Diagnosis of the onset of facial paralysis may be made by various specialists, neurologists, physiatrists, internists, infectious disease specialists, otolaryngologists, and ophthalmologists, in addition to emergency doctors. Evaluating the pathology requires specific experience, both for the identification of symptoms and to address the functional damage created immediately and that which could arise from possible future complications.
A functional nerve deficit is evinced by the alteration of both static and dynamic facial expressions. For several years, numerous assessment scales have been proposed and researched for the quantitative and qualitative determination of this deficit [1–4].
The House-Brackmann (HB) scale, known today by the Facial Nerve Grading System (FNGS) acronym, is the scale most used internationally [5,6]. Published by two authors in 1985, the method is still the most well-known by all specialists dealing in facial paralysis. Other highly valued methods include: the Sydney scale, based on the branches of the facial nerve; the Sunnybrook scale, based on a few facial expression movements; and the Yanagihara this is a regional scale. There are also assessment systems based on facial muscle testing, the Frey’s classification, or linear measurement techniques such as the Burres lines or the Nottingham system [7].
Materials and Methods
This prospective study was conducted at the Center for Facial Nerve Disorders of the San Camillo Hospital in Rome. Sixty individuals affected by facial paralysis were examined with our system. The patients were assessed at the onset of pathology (T-0) and at 3 (T-3) and 6 (T-6) months after onset.
The 60 patients considered for our study all had Bell’s palsy, and were selected to make the case studies as homogenous as possible.
Three specialists were involved in the study, all aware of our method of assessment an otolaryngologist, an internist and a facial plastic surgeon. These three specialists were aware of the most common methods used in Italy to evaluate the facial palsy: the House-Brackmann Scale and the May assessment.
All three specialists performed assessments on the patients at T0, T3, and T6.
The selection of the three specialists was made based on their individual experience in the treatment of facial nerve disorders.
