Avascular necrosis is a devastating disease that primarily affects weight bearing joints typically presents in young patients between the ages of 20 and 40 years [1,2]. The goals of the treatment in avascular necrosis are to relieve pain and pressure of the femoral head for as long as possible. Various procedures for joint preservation have been suggested in literature [2,3]. Core decompression was recently reported to be the most commonly offered intervention for symptomatic precollapse of Avascular necrosis by American Association of Hip and Knee surgeons [3]. A current therapeutic concept for Avascular Necrosis of the femoral head is based on its early detection by magnetic resonance imaging and femoral head preservation by core decompression. Currently the treatment of avascular necrosis is guided and monitored by MR imaging [1].
Magnetic Resonance Imaging (MRI) is the most sensitive and specific imaging technique for evaluating avascular necrosis of the femoral head in early/precollapse stage [1,2,4]. The results of core decompression vary considerably in the literature [1–3]. Post surgical follow-up has been through clinical and radiographic evaluation. MRI controlled studies of the postsurgical outcomes are scarce [1].
Hence, the present study aims to analyse the MRI changes in avascular necrosis of femoral head pre and post core decompression and to identify the MRI criteria associated with successful and poor outcome.
Materials and Methods
This is a contiguous observational cohort of 40 hips treated by core decompression during 2008-2010. Patients with history of trauma and presence of collapse on radiographs were excluded from the study. Written and informed consent was obtained in all cases. Radiographic evaluation was done on standard AP and lateral radiographs. All MRI images are obtained on 1.5 T superconducting unit (ESSENZA: SEIMENS GERMANY). No specific patient preparation was required prior to the study. No contrast injection was used. All scans were performed using body coil designed for body imaging. Hips were imaged in neutral position with 0° of flexion and 10-15° of internal rotation. Images were acquired in coronal, axial and sagittal sections. The following pulse sequences were used T1W SE: Coronal/Axial. STIR/FAT SAT T2W: Coronal. FSE T2W SE: Coronal/Sagittal. Slice thickness; 5mm FOV: 300x300 mm, Image matrix: 256x256. Core decompression of the femoral head was performed within 4 weeks under C-arm guidance in regional anaesthesia. An 8 mm Michele trephine was inserted from just below the greater trochanter into the centre of the necrotic lesion to within 5 mm of the articular surface. Patients were kept non weight bearing on the affected side for 4 weeks after core decompression. Post core decompression, the radiograph and MRI scans were repeated at six months. The follow-up ranged from 6 months to 5 years.
Imaging evaluation: All the hips were staged according to Ficat and Arlet classification [5] on radiographs and only stage 1 and 2 i.e. patients with early/precollapse stage were included in our study.
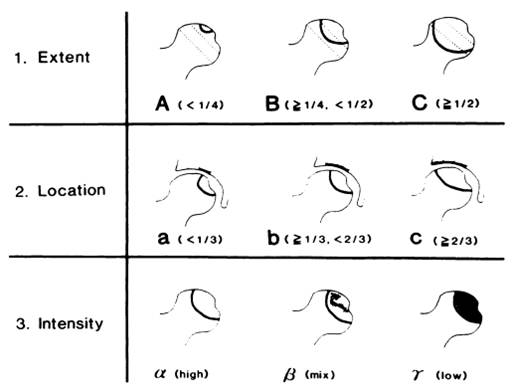
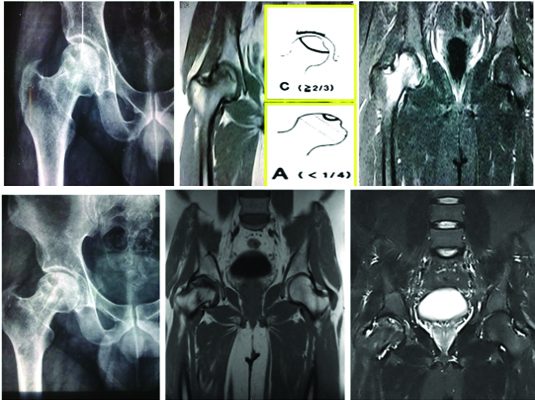
MRI evaluation was done mainly on coronal plane. Each MRI study was analysed for presence of a single line sign/a single line sign plus accompanying marrow oedema on T1W sequence or a double line sign /double line sign plus accompanying marrow oedema on T2W sequence described by Radke S et al., [1]. Coronal images obtained with the T1 W spin-echo sequence were used to analyse the extent of necrosis of the femoral head, location and intensity of the signal according to Shimizu K et al., [6] [Table/Fig-1]. Clinically, all hips were ranked by the Harris score [7] a quantitative measurement of pain, functional impairment and physical examination. A maximum score of 100 is assigned to the asymptomatic hip. Postoperative increase in HHS by 20 points and no additional femoral collapse was considered successful result clinically. End point of adverse clinical outcome dictated by fall in harris hip score was conversion or intention to convert to THR. MR parameters was also studied postoperatively for evaluation and monitoring. Also, the MRI changes associated with good/ poor outcome were documented.
