Nasal Septal Angiofibroma in a Post-Menopausal Woman: A Rare Entity
Sandie Ewe1, Farah Dayana2, Fazalina Mohd Fadzilah3, Balwant Singh Gendeh4
1 Resident, Department of Otorhinolaryngology, Head and Neck Surgery, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Kuala Lumpur, Malaysia.
2 Specialist, Department of Otorhinolaryngology, Head and Neck Surgery, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Kuala Lumpur, Malaysia.
3 Specialist, Department of Radiology, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Kuala Lumpur, Malaysia.
4 Professor, Department of Otorhinolaryngology, Head and Neck Surgery, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Kuala Lumpur, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sandie Ewe, Resident, Universiti Kebangsaan Malaysia Medical Centre (UKMMC), Jalan Yaacob Latiff, Kuala Lumpur, Malaysia
E-mail: drsandie@gmail.com
Juvenile angiofibromas (JAs) are well-characterised in literature, arising typically in the posterolateral wall of the nasal cavity of young males. Numerous theories have been proposed to explain the occurrence of this unique and rare tumour. Angiofibromas originating in other sites within the head and neck have been described but this is exceedingly rare, constituting less than 2% of all diagnosed cases. Extranasopharyngeal angiofibroma is a rare lesion, and more importantly, controversial. It is not known whether it is actually a relative of the well-known JA that is seen exclusively in adolescent males. We present the case of a post-menopausal woman with unilateral nasal obstruction who was unexpectedly diagnosed as nasal septal angiofibroma.