No training for the use of the Arianne Disease Scale (ADS) scale was provided.
ADS (Our Assessment System)
Our system divides the face into three areas: upper, middle, and lower [Table/Fig-1]. The assessment evaluates the muscle tone at rest (static), during movement (dynamic), and syncinetic.
Muscle area subdivision according to the A.D.S. scale.
Legend figure face:
(1) Frontalis medial portion; (2) Frontalis lateral portion; (3) Procerus; (4) Depressor supracilii; (5) Levator labii superioris alaeque nasi; (6) Zigomaticus minor et major;
(7) Orbicularis oculi: pre tarsal portion; (8) Orbicularis oculi:pre septal portion;
(9) Orbicularis oculi: orbital portion; (10) Compressor nasi; (11) Dilator nasi;
(12) Depressor septi; (13) Orbicularis oris; (14) Depressor anguli oris;
(15) Depressor labii; (16) Mentalis; (17) Platysma; (18) Corrugator; (19) Risorius
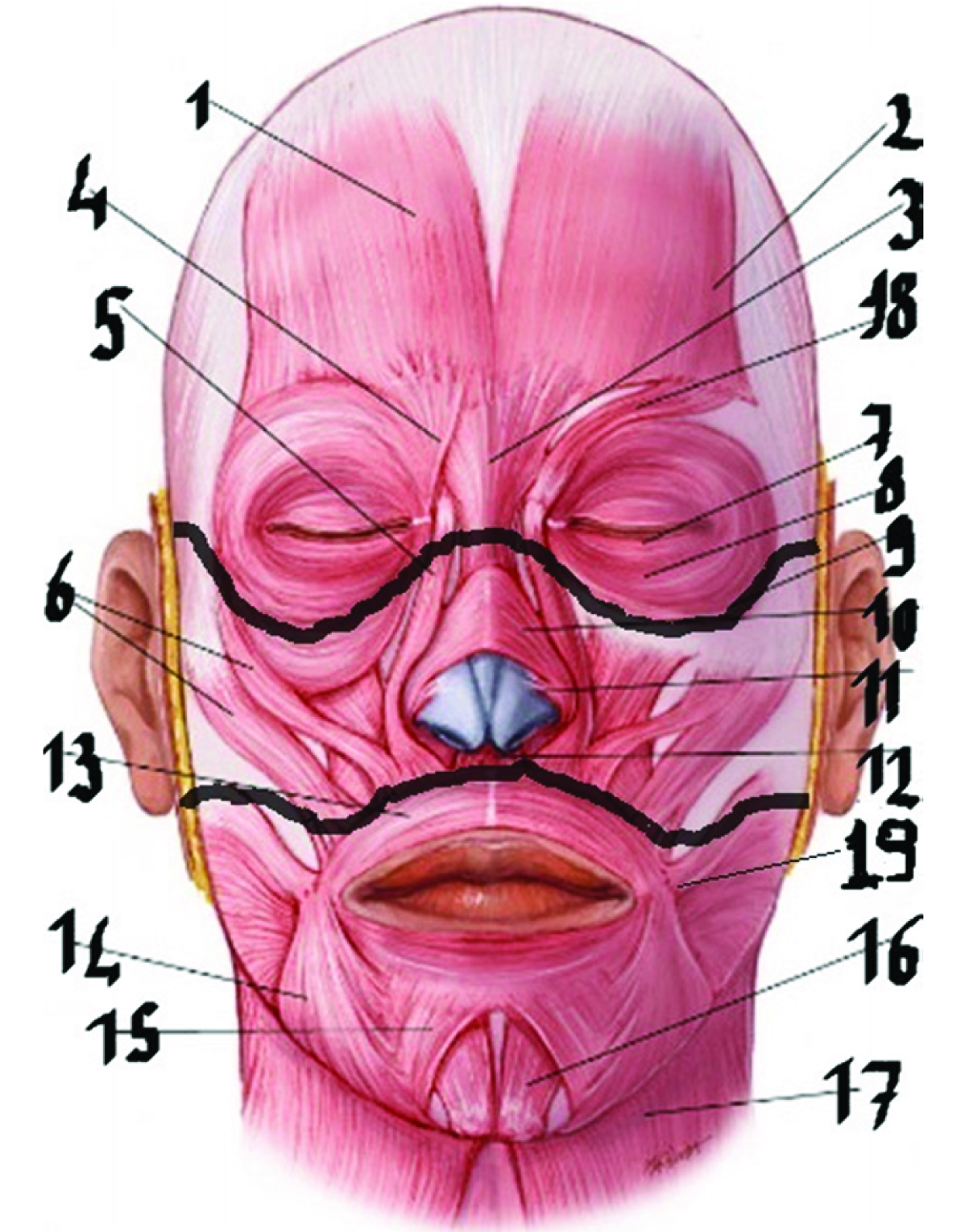
Each area is then assessed for the functional capacity of individual muscles in performing specific movements:
Raising the forehead = frontal muscle; Corrugate = corrugator muscle; Closed eyes with or without effort = orbicular muscle of the eye; Corrugate nose = elevator muscle of the nose, and orbicular muscle of the mouth; Smile = orbicular muscle, risorius muscle, zygomatic, chin, and platysma muscles; Kiss = orbicular and chin muscles; Lower lip = chin muscle; and Stretch the neck = platysma muscle.
Each facial area (upper, middle, and lower) was then subdivided into muscle units considering facial expressions. The muscle capacity was expressed numerically with a grading system from 0 to 1 for each muscle, for a total ranging from 0 to 4 for each area. Grading system 0 to 1 is the system used for each single face district (upper, middle and lower face), when considering the muscle evaluated for each area we can obtain an “area result” linked to the number of muscles. For example, in middle face we considered two muscles only if each muscle had a ranging value from 0 to 1, in case of partial recovery of zygomatic muscle (0.3) and a total recovery of alar nose elevator (1) the results will be 1.3. Considering low district with 4 muscles, if total mobility was recovered by all muscles (1), we will have 4 like score facial area.
