Placenta Percreta Presenting with Delayed Haematuria
Vinayak Gorakhanath Wagaskar1, Sudarshan Omprakash Daga2, Sujata Kiran Patwardhan3
1 Resident, Department of Urology, King’s Edward Memorial Hospital and S.G.S. Medical College, Mumbai, India.
2 Resident, Department of Urology, King’s Edward Memorial Hospital and S.G.S. Medical College, Mumbai, India.
3 Professor and Head, Department of Urology, King’s Edward Memorial Hospital and S.G.S. Medical College, Mumbai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vinayak Gorakhanath Wagaskar, Resident, Department of Urology, 8th Floor New Building, Kings Edward Memorial Hospital and S.G.S. Medical College, E Borges Road, Parel; Mumbai-400012, India.
E-mail: vinayakwagaskar99@gmail.com
Placenta percreta presents as life threatening complications with bladder invasion. A condition of placenta invading urinary bladder presented with differential diagnosis of gestational trophoblastic neoplasia on imaging and responded to chemotherapy. A 35-year-old primi-gravida presented at term with per vaginal bleeding. During caesarian section placental mass totally invading uterine myometrium was found. She was given single dose of Methotrexate. After 2 months she presented with gross haematuria with clot retention two times. Her MRI was suggestive of gestational trophoblastic neoplasia of size 19 X 10 X 13cm. Her beta-Human Chorionic Gonadotropin levels were 691.23 mIU/ml. She was given total four doses of methotrexate. At present size of mass was 1.6 X1.3X 1.1cm. Her beta Human Chorionic Gonadotropin level dropped down to 2mIU/ml. Patient was not willing for further intervention or for follow up.
Bladder invasion, Hysterectomy, Mass methotrexate, Placenta percreta
Case Report
A 35-year-old primi-gravida presented at term with per vaginal bleeding. She underwent elective caesarian section in July 2014. As she was not a registered case, she did not have routine ultrasound examination during ante-natal period.
Intraoperatively, she was found to have placenta totally invading uterine myometrium. Placenta was left in situ as it was adhered and imaging was not available and baby delivered. No biopsy was taken during caesarian section. Her beta-Human Chorionic Gonadotropin levels were 691.23 mIU/ml. She was given injection Methotrexate 65 mg post-delivery. Patient was discharged on 7th postoperative day and advised to follow up with imaging after 2 weeks period but she did not review.
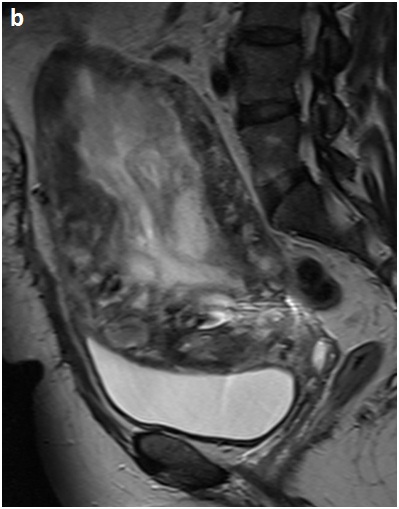
After 2 months the patient presented with haematuria. She was managed conservatively with clot evacuation. Again after 5 days she had similar episodes with clot retention along with urinary tract infections. Again she underwent clot evacuation and course of antibiotics. MRI Pelvis [Table/Fig-1a&b] suggestive of mass approximately of size 19x10x13cm with lobulated heterogeneous T2 intermediate signal intensity seen within endometrial lining extending into myometrium. The lesion was seen extending into superior wall of urinary bladder also encasing left distal ureter with upstream dilatation.
Coronal section T1 W:Mass approximately of size 19 X 10 X 13cm with lobulated extending into superior wall of urinary bladder
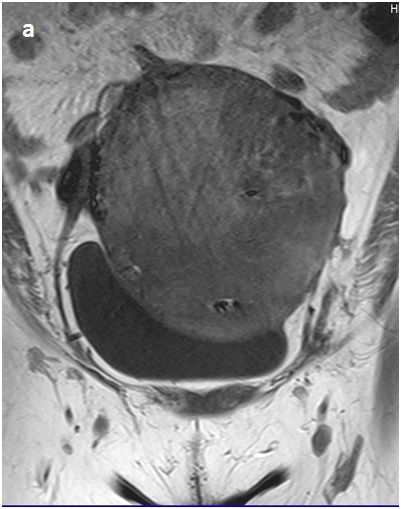
OAxial section T2 W: Heterogeneous signal intensity and extending into superior wall of urinary bladder also encasing left distal ureter with upstream dilatation
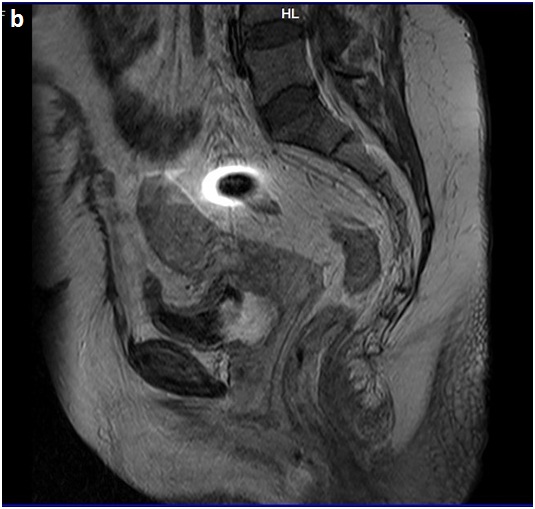
Patient underwent cystoscopy for haematuria and clot retention. Findings were suggestive of hyperaemia of entire bladder mucosa along left lateral wall including left ureteric orifice. Mucosa was bleeding on touch. Left double J stenting was done in view of hydro-ureteronephrosis on that side. Patient treated as placenta percreta and received three doses of Methotrexate 50mg every alternate day. There was improvement in her symptoms. She underwent cystoscopy after three months. It showed hyperaemic patch over left ureteric orifice and double J stent was removed. Her beta Human Chorionic Gonadotropin levels dropped down to 2mIU/ml. Follow up MRI Pelvis was suggestive of residual lesion in antero-inferior wall of uterus with persistent invasion in right postero-superior wall of the bladder measuring approximately 1.6X1.3X1.1cm [Table/Fig-2a&b]. Patient was advised open exploration and biopsy. But she was unwilling for the same.
