in lungs. Genitourinary tuberculosis can occur 10-15% of pulmonary tuberculosis and 4-5 % of all cases of extra-pulmonary tuberculosis [2–5]. Out of 16 cases of tuberculosis with GN reported in literature, 6 cases were IgA nephropathy [6–11], 2 were mesangial proliferative GN [12,13], 4 were crescentic GN [2,4,14,15], 1 case each of collapsing GN [16], mesangiocapillary [17] GN and 2 cases were of membranous nephropathy [18,19]. Crescentic GN with pulmonary tuberculosis associated with Rifampicin has also been reported [20,21].
Eastwood et al., has reported that in most of the cases of renal tuberculosis there was clinical or radiological evidence of past infection suggestive of reactivation of infection [1]. Present patient also had past history of pulmonary tuberculosis which presented as crescentic GN with reactivation of tuberculosis. Early diagnosis and treatment of tuberculosis may help to prevent risk of worsening of infection as immunosuppressive agents are used for GN. Hepatitis B virus can lead to immune complex mediated glomerulonephritis. In a study of 129 patients 73 had MGN (57%), 35 had a mesangial proliferative glomerulonephritis and 21 had membranoproliferative glomerulonephritis [22]. In our patient HBsAg was positive but there was no feature suggestive of immune complex mediated glomeruonephritidis secondary to HBsAg. In present patient although there was linear GBM IgG deposit seen on immunofluorescence, anti-GBM antibody was absent and patient did not have pulmonary haemorrhage. Similar findings were reported by Solak et al., [4]. Our patient was anuric and he was treated with haemodialysis, plasmapheresis, immunoglobulins and corticosteroids. Cyclophosphamide was not used since he had active tuberculosis. He did not respond to 4 drug-ATT and had to be instituted on maintenance haemodialysis. Similar result was also obtained in patient with IgA nephropathy with cellular cresents [23]. However, other authors have reported recovery with ATT [2,14,15]. However, our patient responded to pulmonary TB so he was not given treatment for Multi-drug-resistant tuberculosis (MDR-TB). It is proposed that renal lesions might be a consequence of tuberculosis due to the sedimentation of circulating immune-complex [2]. Shribman et al., suggested T-cell suppression may be prerequisite for immune complex nephritis in tuberculosis [12].
Conclusion
Immune complex crescentic GN with tuberculosis is a rare association, however it should be suspected in a patient with rapidly deteriorating kidney function in the background of pulmonary tuberculosis infection.
[1]. Eastwood JB, Corbishley CM, Grange JM, Tuberculosis and the kidneyJ Am Soc Nephrol 2001 12(6):1307-14. [Google Scholar]
[2]. Waikhom R, Sarkar D, Bennikal M, Pandey R, Rapidly progressive glomerulonephritis in tuberculosisSaudi J Kidney Dis Transpl 2014 25(4):872-75. [Google Scholar]
[3]. Wise GJ, Shteynshlyuger A, An update on lower urinary tract tuberculosisCurr Urol Rep 2008 9:305-13. [Google Scholar]
[4]. Solak Y, Gaipov A, Anil M, Glomerulonephritis associated with tuberculosis: A case report and literature reviewKaohsiung J Med Sci 2013 29(6):337-42. [Google Scholar]
[5]. Simon HB, Weinstein AJ, Pasternak MS, Swartz MN, Kunz LJ, Genitourinary tuberculosis. Clinical features in a general hospital populationAm J Med 1977 63(3):410-20. [Google Scholar]
[6]. Cohen AJ, Rosenstein ED, IgA nephropathy associated withdisseminated tuberculosisArch Intern Med 1985 145(3):554-56. [Google Scholar]
[7]. De Siati L, Paroli M, Ferri C, Muda AO, Bruno G, Barnaba V, Immunoglobulin A nephropathy complicating pulmonary tuberculosisAnn Diagn Pathol 1999 3(5):300-3. [Google Scholar]
[8]. Matsuzawa N, Nakabayashi K, Nagasawa T, Nakamoto Y, Nephrotic IgA nephropathy associated with disseminated tuberculosisClin Nephrol 2002 57(1):63-68. [Google Scholar]
[9]. Keven K, Ulger FA, Oztas E, Ergun I, Ekmekci Y, Ensari A, A case of pulmonary tuberculosis associated with IgAnephropathyInt J Tuberc Lung Dis 2004 8(10):1274-75. [Google Scholar]
[10]. Singh P, Khaira A, Sharma A, Dinda AK, Tiwari SC, IgAnephropathy associated with pleuropulmonarytuberculosisSingapore Med J 2009 50(7):e268-69. [Google Scholar]
[11]. Ortmann J, Schiffl H, Lang SM, Partial clinical remission of chronic IgA nephropathy with therapy of tuberculosisDtsch Med Wochenschr 2010 135(24):1228-31. [Google Scholar]
[12]. Shribman JH, Eastwood JB, Uff J, Immune complex nephritis complicating miliary tuberculosisBr Med J (Clin Res Ed) 1983 287(6405):1593-94. [Google Scholar]
[13]. O’Brien AA, Kelly P, Gaffney EF, Clancy L, Keogh JA, Immune complex glomerulonephritis secondary to tuberculosisIr J Med Sci 1990 159:187 [Google Scholar]
[14]. Sopena B, Sobrado J, Javier Perez A, Oliver J, Courel M, Palomares L, Rapidly progressive glomerulonephritis andpulmonary tuberculosisNephron 1991 57(2):251-52. [Google Scholar]
[15]. Wen YK, Chen ML, Crescentic glomerulonephritis associatedwithmiliary tuberculosisClinNephrol 2009 71(3):310-13. [Google Scholar]
[16]. Coventry S, Shoemaker LR, Collapsing glomerulopathy in a 16-year-old girl with pulmonary tuberculosis: the role of systemicinflammatory mediatorsPediatr Dev Pathol 2004 7(2):166-70. [Google Scholar]
[17]. Meyrier A, Valensi P, Sebaoun J, Mesangio-capillary glomerulonephritisand the nephrotic syndrome in the course ofdisseminated tuberculosisNephron 1988 49(4):341-42. [Google Scholar]
[18]. Yuan Q, Sun L, Feng J, Liu N, Jiang Y, Ma J, Lumbartuberculosis associated with membranous nephropathy andinterstitial nephritisJ Clin Microbiol 2010 48(6):2303-6. [Google Scholar]
[19]. Ghosh B, Pande A, Ghosh A, Banerjee A, Saha S, Membranous glomerulonephritis and tuberculous peritonitis: a rare associationJ Infect Dev Ctries 2011 5(7):550-52. [Google Scholar]
[20]. Kohler LJ1, Gohara AF, Hamilton RW, Reeves RS, Crescenticfibrillary glomerulonephritis associated with intermittent rifampin therapy for pulmonary tuberculosisClinNephrol 1994 42(4):263-65. [Google Scholar]
[21]. Murray AN, Cassidy MJ, Templecamp C, Rapidly progressive glomerulonephritis associated with rifampicin therapy for pulmonary tuberculosisNephron 1987 46(4):373-76. [Google Scholar]
[22]. Zheng XY, Wei RB, Tang L, Meta-analysis of combined therapy for adult hepatitis B virus-associated glomerulonephritisWorld J Gastoenterol 2012 18:821-32. [Google Scholar]
[23]. Fofi C, Cherubini C, Barbera G, Nicoletti MCD, Di Giulio S, Extracapillary IgA nephropathy and pulmonary tuberculosisClinical Pulmonary Medicine 2005 12:305e8 [Google Scholar]