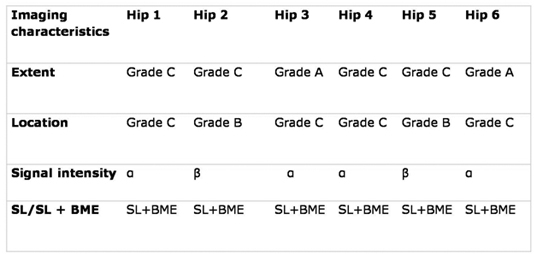
Extent: The outline of the femoral head on the coronal image was extrapolated to a complete circle; necrosis was classified as Grade A if its maximum radial distance from the circumference was less than one-fourth the diameter of the circle. The necrosis was considered to be Grade B if the distance was one-fourth to less than one-half of the diameter and Grade C if the distance was one-half the diameter or greater.
Location: The major weight bearing rim of the acetabulum as it appeared on the coronal image was divided into thirds, the measurement of the necrotic area at the articular margin of the adjacent femoral head was expressed as Grade A if it was less than one third of the weight bearing acetabular rim. Grade B if it was one third to less than two thirds and Grade C if it was two thirds or greater.
Intensity: The intensity of the signal on the coronal T1W spin echo images was classified as grade α (high), grade β (mixed) or grade γ (low).
All the data was analysed using SPSS software version. Statistical significance was accepted when p<0.05.
Results
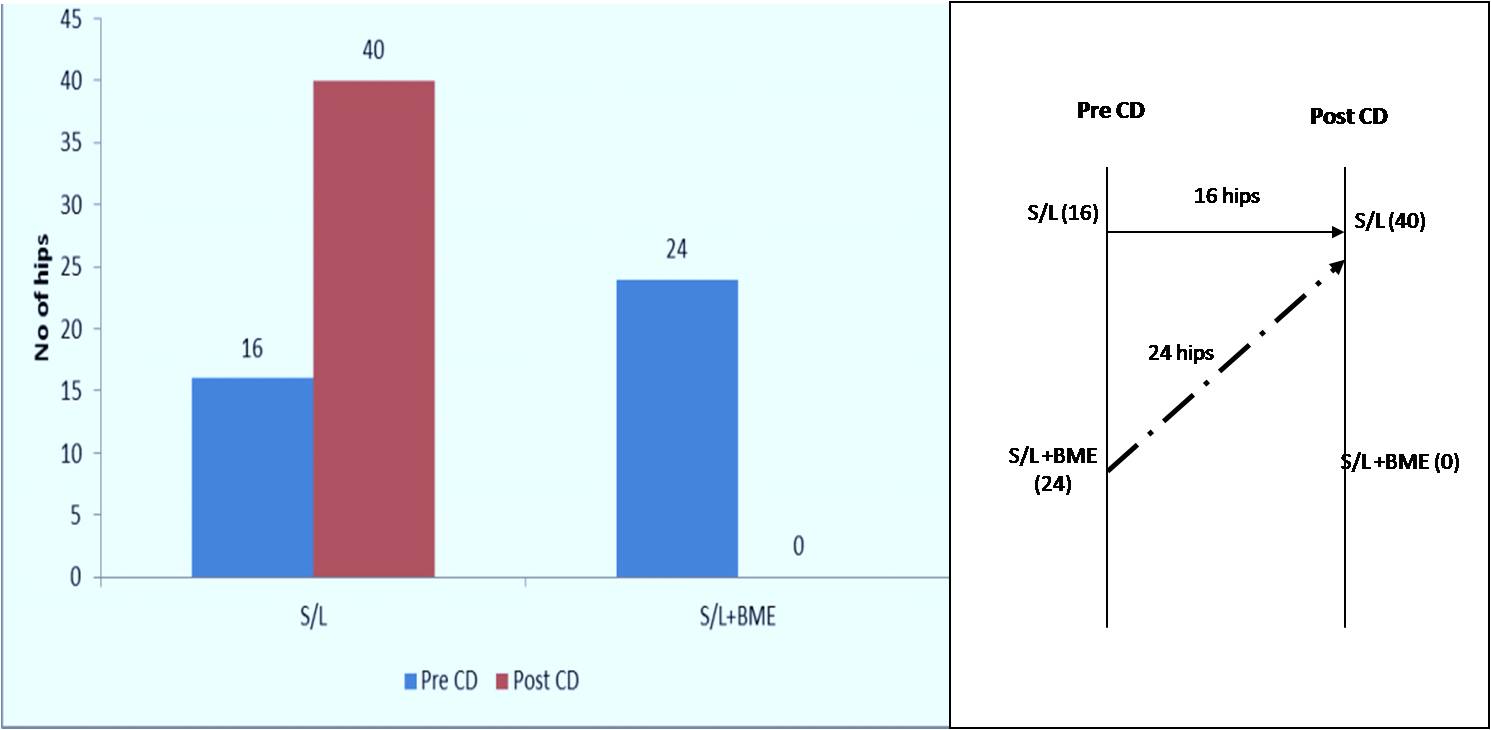
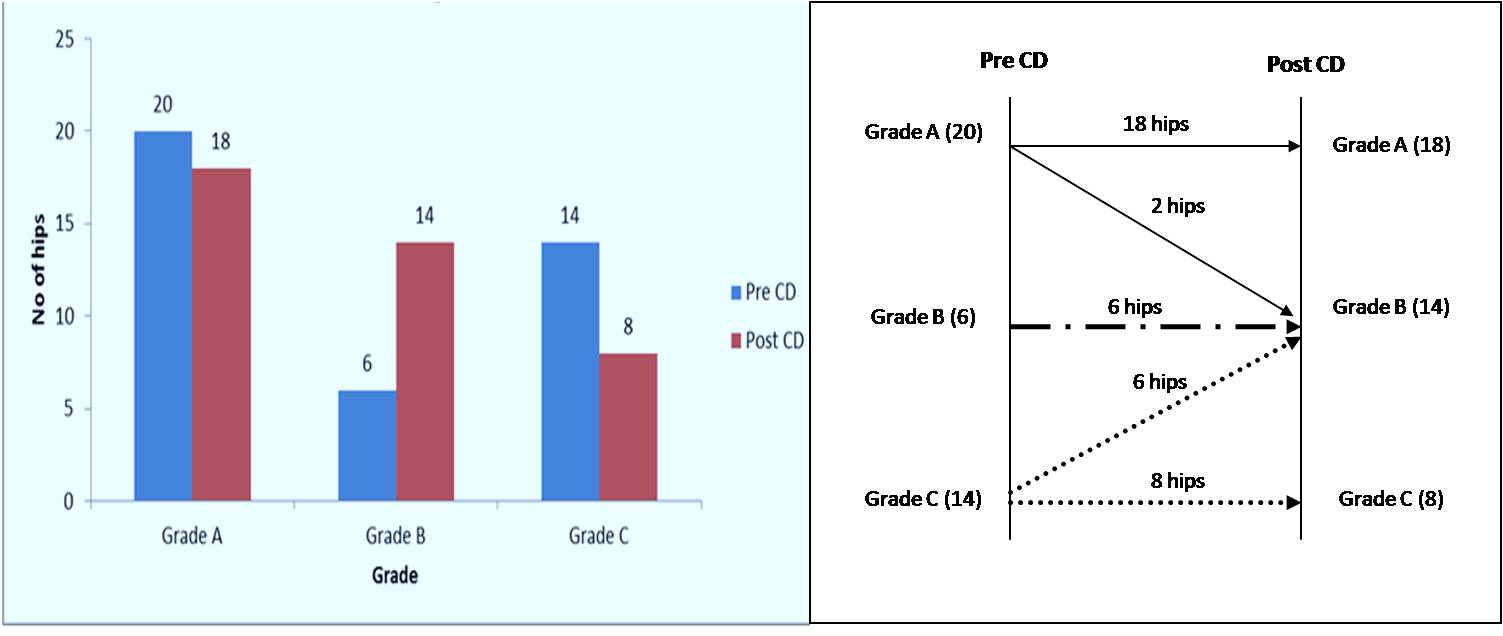