Angiofibroma, Extranasopharyngeal angiofibroma, Nasal septum, Post-menopause
Case Report
A 67-year-old lady presented to the Otorhinolaryngology clinic with complaints of right nasal obstruction for the past 6 months. She had no symptoms of persistent rhinorrhoea, recurrent epistaxis, anosmia, facial pain, facial numbness, headache, epiphora and diplopia. She had neither accompanying ear or throat symptoms nor preceding history of trauma or infection. She was a non-smoker, with no known occupational exposure risk factors. Endoscopic examination revealed a firm, smooth surface lobulated red mass arising from the right anterosuperior septum impinging on the inferior turbinate. The left nasal cavity looked normal. The nasopharynx, oropharynx and larynx were otherwise normal. There were no palpable cervical lymph nodes. Our initial working diagnosis was pyogenic granuloma, septal turbinate or nasal lymphoma. We proceeded with an office biopsy of the mass to rule out malignancy.
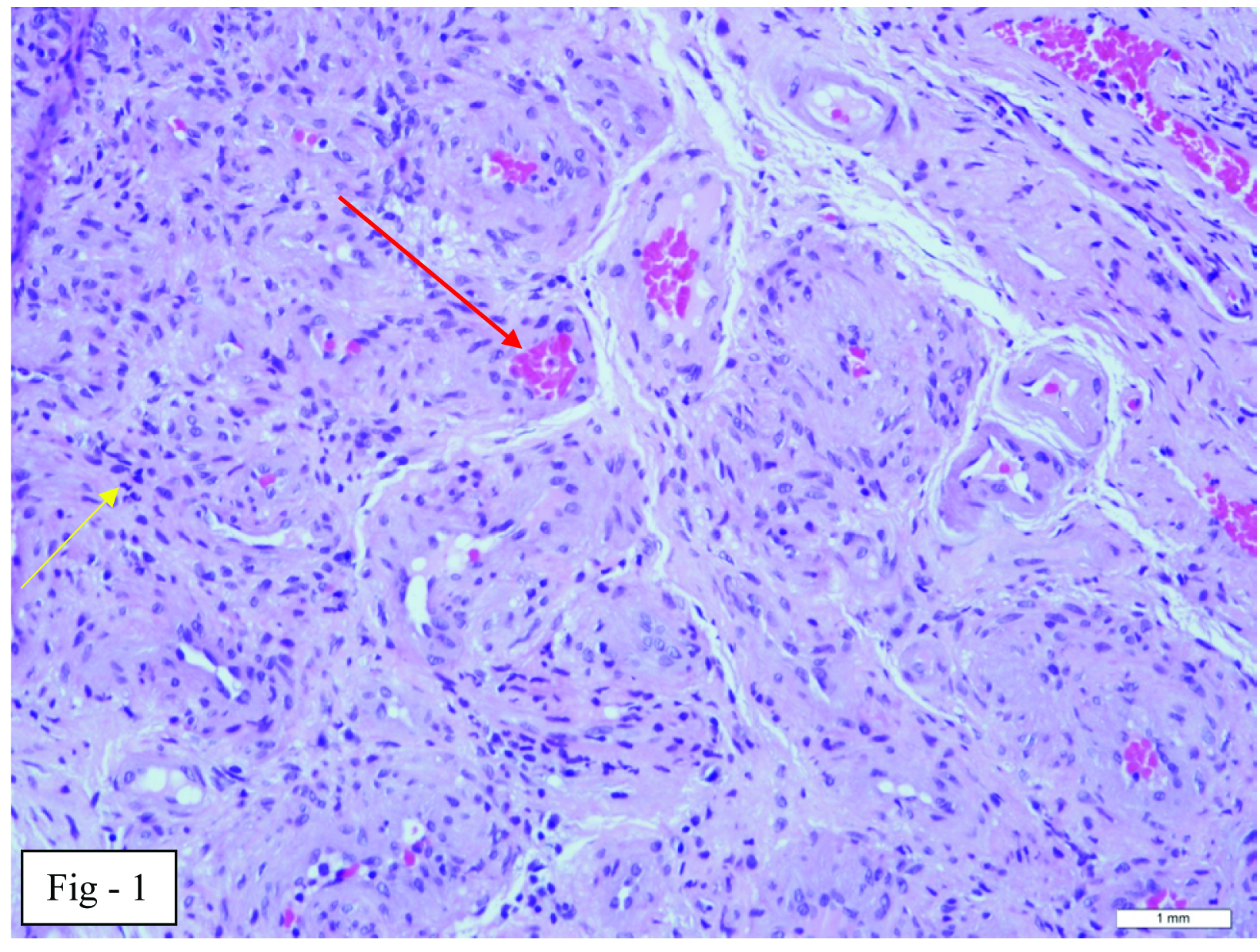
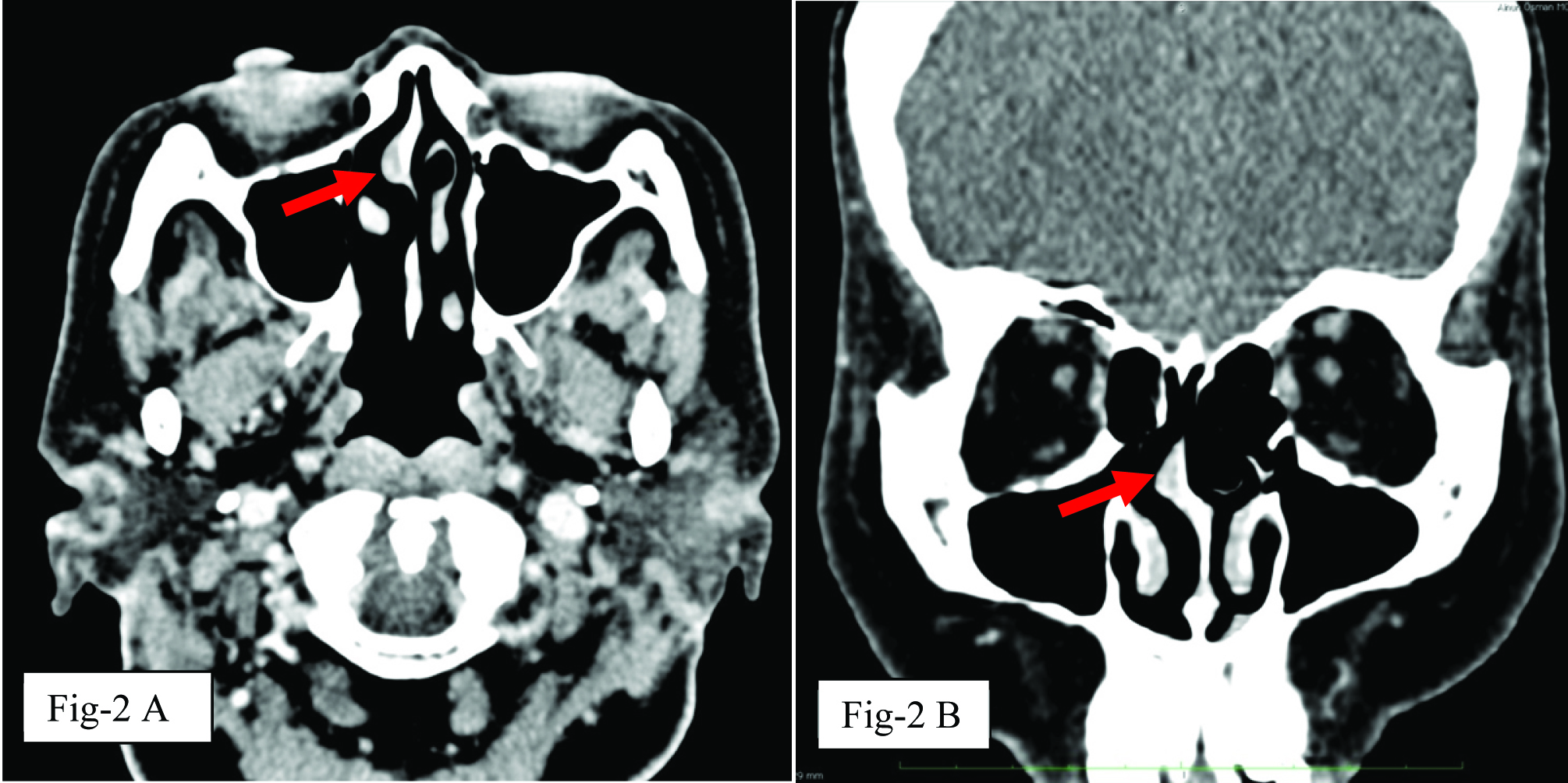
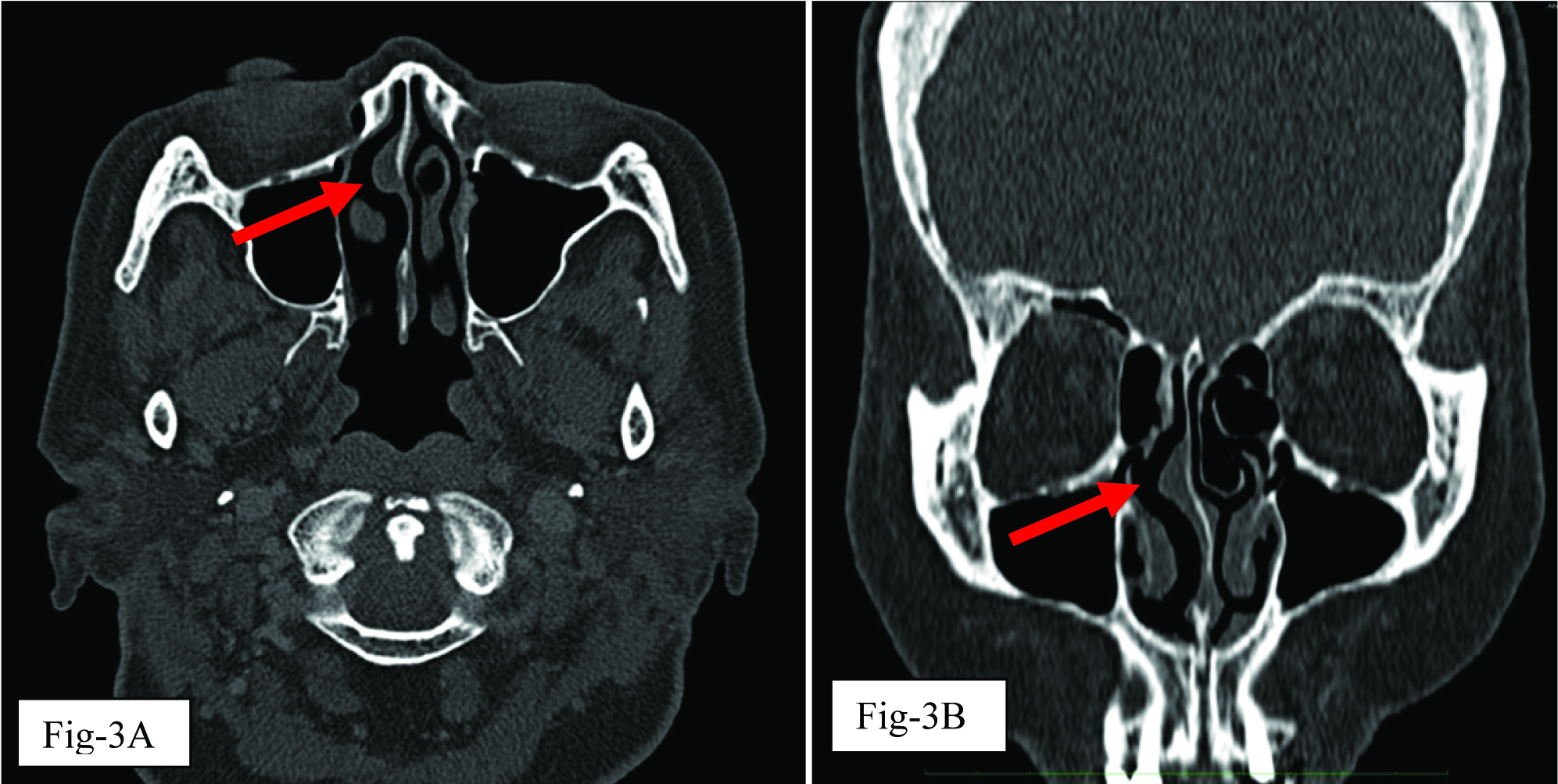