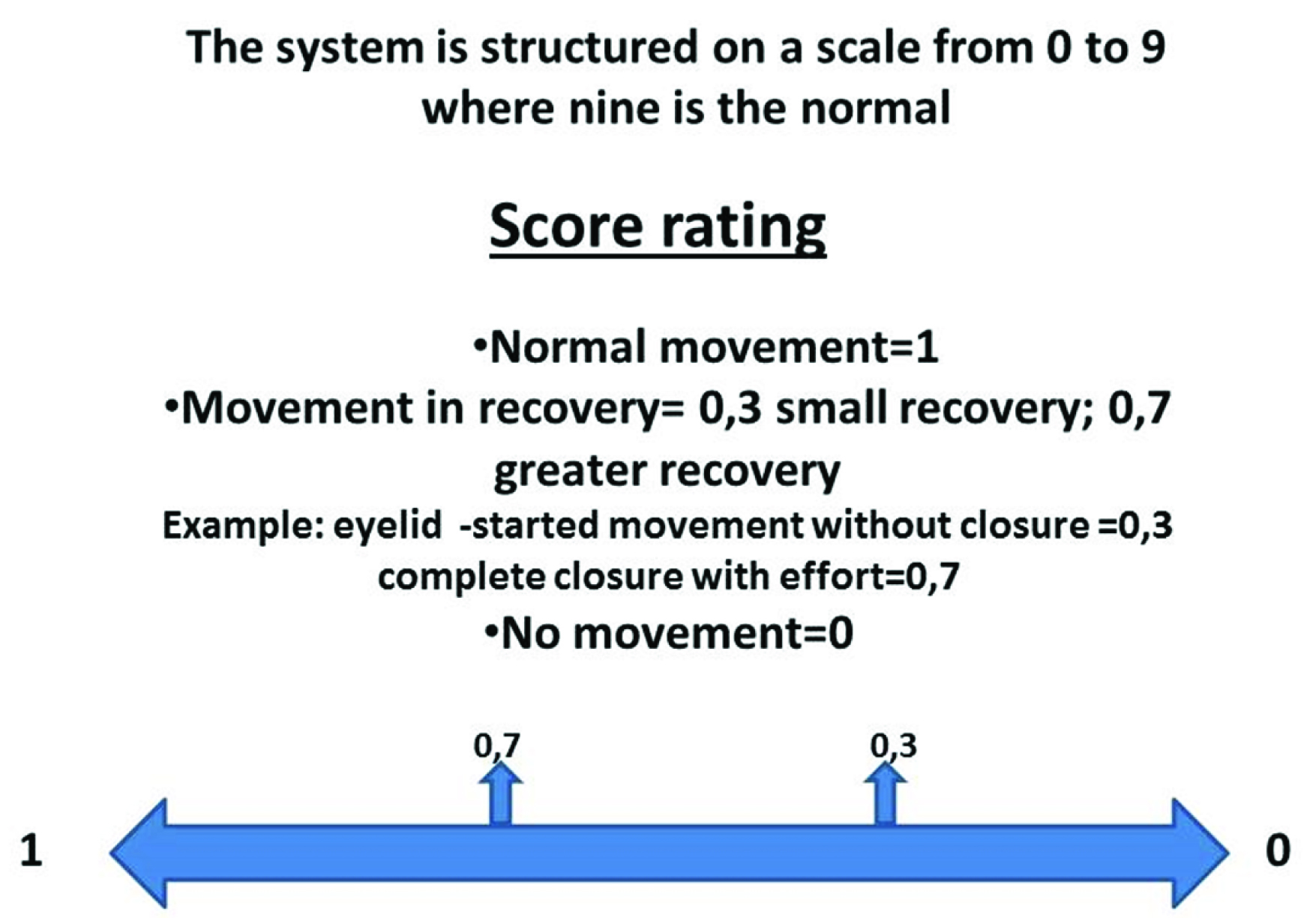
A score of 0 equals the absence of movement, 0.3 equals a small recovery (upper eyelids mobile with effort but cannot be closed), 0.7 equals a major recovery (eyelids can be closed with effort), and 1 equals normal movement (eyelids can be closed without effort) [Table/Fig-2].
Numbering system in the ADS scale
Upper: frontal, corrugator, orbicular eye.
Middle: alar elevator muscle of the nose, zygomatic.
Lower: orbicular muscle of the mouth, risorius, chin muscle, platysma (we didn’t consider buccinator muscle because it has not involved in the smile).
From the sums of the various numbers, we obtained scores ranging from 0 to 4. In areas with two muscles, a maximum of 2 points could be obtained (middle face); in areas with three muscles, a maximum of 3 points could be obtained (upper face); and in those with four, a maximum of 4 points could be obtained (lower face). The sum of all points for each sector could result in a maximum score of 9, that is, the full-face assessment.
