Gallstone disease is one of the most common problems affecting the digestive tract. The prevalence of gallstones is related to factors like age, gender, and ethnic background. The prevalence of gallstone varies widely from place to place. It is estimated that approximately 20 million people in the United States have gallstones and that approximately 1 million new cases of cholelithiasis develop each year. In India the prevalence is estimated to be around 4% [1] changing incidence in India is mainly attributed to westernization of diet, change in socioeconomic structure and availability of ultrasound as investigation in both rural and urban areas.
The National Institute of Health (NIH) consensus development conference in the year 1992 concluded that laparoscopic cholecystectomy provides a safe and effective treatment for most patients with symptomatic gallstones [2].
At present, laparoscopic cholecystectomy (LC) is considered the treatment of choice for symptomatic cholelithiasis. It has many advantages over open cholecystectomy in terms of minimal postoperative pain, shorter hospital stay, better cosmetics and early recovery. As the experience with LC is increasing throughout the world, selection criteria have become more liberal. Most of the factors like morbid obesity and previous upper abdominal surgery which were considered as absolute contraindication for attempting LC have no longer remained as absolute contraindications. The number of contraindications has come down significantly over time. Attempts can be made in all cases of gall stone diseases with laparoscopic procedure except for patients with bleeding diathesis, carcinoma gallbladder and patients not fit for general anaesthesia [3].
However, of all Laparoscopic cholecystectomies, 1-13% requires conversion to an open for various reasons [4]. Thus, for surgeons it would be helpful to establish criteria that would assess the risk of conversion preoperatively. This would be useful for informing patients and a more experienced surgical team could be assembled when risk for conversion appears significant. Thus this study is conducted at our hospital to predict the difficult laparoscopic cholecystectomy and conversion using various clinical and radiological parameters.
To predict difficult laparoscopic cholecystectomies by clinico-radiological assessment.
Materials and Methods
In this prospective study all patients who require cholecystectomy for reasons like acute calculous cholecystitis and chronic calculous cholecystitis were included. Exclusion criteria were presence of jaundice, cholangitis, raised alkaline phosphatase, dilated common bile duct, common bile duct stones, empyema of gall bladder and Acalculous cholecystitis. One hundred and eighty patients who underwent LC between October 2010 and October 2014 met the inclusion criteria. Details of cases were recorded including history, clinical examination and investigations done. Four parameters number of attacks, total leucocyte count, gall bladder wall thickness and pericholecystic fluid collection on ultrasonography of each patient were recorded preoperatively and compared with intaoperative findings. Intraoperative findings were divided into easy laparo scopic cholecystectomy, difficult laparo scopic cholecystectomy and conversion to open cholecystectomy. Difficult laparoscopic cholecystectomy was judged based on presence of at least one of the following i.e. dense adhesions between gallbladder and surrounding, dense adhesions between gallbladder and liver bed and frozen Calot’s triangle.
Results
This study included 180 cases that were studied prospectively over a period of 4 years, from October 2010 to October 2014. The statistical analysis was done using Z-test.
Age Distribution of Patients
In the present series the youngest patient was 14 years of age and the oldest was 80 years of age. Majority of the patients in the present series were in the age group of 31-50 years of age as shown in [Table/Fig-1].
Showing the age wise distribution of cholelithiasis
| Age in years | No. of patients |
|---|
| 10 – 20 | 11 |
| 20 – 30 | 30 |
| 30 – 40 | 38 |
| 40 – 50 | 41 |
| 50 – 60 | 26 |
| 60 – 70 | 23 |
| 70 – 80 | 11 |
The mean age of patients in non converted group is 44.1 years and 62.33 years in converted group. The mean age in non converted patients was not statistically different from the conversion patients (p=0.22, 95% confidence interval).
Sex Distribution
Out of total 180 patients 115 were females and 65 were males. Male: female ratio is 1: 1.76
Conversion of laparoscopic cholecystectomy to open surgery in males and females
Out of 65 male patients 7 were converted to open cholecystectomy and out of 115 females 3 were converted. The conversion rate in males was statistically significant (p = 0.034, 95% confidence interval.