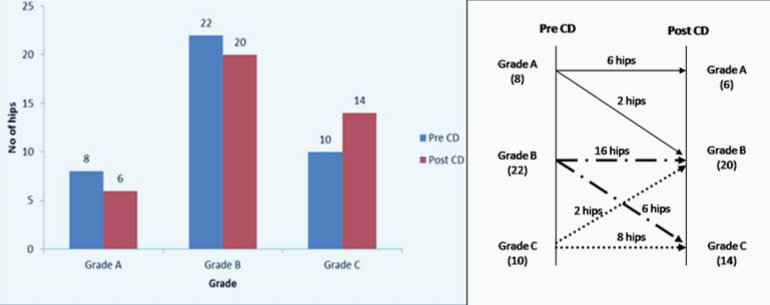
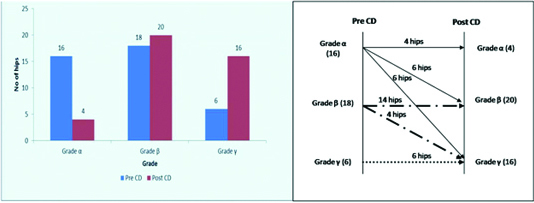
Forty hips of precollapse avascular necrosis in 24 patients were treated by core decompression during two year period. Sixty patients had bilateral avascular necrosis of the femoral head with male predominance (M:F-16:8). Maximum incidence was noted in the 31-40 years age group in the index series. The aetiology in non-traumatic AVN of the femoral head was broadly classified into 3 categories of which steroid intake was found to be most common cause (n=16), followed by idiopathic (n=6) and alcoholism (n=2) (p-value < 0.05). Pre and post procedural comparative imaging analysis was categorized into: 1) Bone marrow oedema; 2) extent of necrotic lesion; 3) Location of necrotic lesion; 4) Signal intensity of necrotic lesion; 5) Clinical outcome; 6) Predictors of poor outcome. The occurrence of bone marrow oedema was 60% (24 out of 40) in hips with osteonecrosis of the femoral head and all were placed in stage 2 (p-value<0.05). Post core decompression, there was resolution of marrow oedema in all with amelioration of pain [Table/Fig-2]. With regard to the extent [Table/Fig-3] and location of AVN [Table/Fig-4], hips with smaller lesions (90% grade A & 100% grade B) remained stable after core decompression as opposed to hips with grade C lesions where, 42.85% of hips improved and 57.14% remained stable (p<0.05). In regard to the signal intensity of AVN of femoral head, all the hips showed alteration in the signal intensity post core decompression and majority progressed to a higher grade (α—γ) irrespective of improved pain relief in short term follow-up [Table/Fig-5]. All the hips which were stable or improved after core decompression on MRI were also clinically stable and improved in short term follow up. In our study, 6 hips underwent total hip replacement between 9 to 12 months after core decompression [Table/Fig-6]. All these patients had initial pain relief after core decompression but developed sudden onset collapse between 9 and 12 months which necessitated total hip replacement. Of these 4 lesions were grade C with more than 50% of weight bearing head involvement with bone marrow oedema [Table/Fig-7].
Among 16 hips (40%) without bone marrow oedema in pre CD remained status. (p value < 0.05) Among 24 hips (60%) with bone marrow oedema in pre CD, all of them showed resolution (p value < 0.05).
