Abridged Technique for Precise Implant Angulation
Praveen Perumal1, Gopi Naveen Chander2, Anitha Kuttae Viswanathan3, Ramesh Reddy4, B. Muthukumar5
1 Postgraduate Student, Department of Prosthodontics, SRM Dental College, Ramapuram, Chennai, Tamilnadu, India.
2 Professor, Department of Prosthodontics, SRM Dental College, Ramapuram, Chennai, Tamilnadu, India.
3 Reader, Department of Prosthodontics, SRM Dental College, Ramapuram, Chennai, Tamilnadu, India.
4 Senior Lecturer, Department of Prosthodontics, SRM Dental College, Ramapuram, Chennai, Tamilnadu, India.
5 Professor and Head, Department of Prosthodontics, SRM Dental College, Ramapuram, Chennai, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anitha Kuttae Viswanathan, Department of Prosthodontics, SRM Dental College, Ramapuram, Chennai – 600089, Tamilnadu, India. E-mail : dranikv@yahoo.co.uk
Enormous scientific knowledge with evidence and clinical dexterity impart definitive ground for success in implant dentistry. Nevertheless, the unfeasibility to access the inner bone tissue makes the situation altogether more demanding. Presently the advent of numerous imaging techniques and associated surgical guide templates are documented for evaluation of implant angulation. However, they are not cost effective and consume more time to plan and design the structure. This article describes a simple concise technique for precise implant angulation.
Digital protractor, Implant dentistry
Case Report
A 24-year-old patient reported to the Department of Prosthodontics, SRM Dental College, Ramapuram, and Chennai, India desirous of replacing his lost left upper back tooth. A clinical examination revealed that his maxillary left first premolar was lost as a result of dental caries two months back. Various treatment modalities like Removable Partial Denture (RPD), tooth supported Fixed Partial Denture (FPD), resin bonded FPD, and an implant supported crown was explained to the patient. Since the patient desired a fixed option, RPD was ruled out. The patient did not want his adjacent sound tooth structure to be reduced, hence conventional FPD was eliminated. An Intraoral Peri Apical Radiograph (IOPA) was taken to investigate the availability of bone. It disclosed sufficient bone thus, implant therapy was finalised after obtaining patient consent.
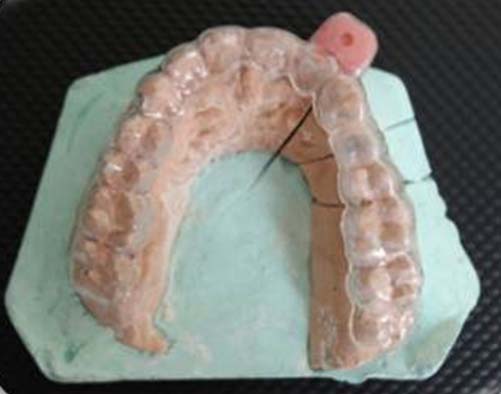
A diagnostic impression was made with irreversible hydro colloid (Zelgan, DentsplyDeTrey GmbH). Maxillo-mandibular relation was recorded using polyvinyl siloxane bite registration paste material (Virtual CADbite Registration, Ivoclar Vivadent). Face bow transfer was done with the Hanau Spring-Bow and the casts were articulated on a Hanau Wide- Vue 183-2 semi adjustable articulator. A comprehensive evaluation of the casts was done. Bone mapping, to determine the soft tissue thickness and available bone topography was done in a conventional manner on a duplicate diagnostic cast. Local anaesthetic gel was applied on the edentulous site in the patient’s mouth. A perpendicular cut was then made in the centre of the edentulous ridge of the diagnostic cast. An endodontic K file, size no. 25 with a rubber stopper was inserted through the patient’s mucosa over the site of the implant to determine the soft tissue thickness. The file was pierced into the crest of the ridge, at two markings on buccal and palatal side, in order to reproduce the osseous and soft tissue topography. The markings obtained from the file were transferred to the sectioned cast. The file was pierced on the crest, facial and palatal side of the ridge in the patient’s mouth. The marked areas on the cast were joined and shaded to distinguish the amount of soft tissue thickness and the contour of the underlying bone [Table/Fig-1].