Coronal section T1 W: Residual lesion in antero-inferior wall of uterus

Axial section T1 W:Residual lesion of uterus with persistent invasion in right postero-superior wall of the bladder
Discussion
Bladder invasion by the placenta (placenta percreta) is a potentially life-threatening obstetric complication. The diagnosis is usually established when attempts are made to separate the adherent placenta from the bladder [1]. The management of placenta percreta with invasion into urinary bladder is not well established due to lack of Randomized controlled trials of this uncommon but increasingly significant abnormality. For effective management, familiarity with this condition is crucial. The incidence of placenta accreta has increased recently with increasing cesarean delivery rate. It was 1 in 533 pregnancies for the period of 1982–2002 [2].
Gupta et al., found this condition in 15 weeks pregnancy [3]. They performed open exploration with hysterectomy and en bloc removal of clot along with bladder wall. In our case, patient diagnosed during delivery and responded to methotrexate. Women are at greater risk of placenta accreta whose myometrial damage has occurred due to previous caesarian delivery. Other reasons cited are advanced maternal age, previous myomectomy and endometrial defects due to vigorous curettage causing Asherman syndrome [4], thermal ablation [5] and uterine artery embolization [6]. Placenta percreta without prior myometrial damage constitute 5% or less of total placenta accreta cases. The present case was 35-year-old primi delivery. Besides advanced age, no contributable risk factor was present. She was non registered case. Hence Antenatal imaging was not available to document placenta percreta.
It is accepted that placenta accreta is delivered through caesarian section. There are two major management options for placenta percreta; cesarean hysterectomy and cesarean delivery with conservative management of the placenta. ACOG approved hysterectomy as the primary treatment for placenta accreta but it was associated with a high morbidity and mortality [7].
Our patient received total four doses of Methotrexate. Patient also underwent cystoscopy and left double stenting. Till now, no case reported in the literature with placenta percreta invading urinary bladder with distal ureteric involvement. Crespo et al., gave 4 doses of Methotrexate intramuscularly every other day in a case of placenta percreta approximately 7X7cm size. After seven months, patient passed fleshy tissue mass vaginally with subsequent ultrasound examination documented empty uterine cavity [8].
Teskin et al., gave 5 doses of Methotrexate by weekly intervals at 100 mg dose. They performed bilateral internal artery ligation at the time of caesarian section. They observed no change in placenta mass size, vascularity and bladder invasion, except for decreasing HCG levels. They performed hysterotomy with manual removal of placental mass following which she returned to normal menses at 4 months postoperatively [9]. Our patient responded to Methotrexate.
Conclusion
Though hysterectomy is the primary treatment of placenta percreta our case report showed methotrexate as the treatment modality can be an alternative. Further large studies are required to establish methotrexate as treatment modality.
[1]. Konijeti R, Rajfer J, Askari A, Placenta percreta and the urologistRev Urol 2009 11(3):173-76. [Google Scholar]
[2]. Wu S, Kocherginsky M, Hibbard JU, Abnormal placentation: twenty-year analysisAm J ObstetGynecol 2005 192:1458-61.[PubMed] [Google Scholar]
[3]. Gupta P, Pradeep Y, Goel A, Singh R, Haematuria: an unusual presentation of placenta percretaUrology 2012 80(2):e13-14. [Google Scholar]
[4]. Al-Serehi A, Mhoyan A, Brown M, Benirschke K, Hull A, Pretorius DH, Placenta accreta: an association with fibroids and Asherman syndromeJ Ultrasound Med 2008 27:1623-28.[PubMed] [Full Text] [Google Scholar]
[5]. Hamar BD, Wolff EF, Kodaman PH, Marcovici I, Premature rupture of membranes, placenta increta, and hysterectomy in a pregnancy following endometrial ablationJ Perinatol 2006 26:135-37.[PubMed] [Full Text] [Google Scholar]
[6]. Pron G, Mocarski E, Bennett J, Vilos G, Common A, Vanderburgh L, Pregnancy after uterine artery embolization for leiomyomata: the Ontario multicenter trial. Ontario UFE Collaborative GroupObstetGynecol 2005 105:67-76.[PubMed] [Obstetrics & Gynecology] [Google Scholar]
[7]. Committee on Obstetric PracticeACOG committee opinion. Placenta accretaInt J GynaecolObstet 2002 77:77-8.:10 [Google Scholar]
[8]. Crespo R, Lapresta M, Madani B, Conservative treatment of placenta increta with methotrexateInternational Journal of Gynecology and Obstetrics 2005 91:162-63. [Google Scholar]
[9]. Teksin C, Cem Y, Sait Y, Serdar O, Conservative management of placenta previa percreta by leaving placental tissue in situ with arterial ligation and adjuvant methotrexate therapyJ Turkish-German Gynecol Assoc 2011 12:127-29. [Google Scholar]