Out of 20 hips (50%) of hips in grade A in Pre CD 18 hips (45%) remained as grade A and 2 hips (5%) progressed to grade B in Post CD. Among 6 hips (15%) in grade B in Pre CD all remained as grade B in Post CD. Among 14 hips (35%) of hips in grade C in Pre CD 6 hips (15%) improved to grade B and remaining 8 hips (20%) remained grade C.
Among 8 hips (20%) in grade A in Pre CD, 6 hips remained as grade A and 2 hips progressed to grade B. Among 22 hips (55%) in grade B in Pre CD, 16 hips remained as grade B and 6 hips progressed to grade C. Among 10 hips (25%) in grade C in Pre CD, 8 hips remained as grade C and 2 hips progressed to grade B.
Among 16 hips (40%) which were in α in pre CD, 6 hips progressed to β and 6 hips progressed to γ, while 4 hips remained status. (p value < 0.05).
Clinical outcome: Initial clinical improvement was seen in all patients, HHS improved from 57 to 80. 6 hips had a fall in Harris hip score to mean value of 34.1 during follow up (9 to 12 months) and underwent THR.
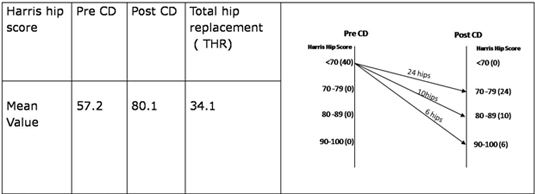
Imaging characteristics of 6 hips who underwent THR in long term follow up (9-12 months) :4 hips had extent of osteonecrosis grade C and 2 hips had extent of osteonecrosis grade A, where the location was grade C. The other 4 hips had a location of grade C and grade B i.e more than 1/3rd of involvement. Signal intensity of 3 hips who underwent THR is α for4 hips and β for 2 hips. All the 6 hips showed bone marrow oedema.
Discussion
There is scarcity of literature on follow up of core decompression using MRI studies in our Indian population. The present study is intended to analyse the MRI changes following core decompression and to identify the MR criteria associated with successful outcome. To our knowledge, this is the first study in Indian patients evaluating the MR appearance after core decompression and correlating with clinical outcome.
Early diagnosis and treatment of avascular necrosis is crucial because it affects relatively young individuals and treatment options for advanced disease are limited [1,2]. Total hip replacement has been proven to be a standard modality of treatment after collapse [3]. However, because of young age of many of these patients, a hip replacement cannot be expected to last patient’s life time and therefore when feasible attempts should be made to save the femoral head prior to collapse. The results in present study are similar to previously reported studies in terms of risk factors, age, male predominance and bilateral involvement [1–3]. Corticosteroid treatment, chronic alcoholism and hypertriglyceridemia favoured male predominance in the present study. Ficat RP theorized that AVN is a compartment syndrome caused by increased intramedullary pressure and venous stasis [5]. These observations led to the use of core decompression to reduce the intramedullary pressure and halt the natural progression of the disease which leads to disabling arthritis requiring joint replacement. Although, spontaneous regression has been reported [8], it is very uncommon. Core decompression is effective surgical treatment for early stage avascular necrosis [1–3] with success rates ranging between 60%-80% at the time of short term and midterm follow-up [9]. This wide range of success rates of core decompression is attributed to differences among studies with regard to selection of patients (i.e., differences in patient diagnoses), classification systems, operative procedures, postoperative management, and evaluation of clinical outcome [10]. The detection of avascular necrosis particularly in its early stages is imperative to give therapeutic intervention the best opportunity for successful management. MRI has emerged as the modality of choice for evaluation of avascular necrosis of bone. Magnetic resonance imaging can detect and characterize osteonecrotic segments of the femoral head before such abnormalities are evident on plain radiography, scintigraphy, or computerized tomography [1,2,4].