Bone mapping sectioned cast

Diagnostic wax up for the missing premolar was done on another set of casts. An impression of the waxed up cast was made with irreversible hydro colloid and poured with type III dental stone. A thermoplastic resin sheet (Duran, Biostar, Scheu Dental) of 1mm thickness was used to fabricate a template over the maxillary cast. The template was made to adapt over the teeth and excess resin sheet was trimmed till the gingival contours of the buccal aspect of ridge. In order to counter the difference in implant angulation, a transferable reference guide with self-cure acrylic resin (RR Cold Cure, DPI) was made and fastened to the clear resin surgical template in the adjacent abutment tooth area. A slot of pilot drill diameter was made into the reference guide [Table/Fig-2].
Transferable reference guide with clear resin template.
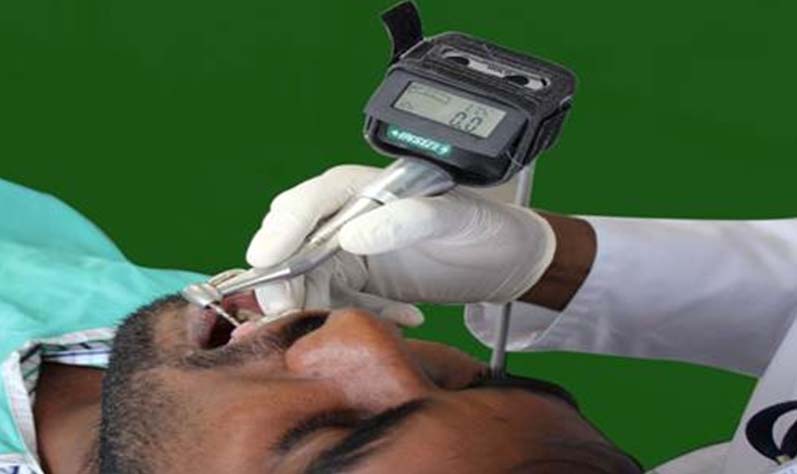
A mechanical device named "Digital Protractor" (2178-1, Insize digital level and protractor, Precision Measurement & Control Solutions from CDI) which is an instrument employed for measuring angles of slope or tilt with respect to gravity was used in the study to determine the tilt of the hand piece. It is a dual axis instrument with width to height measurement of 60mm - 56mm. A tilt of 0-180 degrees could be detected with 0.1o (=1.745mm/m) resolution at an accuracy of ±0.1o [Table/Fig-3]. An inbuilt display monitor was present to show the numerical tilt value [Table/Fig-4]. This device was secured to the dental hand piece with the help of a belt [Table/Fig-5]. The tilt of the hand piece in a clockwise or anti clockwise direction was demonstrated by the reading shown in the display unit of the device. The inclination of the hand piece was set to zero degree by placing into the slot of the reference guide.
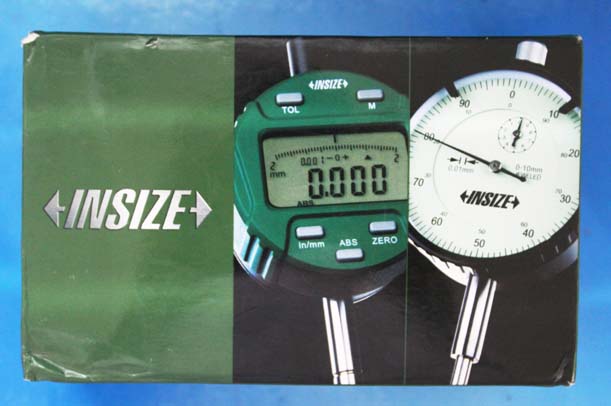
Display monitor of the protractor.