Biopsy of the mass resulted in minimal bleeding and haemostasis was secured. Proliferation of thin-walled vessels in dense fibrous stroma was seen in the biopsy specimen, and histologically the mass was diagnosed as an angiofibroma [Table/Fig-1]. A computerized tomography (CT) scan with contrast revealed a localised well-defined small mildly enhancing soft tissue lesion measuring 0.8cm by 0.4cm by 0.8cm, confined to the right anterosuperior septum with mild deviation of the nasal septum to the right. The soft tissue mass appeared to be localised over the right perpendicular plate of ethmoid portion of the septum, just inferior to the cribriform plate of ethmoid [Table/Fig-2]. There was no radiological evidence of bony erosion or extension to the paranasal sinuses [Table/Fig-3]. The patient was offered the option of endoscopic resection of the mass but patient refused. One-year follow up demonstrated no evidence of change in the septal mass.
Photomicrograph showing proliferation of vessels (red arrow) in fibrous stoma (yellow arrow) which were consistent with angiofibroma (H&E, 40X)
CT scan of the paranasal region in soft tissue window showing a localised well-defined mass (red arrow) with some nodular enhancement arising from nasal septum and no associated bony erosion. (A: axial view; B: coronal view)
CT scan of the paranasal area in bone setting showing a localised well-defined mass (red arrow) with some nodular enhancement arising from nasal septum and no associated bony erosion (A:axial view; B:coronal view).
Discussion