Distribution of Surgical Outcome
Out of 180 patients included in this study 126 were easy, 44 were difficult and 10 patients required conversion to open cholecystectomy. The overall conversion rate was 5.55%.
Number of Attacks
Out of 180 patients, 65 patients had history of similar cholecystitis attacks in the past and 115 patients had no such attacks previously as shown in [Table/Fig-2].
Change in frequency of difficulty and conversion with number of attacks
| No of attacks | Easy | Difficult | Conversion | Total |
|---|
| 1 | 99 | 14 | 2 | 115 |
| 2 | 23 | 14 | 3 | 40 |
| 3 and more | 4 | 16 | 5 | 25 |
It was found that the difficult laparoscopic cholecystectomy and conversion were not significantly different when compared between patients with first attack and patients with more than 1 attack. But patients with >2 attacks had significant high rates of difficulty (21.29% vs 84%, p = 0.01, 95% confidence interval) and conversion (3.22% vs 20%, p = 0.03, 95% confidence interval) compared to patients with 2 and less than 2 attacks (as shown in [Table/Fig-3]).
Predicting difficult laparoscopic cholecystectomy and conversion of laparoscopic cholecystectomy to open surgery based on number of attacks >2
| Difficult | | Conversion |
|---|
| p-value | 0.01 | | p-value | 0.03 |
| Sensitivity | 38.88 | | Sensitivity | 50 |
| Specificity | 96.82 | | Specificity | 88.23 |
| Positive predictive value | 84 | | Positive predictive value | 20 |
| Negative predictive value | 78.70 | | Negative predictive value | 96.77 |
The sensitivity, specificity, positive predictive value and negative predictive value of no. of attacks >2 in predicting difficult laparoscopic cholecystectomy are 38.88%, 96.82%, 84% and 78.70% respectively.
The sensitivity, specificity, positive predictive value and negative predictive value of no of attacks >2 in predicting conversion of laparoscopic cholecystectomy to open surgery are 50%, 88.23%, 20% and 96.77% respectively.
Mean Number of Attacks
It was found that the mean number of attacks of cholecystitis was highest in converted group and least in easy cholecystectomy group. The mean attacks in easy group was 1.285, difficult group was 2.333 and 3.666 in converted group.
Total Leucocyte Count
Out of 180 patients included in this study, 36 patients had TLC more than 11000/cumm and 144 patients had less than 11000/cu mm as shown in [Table/Fig-4].
Change in frequency of conversion with change in total leukocyte count
| TLC (per cumm) | Easy | Difficult | Conversion | Total |
|---|
| 4000-11000 | 118 | 24 | 2 | 144 |
| >11000 | 8 | 20 | 8 | 36 |
It was found that patients with TLC >11000/cu mm had significant high rates of difficulty (18% vs 77.77%, p = 0.02, 95% confidence interval) and conversion (1.38% vs 22.22%, p = 0.03, 95% confidence interval) compared to patients with TLC <11000/cu mm (as shown in [Table/Fig-5]).
Predicting difficult laparoscopic cholecystectomy and conversion of laparoscopic cholecystectomy based on TLC >11000
| Difficult | | Conversion |
|---|
| p-value | 0.02 | | p-value | 0.03 |
| Sensitivity | 51.85 | | Sensitivity | 80 |
| Specificity | 93.65 | | Specificity | 83.52 |
| Positive predictive value | 77.77 | | Positive predictive value | 22.22 |
| Negative predictive value | 81.94 | | Negative predictive value | 98.61 |
The sensitivity, specificity, positive predictive value and negative predictive value of TLC > 11000/cu mm in predicting conversion of laparoscopic cholecystectomy to open surgery are 80%, 83.52%, 22.22% and 98.61% respectively.
