Large Tubullo-villous Adenoma of Duodenum Presenting as Gastric Outlet Obstruction
Utpal Anand1, Manish Kumar Pandey2, Rajeev Nayan Priyadarshi3, Ramesh Kumar4, Binita Chaudhary5
1 Consultant, Department of Gastro Surgery, Paras HMRI Hospital, Patna, Bihar, India.
2 Consultant, Department of Gastro Surgery, Paras HMRI Hospital, Patna, Bihar, India.
3 Assistant Professor, Department of Radiology, IGIMS, Patna, Bihar, India.
4 Consultant, Department of Gastroenterology, Paras HMRI Hospital, Patna, Bihar, India.
5 Senior Resident, Department of Anatomy, AIIMS, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manish Kumar Pandey, Consultant, Department of Gastro Surgery, Paras HMRI Hospital, Patna, Bihar, India.
E-mail: drmanish99@gmail.com
Tubullo-villous adenoma of duodenum is a rare entity. These are potentially malignant tumours and therefore, complete excision is the treatment of choice. However, at times preoperative diagnosis could not be always achieved posing difficulty in choosing the optimal surgical method of excision. We report a 40-year-old male patient presented with vague upper abdominal pain and vomiting for last 6 months. His computed tomography and endoscopy demonstrated intraluminal polypoidal mass. Endoscopic biopsies were negative for malignancy. Local surgical excision with tumour free margin was performed and histology revealed tubullo-villous adenoma.
Endoscopic biopsy, Malignant transformation, Transduodenal excision
Case Report
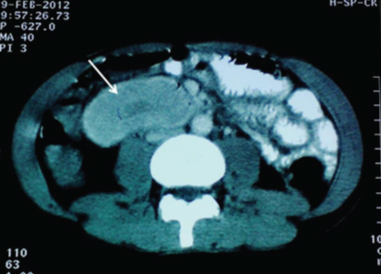
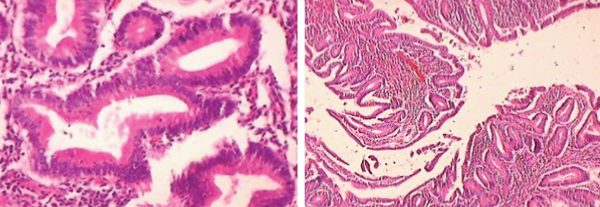
A 40-year-old man presented to the outpatient clinic with vague upper abdominal pain and vomiting for last 6 months. His vital signs were normal. Physical examination revealed mobile epigastric non-tender lump and routine laboratory tests were normal. On Gastroduodenoscopy, a large mobile polypoidal mass was found in the contra lateral portion to the ampulla of Vater [Table/Fig-1]. Multiple biopsy specimens were taken but the report showed non-specific inflammation. Contrast enhanced computed tomography (CT scan) showed bulky intraluminal polypoidal mass in the second and third portion of duodenum [Table/Fig-2]. He underwent transduodenal resection of tumour. On duodenotomy, intraoperative findings was large intraluminal duodenal polyp arising from the anterolateral part of the second portion of the duodenum intussuscepting into the third and fourth portion of the duodenum and proximal jejunum [Table/Fig-3]. Ampulla of vater and medial portion of the second part of duodenum were found not to be involved by tumour. Postoperative course was uneventful. Histopathology report showed Tubullo-villous adenoma with moderate dysplasia [Table/Fig-4].