Juvenile angiofibromas (JA) are well-characterised in literature; classically presenting with the triad of unilateral nasal obstruction, epistaxis and a nasopharyngeal mass. JA is seen in young males, between the ages of 6 and 26 years [1]. Its site of origin is typically in the posterolateral wall of the nasal cavity, near the superior margin of the sphenopalatine foramen. Numerous theories have been proposed to explain this predilection. Tillaux speculated that angiofibromas originate in the tissue of the anterior margin of the atlas at the lower surface of the sphenoid bone, which was referred to as fibrocartillagenous barriers [2]. These tissue were termed as ‘fascia basalis’ by Brunner because it contained no cartilage [2].
Angiofibromas have also been reported in other unusual sites such as the maxillary sinus, nasal septum, middle turbinate and inferior turbinate [3]. Angiofibromas of the nasal septum is extremely unusual, and to date only 16 nasal septal angiofibromas have been reported in English literature [Table/Fig-4] [1,2,4–15]. The nasal septum is almost devoid of ‘fascia basalis’ except in the posterior part of the vomer and the ethmoid bone [2]. Site of origin of nasal septal angiofibromas (NSAs) previously described includes the anterior 1/3 of septum (cartilagenous septum), bony cartilaginous junction, as well as perpendicular plate of ethmoid [1–15]. This varied site of origin within the nasal septum suggests the possibility of the tumour arising from ectopic tissue due to migration error during development of the nasal septum [2].