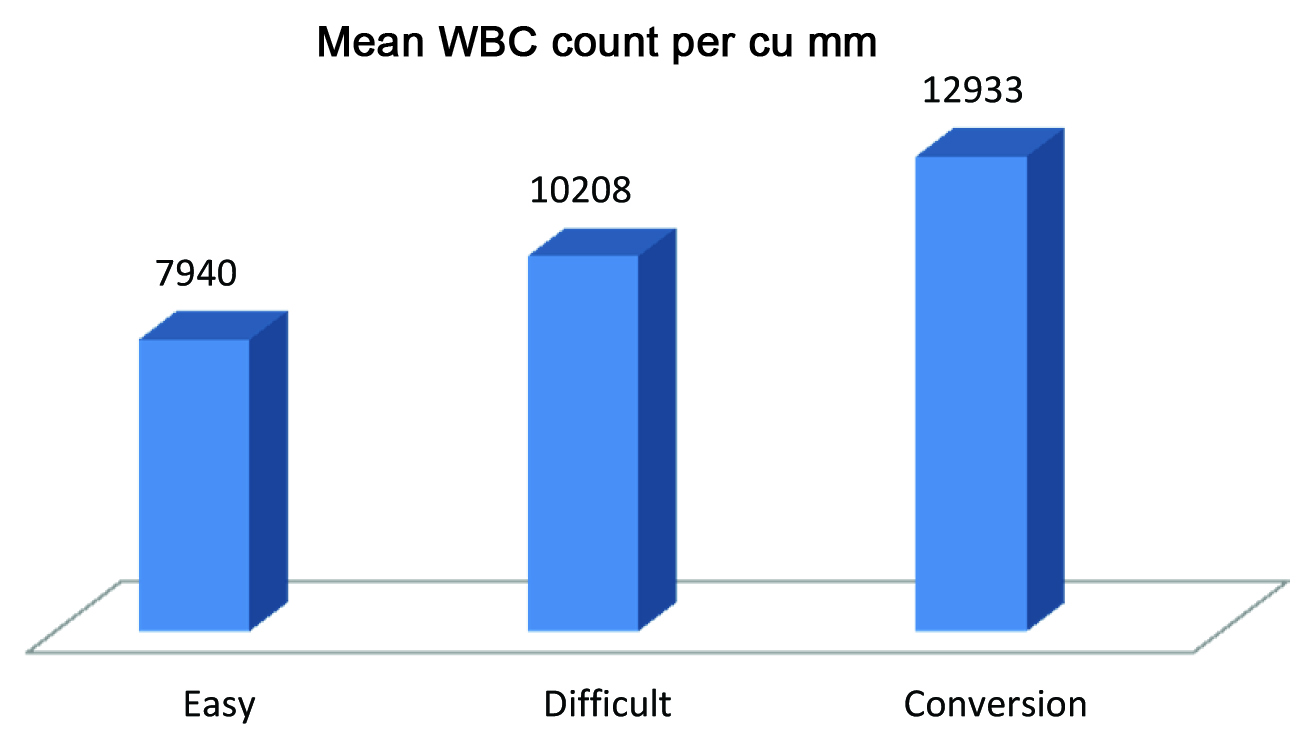
The mean WBC count in difficult LC and conversion group was significantly higher compared to easy group as shown in [Table/Fig-6].
Showing mean WBC count in each group
Gall bladder Wall thickness
As shown in [Table/Fig-7], Out of 180 patients included in this study 28 patients had gall bladder wall thickness more than 3mm and 152 patients had less than 3 mm.
Change in frequency of difficulty and conversion with change in gall bladder wall thickness on USG
| GBwall thickness (mm) | Easy | Difficult | Conversion | Total |
|---|
| <3 | 119 | 30 | 3 | 152 |
| >3 | 7 | 14 | 7 | 28 |
It was found that patients with gall bladder wall thickness >3 mm had significantly high rates of difficulty (21.71% vs 75%, p = 0.01, 95% confidence interval) and conversion (1.97% vs 25%, p = 0.01, 95% confidence interval) compared to patients with gall bladder wall thickness < 3 mm (as shown in [Table/Fig-8]).