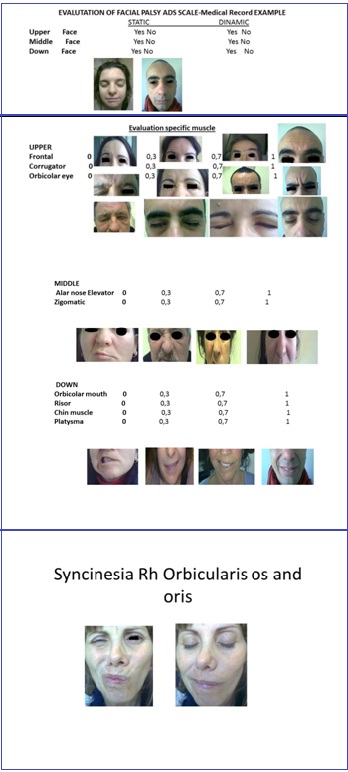
The appearance of syncinesis reduced the points by 0.5 for each small muscle involved. For the assessment of syncinesis, patients were asked to smile, make their lips protrude, and close their eyes, so that we could identify the pairing of movement between the orbicular muscle of the eye and of the mouth, or between other muscles.
The total score for the full evaluation of the face was between 0 and 9, where 0 equals the absence of movement and 9 equals normal movement [Table/Fig-3].
ADS scale clinical data recovery
| Evaluation of Facial Palsy ADS Scale-Medical Record |
|---|
| Static | Dynamic |
|---|
| Upper face | Yes | No | Yes | No |
| Middle face | Yes | No | Yes | No |
| Down face | Yes | No | Yes | No |
| Evaluation specific muscle |
| Upper | | | | |
| Frontal | 0 | 0, 3 | 0, 7 | 1 |
| Corrugator | 0 | 0, 3 | 0, 7 | 1 |
| Orbicolar eye | 0 | 0, 3 | 0, 7 | 1 |
| Middle | | | | |
| Alar nose elevator | 0 | 0, 3 | 0, 7 | 1 |
| Zigomatic | 0 | 0, 3 | 0, 7 | 1 |
| Down | | | | |
| Orbicolar mouth | 0 | 0, 3 | 0, 7 | 1 |
| Risor | 0 | 0, 3 | 0, 7 | 1 |
| Chin muscle | 0 | 0, 3 | 0, 7 | 1 |
| Platysma | 0 | 0, 3 | 0, 7 | 1 |
Based on the author’s personal experience, the assessment time expected for each patient, using our scale is 30 sec.
Results
Our results considered 60 patients, 57% were females and 43% were male, with ages ranging from 8 years to 75 years (average, 53 years of age).
The results took into consideration:
(1) The time necessary for patient assessment and ease of use of the selected scale;
(2) The precision of the assessment of each individual functional deficit;
The average time for the specific assessment of each muscle deficit was 1 min and 35s - 1 min for the most convenient and 2 min for the least convenient. The general assessment was made by all three specialists in 25s, this data is less than the expected author’s time of 30s.
Relative to the precision of muscle area assessment at the highest degree of deficit (0 and 1), there was conformity of assessment that was comparable for all three specialists (100%), with the discrepancies mainly in the scores 0.3 and 0.7. The discrepancies in these scores were evident in all three stages of assessment (T0, T3, T6) and were not perfect agreement between evaluators. In fact, the three evaluators’ assessments concurred in only 92% of upper area cases examined, in 87% of middle area cases, and in 80% at the lower level.
We noted that intermediate scores 0.3 and 0.7 became difficult to define in areas where the movement involved more muscles at the same time. During a smile, for example risorius action was difficult to identify and understand, except in the case of a careful analysis.
Frontal and Corrugator muscles were easier to evaluate even with the intermediate scoring. Frontal and corrugator movements were easily understood observing the position of the eyebrow.
Although the zygomatic muscle has a big effect in cheekbone definition, understanding the score 0.3 or 0.7 tied to the movement of the movement of the zygomatic muscle was very difficult to evaluate when a patient smiled. Examples can be seen in [Table/Fig-4a-c].