Reported NSAs in literature
| Authors | No of cases | Site of origin | Symptoms | Age (years) | Sex |
|---|
| Hiraide and Matsubara, 1984 [4] | 1 | Nasal septum | Epistaxis, nasal obstruction | 13 | Male |
| Sarpa and Novelly, 1989 [5] | 1 | Bony cartilagenous junction | Epistaxis, nasal obstruction | 9 | Male |
| Handa et al., 2001 [6] | 1 | Bony cartilagenous junction | Epistaxis, nasal obstruction | 8 | Male |
| Akbas and Anadolu, 2003 [2] | 2 | Nasal septum | Epistaxis, nasal obstruction | 34, 50 | Female, Female |
| Somdas et al., 2005 [7] | 1 | Bony cartilagenous junction | Epistaxis, nasal obstruction | 27 | Male |
| Castillo et al., 2006 [8] | 1 | Anterior nasal septum | Epistaxis, nasal obstruction | 9 | Male |
| Tasca and Compradetti, 2008 [9] | 1 | Posterior nasal septum | Nasal obstruction | 57 | Female |
| Uyar et al., 2009 [10] | 1 | Anterior nasal septum | Epistaxis, nasal obstruction | 19 | Male |
| Mohindra et al., 2009 [11] | 1 | Anteroinferior end of cartilaginous septum | Epistaxis, nasal obstruction | 22 | Male |
| Garcia-Rodriguez et al., 2012 [1] | 2 | Anterior nasal septum | Patient 1: EpistaxisPatient 2: Nasal obstruction | 60, 56 | Male, Male |
| Hamdan et al., 2012 [12] | 1 | Anterior nasal septum | Epistaxis, nasal obstruction | 19 | Male |
| Correia et al., 2013 [13] | 1 | Posterior nasal septum | Nasal obstruction | 10 | Male |
| Atmaca et al., 2013 [14] | 1 | Posterior nasal septum | Epistaxis | 37 | Male |
| Dogan et al., 2013 [15] | 1 | Anterior nasal septum | Nasal obstruction | 16 | Male |
We performed a Pubmed search using the keywords “extranasopharyngeal angiofibroma” and reviewed the case presentations of angiofibroma arising from the nasal septum. Only 75% of the patients (12 out of 16 patients) presented with recurrent epistaxis. On histopathological examination, angiofibroma is described as a non-encapsulated tumour consisting of both vascular and fibroblastic components. Microscopically, the presence of numerous large stag-horn vessels within its fibroblastic stroma due to lack of a complete muscular layer in the blood vessels results in catastrophic hemorrhage on manipulation of the tumour. The absence of catastrophic bleeding in our patient may possibly be due to a higher composition of fibroblastic component as opposed to its vascular component that is often seen in older patients [1].
It appears that there are inherent differences between JA and NSA from clinical and aetiologic perspectives, as summarized in [Table/Fig-5].
Inherent differences between JA and NSA from clinical and aetiologic perspectives
| Juvenile Angiofibroma (JA) | Nasal Septal Angiofibroma (NSA) |
|---|
| 1.Epidemiology | Young adolescent males, patients are 6-26 years old(Mean age: 15.9 years old) [1] | Both males and females, Varied age at presentation, 8-60 years old.Tends to be older(Mean age: 28 years old) |
| 2. Epistaxis at presentation | Common | 25% of reported cases did not present with epistaxis |
| 3. Endoscopy | Obvious mass in nasopharynx | Absence of nasopharyngeal mass |
| 4. Radiology | Hoffmann-Miller’s sign present | Hoffmann-Miller’s sign is absent |
| 5. Aetiology | Arises from ectopic tissue of fascia basalis which is androgen sensitive [2] | Controversial |
| 6. Treatment | Embolisation preoperatively required.Endoscopic endonasal removal from sphenopalatine foramen | No preoperative embolisation required.Endoscopic endonasal septectomy |
JA occurs almost exclusively in young adolescent males, whereas NSA is seen in both males and females. The age at presentation varies widely for NSA, from 8 to 60-year-old, making our patient who was 67-year-old at the time of presentation, the oldest patient diagnosed with NSA. A hormonal theory has been previously proposed to explain the tumour’s tendency to occur in young males. Immunocytochemical techniques have been used to show that androgen receptors are present in both the vascular and stromal elements of at least 75% of the tumours whereas oestrogen receptors have not been demonstrated in the tumour [16]. This lends credence to the role of androgens on the growth of angiofibromas. In our patient, imaging confirmed the angiofibroma to be localised to the perpendicular plate of ethmoid. We speculate that the unusual location of the angiofibroma is due to the presence of ectopic tissue of fascia basalis within the perpendicular plate of ethmoid situated within the posterior septum. This ectopic tissue of fascia basalis is androgen-sensitive [16] but remained dormant initially due to the protective nature of the high levels of oestrogen during her reproductive years. Likely, as the patient went into menopause, a drastic drop in the levels of estrogen leads to the proliferation of the angiofibroma receptors.