Digital protractor secured to hand piece

A trial of the template with the reference guide was monitored in the patient’s mouth. The patient was asked to tilt his head to left and right to check zero degree in inclinometer when the pilot drill was in guiding slot [Table/Fig-6]. With the assistance of the reference guide template and protractor affixed to the hand piece, osteotomy was done within the decided angulation of 20-23 degrees from the reference guide angle [Table/Fig-7].
Zero degree inclination checked in patient’s mouth.
Precise angulation of implant.

Angulation of the implant placed with this technique was more precise at a predetermined angle of 22 degrees and was ascertained with a post-operative radiograph [Table/Fig-8]. Abrupt angular deviation was not evident. Any alteration in the direction of the hand piece was demonstrated as a numerical value in the protractor.

Discussion
The successful outcome of any dental implant procedure depends on various patient related and procedure associated parameters like general health conditions, implant characteristics, nature and amount of existing bone, surgical procedure. Multitudes of significant elements play a role in obtaining a positive outcome of dental implant therapy. Each factor emphasizes on the importance of their role in treatment [1,2]. An artificial substitute for lost tooth structure must simulate natural dentition in restoration of function, aesthetics and phonetics. Among the many factors contributing to the outcome of the treatment, implant angulation plays a pivotal role in directing the occlusal loads to the underlying bone [3–5]. Placement of implant into the underlying osseous structure is to be done at accurate angulation to avoid off axis occlusal loading and to prevent damage to the adjacent sound structures [6]. An enhancement in aesthetics is not feasible to achieve from an improperly angulated implant. In this regard leaps and bounds of research have been performed through the years [7–8]. The development of digital imaging technology assists the operator in the surgical and prosthetic intervention of the patient to optimally place the implant in surgical bed [9–11].
With myriad of research in determination of precise implant angulation, the status of digital imaging techniques and utilisation of surgical guide templates are more absolute. However, a higher cost and dose of radiation, limits the usage of latest 3D imaging modalities as a conventional procedure. The ratio of risk to benefit in the field of radiology cannot be blinded. Besides, the high costs of 3D imaging investigations departs it’s usage as a conventional method [12]. The surgical templates are fabricated on dental casts which are rigid, non-functional surface without the knowledge of underlying soft tissue resiliency and bone topography. Despite the sophistication of current dental technology, all dental operations are performed by hand. Therefore maintaining the angulation of the hand piece during osteotomy is very crucial [13,14]. Thus an attempt was made to transfer an ideal implant position precisely with the application of a mechanical device inclinometer secured to the hand piece. The numerical display in the digital protractor dictated the angular signal during the procedure. Any minor deviation either by the change in the angulations of the hand piece or the tilt of the patient’s head was instantly indicated in the display monitor. With the reference guide, the angle of the hand piece was pre-set to zero degree prior to start of the osteotomy. The various techniques employed for correct implant placement with their pros and cons are enlisted in [Table/Fig-9].
Techniques used for precise implant angulation.
| Systems | Technique | Advantages | Disadvantages |
|---|
| Conventional surgical template | Autopolymerizing acrylic resin surgical template made on dental casts with panoramic radiography (OPG), lateral cephalogram | Inexpensive, easy to fabricate, improved visibility | Diagnostic limitations such as distortion of OPG, 2D imaging, can not view bone in bucco-lingual direction, made on rigid dental casts, no 3D guidance, arbitrarily guided through the template |
| Vacuum formed thermoplastic matrix (0.02 inch) guide made on dental casts | Matrix dictates implant angulations with minimal surgical interference |
| Computer generated surgical templates using CT* or CBCT** | Surgical guides with radiographic markers | 3D imaging, precise surgical osteotomy sites, preservation of anatomic structures | Special training for familiarity with entire system needed, special equipment necessary, intrinsic errors during scanning, lack tactile control during surgical procedure, expensive, no quantitative indication when angulations is changed within the osseous structure |
| Stereolithographic CAD-CAM*** templates | Computer generated drilling guides obtained |
| Computer milled templates | Final position of implant pre-visioned in scanning template by drilling machine |
| Computer navigation system | Permits an intraoperative real-time bur tracking according to planned trajectory |
*CT – Computer Tomography
**CBCT – Cone Beam Computer Tomography
***CAD-CAM – Computer Aided Design – Computer Aided Machining
The digital protractor used is a dual axis instrument and its size is not compact. Handling this device with the implant hand piece required dexterity. These limitations can be overthrown by advancements in the form of triple axis inclinometer. An inbuilt feature of axis detection can be incorporated into the hand piece. Further progression in improvisation of the digital device, can be made to produce alarming signals in case of any deviation from pre-set implant angulations. Alerting signals either in the form of colour change in display unit or sound peep can be made to demonstrate the deviations.