Discussion
Since 1985, many authors have discussed the House-Brackmann scale [1] and its limitations [2]. Other methods of assessment have been proposed in attempts at improved accuracy [3]. Recently, changes were made to the House-Brackmann scale to make it more accurate [4,5].
The House-Brackmann scale is not specific for facial areas. It considers predominantly the functionality of the eyes, but not the specific muscle deficit. The motility of the mouth is assessed by a single expression, but the greater problem results from the assessment of synkinesis. As Charachon, Bebear, Sterks and Magnan showed synkinesis is the effect of a post-damage abnormal recovery of the facial nerve [4]. In the House-Brackmann scale, this occurs at the lowest levels (the best recovery), which may lead to consideration of synkinesis as an onset symptom of paralysis.
The modified Brackmann scale (FNGS2), proposed by the Commission for Facial Nerve Disorders [5,6], considers both the facial areas and synkinesis. The limitations, in this case, are illustrated by the percentage expression of the deficit area and by the fact that the grading for the consideration of synkinesis makes the assessment extremely complex.
There are methods based on video recordings, even computerized, that have been used to assess facial motility, but they were two-dimensional and were limited by the presence of wrinkles that could mask real deficits [2].
The ‘gold standards’ of our study were, most importantly, the real-life analysis of patients, the ease of completing the assessment as shown by the results, and the fact that no examiner training was needed. It was an expedient method not only for the initial completion of assessment in 25 s (as rapid as that needed by the H.B. scale), but also for specific motility (1 min and 35 s) – much faster than the original H.B. scale.
Although, in the assessment of the specific areas, no complete correlation was found (100%) among the three investigators, and, for the intermediate scores, the agreement percentage was reduced from the upper (92%) and middle (87%) areas to the lower area (80%), we determined that a general correlation, based on a full-face total of 86% (85,6666%). The 86% value was based on statistic media between the three scores for each district (upper 92%, middle 87% and lower 80%)
Syncinesis, assessed by subtracting 0.5 from the muscle area of interest, is easy to interpret. Even for someone who is inexperienced, it is sufficient to know the anatomy and physiology of facial movement.
Our assessment method includes a series of points from the various scales something from the House-Brackmann, something from the Sydney, and something from the Sunnybrook [7–9] which we have simplified by reducing the numerical values and increasing the specificity involving the individual muscle areas. In this manner, we were able to obtain greater functional deficit nuances, thereby obtaining a simple but detailed scale.
Currently, ours is an assessment scale that precisely identifies the deficient muscles and is undoubtedly also a valid aid in surgical rehabilitation. Identifying damage to the orbicular instead of the risorious muscle may allow the surgeon to develop a specific technique so that the patient can recover movement [10].
We identified a few limitations in our study. A small number of patients were involved in the study. Having validated the scale a larger cohort of patients can be studied. Several difficulties were found also in the accuracy of deficit in the evaluation of some muscles. Risorius and Zygomatic muscles can be evaluated only at maximum score no movement (0) or normal movement (1), but difficult to understand the correct way to calculate the intermediate score like 0.3 and 0.7; this limit could be explained by muscle’s functions. Risorius and zygomatic are muscles active in smiling, their action is synergic with other muscles, so is very complicated understand these small score’s variation during the movement. Eyelid and mouth’s orbicular muscles have some analysable points able to help in understanding the intermediate score: eyelid’s distance in closure, position of mouth’s angle during smiling.
Finally we did not assess the function of the buccinators muscle as we choose to evaluate only the muscles considered in established scales including ABC. This choice was born in function of the scientific community’s habits. The author believes that including a new muscle could make the assessment more difficult to understand and/or compare.
Conclusion
Among the various scales proposed, that described in our study appears to have valid points: it examines all the facial muscle areas and, indirectly, the functionality of the main branches of the facial nerves. It is an expedient system, both for the initial implementation with the patient and for a more specific analysis of individual deficits. It takes syncinesis into consideration as a complication of damage. It is easy to use and does not require much operator experience.
We believe that it will be necessary to conduct another study with more subjects involved and to create a medical record with standardized pictures to limit the mistakes tied to the evaluation of intermediate score 0.3 and 0.7. The author has determined that this simple clinical scale could be a valid alternative to existing scales, since it includes points from different methods, and, most importantly, for its capacity to identify nuances that currently can be obtained only with more complex assessment methods.