Surgery is the mainstay of treatment of angiofibromas. Unlike JA, patients with NSA typically do not undergo pre-operative embolisation as the tumour is comparatively smaller and less vascular [1]. As with JA, an office biopsy is not recommended because of the risk of bleeding. In our patient, the diagnosis of NSA was not suspected. An office biopsy was in fact performed to exclude malignant neoplasm. Surgical approach is determined by the size, location, vascularity or blood supply of the tumour [12]. NSAs are usually small and accessible endoscopically; it is most commonly excised via endoscopic endonasal approach [1–5,7,9–11,13–15]. KK Handa et al., attempted endoscopic excision of the tumour initially but due to excessive bleeding, it was converted to an open approach via lateral rhinotomy [6]. Interestingly, there was also an unusual case of a 9-year-old Asian-American boy who underwent spontaneous auto-amputation of his NSA prior to intervention [8].
Conclusion
This case highlights that angiofibroma may be considered as a differential diagnosis of a septal mass in a post-menopausal woman even in the absence of torrential bleeding. It appears that angiofibromas occurring outside its typical site in the sphenopalatine foramen is clinically distinct, being diagnosed in an older age group with a less vascular behaviour.
[1]. Garcia-Rodriquez Rudman K, Cogbill CH, Loehrl T, Poetker DM, Nasal septal angiofibroma, a subclass of extranasopharyngeal angiofibromaAm J Otolaryngol 2012 33:473-76. [Google Scholar]
[2]. Akbas Y, Anadolu Y, Extranasopharyngeal angiofibroma of the head and neck in womenAm J Otolaryngol 2003 24:413-16. [Google Scholar]
[3]. Windfuhr JP, Remmert S, Extranasopharyngeal angiofibroma: aetiology, incidence and managementActa Otolaryngol 2004 124:880-89. [Google Scholar]
[4]. Hiraide F, Matsubara H, Juvenile nasal angiofibroma: a case reportArch Otorhinolaryngol 1984 239(3):235-41. [Google Scholar]
[5]. Sarpa JR, Novelly NJ, Extranasopharyngeal angiofibroma of the head and neck in womenOtolaryngol Head Neck Surg 1989 101(6):693-97. [Google Scholar]
[6]. Handa KK, Kumar A, Singh MK, Extranasopharyngeal angiofibroma arising from the nasal septumInt J Pediatr Otorhinolaryngol 2001 58:163-66. [Google Scholar]
[7]. Somdas M, Ketenci I, Unlu Y, Extranasopharyngeal angiofibroma originating from the nasal septumOtolaryngol Head Neck Surg 2005 133(4):647 [Google Scholar]
[8]. Castillo MP, Timmons CF, McClay JE, Autoamptation of an extranasopharyngeal angiofibroma of The nasal septumInt J Pediatr Otorhinolaryngol Extra 2000 (Suppl 1):267-70. [Google Scholar]
[9]. Tasca I, Compadretti GC, Extranasopharyngeal angiofibroma of nasal septum. A controversial entityActa Otorhinolaryngol Ital 2008 28:312-14. [Google Scholar]
[10]. Uyar M, Turanli M, Pak I, Extranasopharyngeal angiofibroma originating from the nasal septum: a case reportKulak Burun Bogaz Ihtis Derg 2009 1:19 [Google Scholar]
[11]. Mohindra S, Grover G, Bal AK, Extranasopharyngeal angiofibroma of the nasal septum: a case reportEar Nose Throat J 2009 88:17-19. [Google Scholar]
[12]. Hamdan AL, Moukarbel RV, Kattan M, Natout M, Angiofibroma of the nasal septumMiddle East J Anesthesiol 2012 21(4):653-55. [Google Scholar]
[13]. Correia FG, Simoes JC, Mendes-Neto JA, Seixas-Alves MT, Gregorio LC, Kosugi EM, Extranasopharyngeal angiofibroma of the nasal septum - uncommon presentation of a rare diseaseBraz J Otorhinolaryngol 2013 79(5):646 [Google Scholar]
[14]. Atmaca S, Bayraktar Yildiz L, Extranasopharyngeal angiofibroma of the posterior nasal septum: a rare clinical entityKulak Burun Bogaz Ihtis Derg 2013 23(5):295-98. [Google Scholar]
[15]. Dogan S, Yazici HM, Baygit Y, Metin M, Soy FK, Extranasopharyngeal angiofibroma of the nasal septum: a rare clinical entityJ Craniofac Surg 2013 24(4):390-92. [Google Scholar]
[16]. Hwang HC, Mills SE, Patterson K, Gown AM, Expression of androgen receptors in nasopharyngeal angiofibroma: an immunohistochemical study of 24 casesMod Pathol 1998 11:1122-26. [Google Scholar]