MRI can also be used to plan and monitor the treatment of the affected hip and may even be able to predict patient’s response to therapy [1]. The ideal timing of MRI after core decompression remains unclear. However, most of the available studies suggest that changes can continue up to 6 months after the surgery [6]. In order to evaluate all possible changes minimum time of 6 months after CD was chosen for the follow up scans. The specific imaging parameters on MRI and radiographs can be analysed with any major classification system as systematic analysis of Classification Systems for Osteonecrosis of the femoral head by Mont A et al., revealed similarities between various classifications systems used for avascular necrosis of the femoral head [11].
In the present study, all the MRI scans are analysed according to Shimizu K et al., for extent [6], location and signal intensity of avascular necrosis of femoral head and for presence of single line/single line and bone marrow oedema on T1 W sequence according to Radke S et al., [1].
Very few studies have correlated the MR changes after core decompression with either positive or negative clinical outcome [1,6,9].
Shimizu K et al., evaluated 66 hips with avascular necrosis using MRI and found that extent of necrosis of the femoral head, location and intensity of signal are useful predictors of the probability of collapse [6]. Aigner N et al., evaluated 45 patients using MRI controlled study of core decompression with early avascular necrosis and found that most lesions that appeared stable on post core decompression MRI also had good clinical outcome [9]. The findings of the present study are consistent with those reported by Aigner et al. The therapeutic success of core decompression is determined by bone marrow oedema and it is important to differentiate on MRI between a double line sign plus bone marrow oedema and a double line sign only [1].
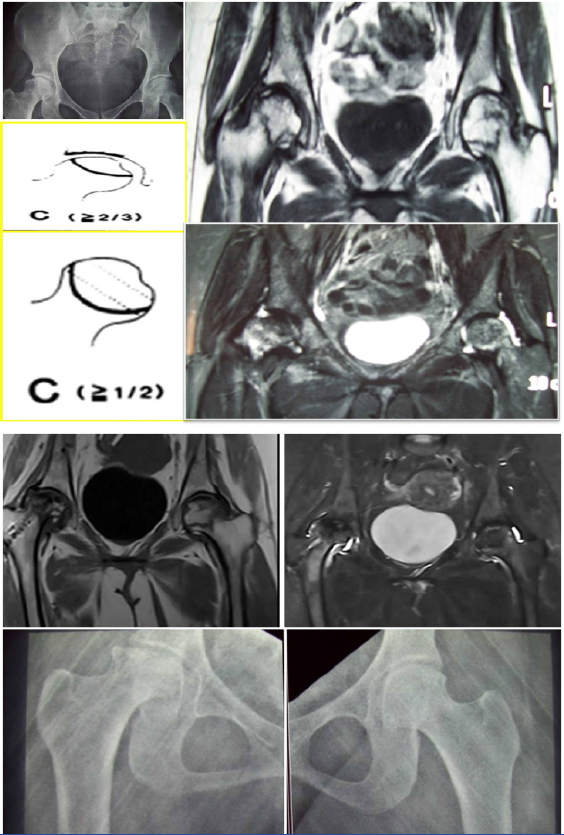
The results of the present study indicate that both extent and location of AVN of femoral head are the important predictors that determine the short term outcome of CD in femoral head. All the hips which were stable or improved after CD on MRI were also clinically stable and improved in short term follow up [Table/Fig-8a–8d]. All the hips showed alteration in the signal intensity after post CD and majority progressed to a higher grade (α—γ) irrespective of improved pain relief in short term follow up similar to a previously reported study [5,6].
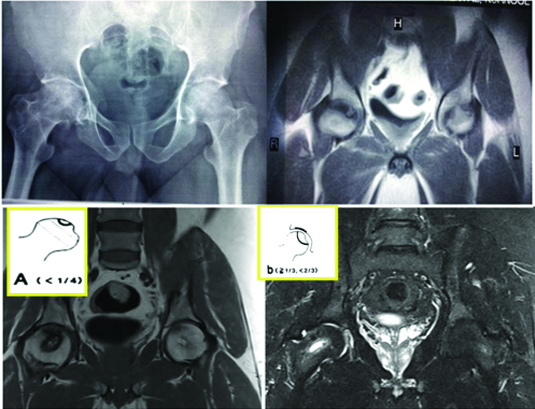
Pre CD – X ray (A) shows stage 2 AVN of right hip and stage 1 AVN of left hip. Pre CD T1 weighted MRI (B)– Right side Lesion extent is grade A location is grade B and signal intensity is grade β. Left side Lesion extent is grade A location is grade A and signal intensity is grade α. There is no evidence of bone marrow oedema.