Conclusion
Thus, it can be concluded that a mechanical digital protractor fastened to dental hand piece can be effectively used for placement of implant in precise angulation. This novel application serves as a definitive technique rather than conventional arbitrary method. In situations where a higher end imaging technology cannot be employed, this procedure would be more favourable in clinical practice.
*CT – Computer Tomography
**CBCT – Cone Beam Computer Tomography
***CAD-CAM – Computer Aided Design – Computer Aided Machining
[1]. Geckili O, Bilhan H, Geckili E, Cilingir A, Mumcu E, Bural C, Evaluation of possible prognostic factors for the success, survival, and failure of dental implantsImplant Dent 2014 23(1):44-50. [Google Scholar]
[2]. Misch CE, Contemporary implant dentistry: Implant success or failure: clinical assessment in implant dentistry 1999 2nd edSt LouisMosby [Google Scholar]
[3]. Mello LA, Garcia RR, Leles JL, Leles CR, Silva MA, Impact of cone-beam computed tomography on implant planning and on prediction of implant sizeBraz Oral Res 2014 28(1):46-53. [Google Scholar]
[4]. Kalra M, Aparna IN, Dhanasekar B, Evolution of surgical guidance in implant dentistryDent Update 2013 40(7):577-8.:581-82. [Google Scholar]
[5]. Arun Kumar G, Mahesh B, George D, Three dimensional finite element analysis of stress distribution around implant with straight and angled abutments in different bone qualitiesJ Indian Prosthodont Soc 2013 13(4):466-72. [Google Scholar]
[6]. Lee DW, Lee DW, Park KH, Moon IS, The effects of off-axial loading on periimplant marginal bone loss in a single implantJ Prosthet Dent 2014 112(3):501-07. [Google Scholar]
[7]. Tischler M, Ganz SD, The CT/CBCT-based team approach to care. Part I: Identifying the implant patient and prosthetic optionsDent Today 2012 31(8):74-79. [Google Scholar]
[8]. Tetradis S, Anstey P, Graff-Radford S, Cone beam computed tomography in the diagnosis of dental diseaseJ Calif Dent Assoc 2010 38(1):27-32. [Google Scholar]
[9]. Gher ME, Richardsen AC, The accuracy of dental radiographic techniques used for evaluation of implant fixture placementInt J Periodontics restorative dent 1996 15:269-85. [Google Scholar]
[10]. Castro-Ruiz CT, Noriega J, Guerrero ME, Validity of ridge mapping and cone beam computed tomography in dental implant therapyJ Indian Soc Periodontol 2015 19(3):290-93. [Google Scholar]
[11]. Sethi A, Sochor P, Predicting aesthetics in implant dentistry using multiplanar angulation: a technical noteInt J Oral Maxillofac Implants 1995 10(4):485-90. [Google Scholar]
[12]. Phillips K, Kois JC, Aesthetic peri-implant site development. The restorative connectionDent Clin North Am 1998 42(1):57-70. [Google Scholar]
[13]. Buser D, von Arx T, Surgical procedures in partially edentulous patients with ITI implantsClin Oral Implants Res 2000 11(Suppl 1):83-100. [Google Scholar]
[14]. Soares MM, Harari ND, Cardoso ES, Manso MC, Conz MB, Vidigal GM, An in vitro model to evaluate the accuracy of guided surgery systemsInt J Oral Maxillofac Implants 2012 27(4):824-31. [Google Scholar]