Contrast enhanced CT shows enhancing intraluminal polypoid mass (arrow) with smooth surface involving second and third portion of duodenum. The duodenal wall appears normal
Upper endoscopic image showing polypoid mobile mass in second part of duodenum

Intraoperative photograph showing cauliflower like polypoid mass arising from second part of duodenum. The surface is fissured in appearance

(H&E Stain. 40X, 10X) Tubulovillus adenoma showing moderate dysplasia involving the duodenum
Discussion
Duodenal tubullo-villous adenomas are uncommon lesions representing less than 1% of all duodenal neoplasm [1]. Tubullo-Villous adenomas are found in the second portion of the duodenum; those that arise in the ampulla and periampullary region have a malignant transformation rate of 30%–60%. They appear as polypoid masses with predominant villous elements at gross inspection. Duodenal Polyps are usually asymptomatic but at times may ulcerate and bleed. Rarely, they may result in obstruction if very large. Our patient presented with abdominal lump, which is unusual for villous adenoma to attain such a large size to be palpable externally. Intraoperative finding was duodenoduodenal intussusception, which is again a very rare finding. Endoscopic examination and biopsy is considered as the best modality of investigation for identification of duodenal villous tumours. On barium meal study these adenomas are seen as intraluminal filling defect. This is a nonspecific finding since similar imaging features can be seen in other intraluminal polypoid or sessile tumours like intraluminal leiomyoma or Brunner’s gland adenoma. Ultrasound is not very useful in identifying duodenal villous lesions [2]. The CT appearance of villous duodenal adenomas is not very specific. They show variegated attenuation and variable enhancement patterns. Large tumours may have a characteristic surface gyral pattern on CT imaging. CT is more useful in determining the extraluminal extent of invasive tumours and assessing regional lymphadenopathy, hence useful for surgical planning [3]. Accurate preoperative histological diagnosis of duodenal villous tumour is difficult. These are frequently large lesions and the small sample taken via the endoscopic biopsy forceps makes the diagnosis inaccurate. False-negative endoscopic biopsy ranges from 25% to 56% in reports [4]. The normal villous architecture of the small intestinal mucosa often makes classification of adenomas of the small bowel difficult [5]. Malignant transformation is also difficult to identify histologically. Similarly, in our case repeated endoscopic biopsies failed to make diagnosis. Treatment of villous tumours of the duodenum can be divided into two procedures: local excision or pancreaticoduodenectomy. Many studies reported a recurrence rate of 46% in patients undergoing local excision [6]. This high rate of local recurrence was attributed to the narrow margins obtained because of the proximity to bile and pancreatic ducts. In our case, we could achieve complete removal of tumour with 1cm margin by transduodenal excision of tumour as it was located in the anterolateral aspect of the second part of duodenum away from the ampulla, hence, pancreaticoduodenectomy could be avoided. The risk for malignant transformation of these tumours is very high, hence serial endoscopic follow-up examinations are recommended for patients who undergo simple local resection [7]. Adenomas are believed to develop from an abnormal process of cell proliferation and apoptosis. Villous type of adenomas are commonly larger in size and are more often associated with severe degrees of dysplasia. Clinical, autopsical, and epidemiological studies provide evidence of adenoma-to-carcinoma progression. Overall, villous adenomas have a malignant transformation risk of 15-25%. The risk of malignant transformation increases with increase in size of adenoma. Risk increases upto 40% in villous adenomas larger than 4 cm in diameter. Therefore, even asymptomatic patients with villous type of adenoma require removal of tumour and careful assessment of histopathology report to identify carcinoma. In our case, final histopathology report showed moderate dysplasia without any evidence of invasive carcinoma.
Duodenal adenomas are extremely common in patients with Gardner’s syndrome and Familial Adenomatous Polyposis (FAP). Polyps in the duodenum occur in 40-90% of FAP patient and these are commonly dysplastic lesions with high risk of cancer. For these reason patient with FAP should go for routine esophagogastroduodenoscopy. It is uncertain whether patients with duodenal adenomas without familial adenomatous polyposis are at greater risk for colorectal neoplasia and, therefore, this patient should routinely undergo surveillance colonoscopy [8].
Conclusion
Tubullo-villous adenomas are very rare tumour of Duodenum. Preoperative diagnosis is difficult at times. Endoscopy and hyptonic duodenography are used for diagnosis of such tumours. It is a potentially malignant tumour; hence complete excision is the treatment of choice. Depending on the localization, extension and size of the tumour, duodenal segment resection, duodenotomy and submucosal excision or duodenopancreatectomy are the best surgical procedures.
[1]. Komorowski RA, Cohen EB, Villous tumours of the duodenum: a clinicopathologic studyCancer 1981 47(6):1377-86. [Google Scholar]
[2]. Bluth EI, Merritt CR, Sullivan MA, Ultrasonic evaluation of the stomach, small bowel, and colonRadiology 1979 133(3 Pt 1):677-80. [Google Scholar]
[3]. Farah MC, Jafri SZ, Schwab RE, Mezwa DG, Francis IR, Noujaim S, Duodenal neoplasms: role of CTRadiology 1987 162(3):839-43. [Google Scholar]
[4]. Ryan DP, Schapiro RH, Warshaw AL, Villous tumours of the duodenumAnn Surg 1986 203(3):301-06. [Google Scholar]
[5]. Aslan S, Cetin B, Markoc F, Cetin A, A duodenal villous adenoma associated with in situ carcinoma: a case reportTurk J Cancer 2001 31(4):162-67. [Google Scholar]
[6]. Braga M, Stella M, Zerbi A, Staudacher C, Sironi M, Di Carlo V, Giant villous adenoma of duodenumBr J Surg 1986 73:924 [Google Scholar]
[7]. Perzin KH, Bridge MF, Adenomas of the small intestine: a clinicopathologic review of 51 cases and a study of their relationship to carcinomaCancer 1981 48:799-819. [Google Scholar]
[8]. Doi K, Iida M, Kohrogi N, Villous adenoma of the duodenum in a patient with familial adenomatosis coliSurg Endosc 1995 9:512-14. [Google Scholar]