Post CD- T1 weighted (C) and STIR MRI (D) – Right side Lesion extent is grade A location is grade C signal intensity is grade γ. Left side lesion extent is grade A location is B signal intensity is grade α.
In our study, the occurrence of bone marrow oedema was 60% in hips with avascular necrosis of the femoral head. Our figure is similar to those previously reported by other investigators, which have ranged from 30% to 50% [1,6,12].
The cause of pain in patients with avascular necrosis of the femoral head is not well understood. Relief of pain after core decompression in patients with early avascular necrosis of the femoral head is a well-documented observation [1,8]. Koo et al., reported that the pain in all eight hips of their patients subsided with ameliorating of bone marrow oedema and intramedullary hypertension after core decompression [12]. In a study by Wirtz C et al., [13], the transient bone oedema showed normal signal pattern at an average of 3 months and in stage 1 and 2, all patients with a preoperative necrosis area of less than 30% of the femoral head showed reduction of the necrotic zone and good clinical results. In our study, post core decompression, there was resolution in the bone marrow oedema in all cases with lesion stability in smaller lesions grade A extent and location [Table/Fig-9a-9f].
(A-C) Pre CD Radiograph (A)shows stage 2 AVN of right hip. Pre CD T1 weighted(B) and STIR (C) MRI shows grade A lesion extent, grade C location and grade α signal intensity. There is bone marrow oedema on STIR.
(D-F) : Post CD Radiograph shows no collapse of femoral head.T1 weighted (E) and STIR MRI (F) shows grade A lesion extent, grade C location and grade γ signal intensity. There is no bone marrow oedema on STIR.
Iida et al., observed that bone marrow oedema correlated highly with hips that progressed to collapse of the femoral head [14].
In our study 6 hips underwent THR between 9 to 12 months after core decompression. All these patients had initial pain relief after core decompression but developed sudden onset collapse between 9 and 12 months which necessitated THR. Of these 4 lesions were grade C with more than 50% of weight bearing head involvement with bone marrow oedema [Table/Fig-10a-10f]. The results of the present study also suggest that bone marrow oedema in the presence of type C involvement of weight bearing head indicate a poor outcome after core decompression with progression to head collapse and are in agreement with results of Beltran J et al., who conducted long term follow up on 34 hips who underwent core decompression of the femoral head for AVN and concluded that MR quantification of the extent of femoral head involvement in AVN predicts collapse shortly after core decompression, so that core decompression can be avoided in patients at risk [15]. More studies with larger number of patients with MR follow up are required to predict the successful outcome of core decompression.
(A-C) Pre CD Radiograph (A) showing bilateral stage 2 AVN. Pre CD T1 weighted (B) and STIR MRI (C) – Right side Lesion extent is grade C location is grade C and signal intensity is grade α. Left side Lesion extent is grade C location is grade B and signal intensity is grade α. There is bone marrow oedema on right side, LD(Line diagram) showing the location and extent).
(D-F) : Post CD Radiograph (A) showing collapse on right side. Post CD T1 weighted (E)and STIR (F) MRI – Right side Lesion extent is grade C location is grade C and signal intensity is grade γ. Left side Lesion extent is grade C location is grade B and signal intensity is grade α. There is no bone marrow oedema on right side.
Conclusion
Core decompression has good outcomes in Grade A and B lesions. However, Grade C lesions with more than 50% involvement of femoral head had higher chance of collapse after core decompression despite pain relief in the short term. All hips showed resolution of bone marrow oedema (BME) post core decompression and this predicts postoperative pain relief. BME is a predictor of higher grade of AVN and also impending collapse when associated with higher grade in extent or location (GRADE C). In majority of cases, progression to higher grade signal could not be altered with core decompression. Grade C involvement in extent, location with concomitant bone marrow oedema is an important predictor of collapse in long term follow up.