Predicting difficult laparoscopic cholecystectomy and conversion of laparoscopic cholecystectomy based on gall bladder wall thickness >3mm.
| Difficult | | | Conversion | |
|---|
| p-value | 0.01 | | p-value | 0.01 |
| Sensitivity | 38.88 | | Sensitivity | 70 |
| Specificity | 94.44 | | Specificity | 87.64 |
| Positive predictive value | 75 | | Positive predictive value | 25 |
| Negative predictive value | 78.28 | | Negative predictive value | 98 |
The sensitivity, specificity, positive predictive value and negative predictive value of gall bladder wall thickness >3 mm in predicting conversion of laparoscopic cholecystectomy to open surgery are 70%, 87.64%, 25% and 98% respectively.
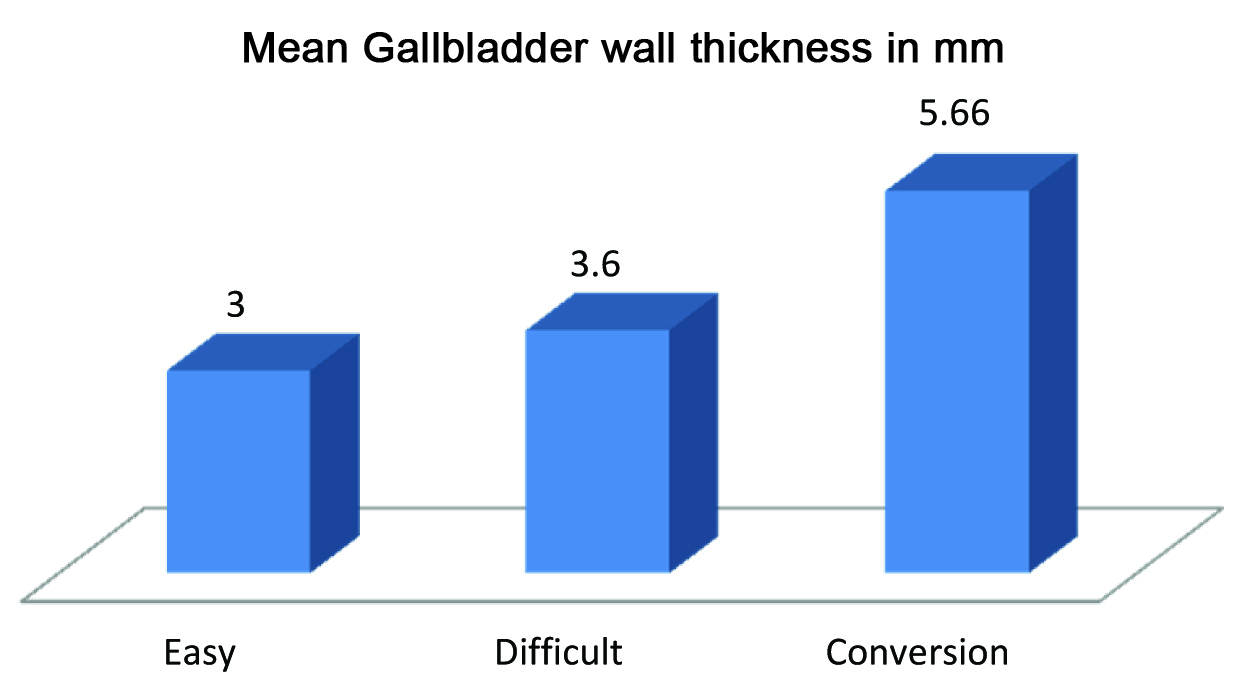
As shown in [Table/Fig-9], the mean gall bladder wall thickness in easy group was 3 mm, difficult group was 3.6mm and 5.66mm in conversion group.
Showing mean gallbladder wall thickness (in mm) in each group
Pericholecystic Collection
Out of 180 patients included in this study, 21 patients had Pericholecystic collection on USG (as shown in [Table/Fig-10])
Change in frequency of conversion with change in Total Leukocyte Count.
| Pericholecystic collection | Easy | Difficult | Conversion | Total |
|---|
| Absent | 122 | 34 | 3 | 159 |
| present | 4 | 10 | 7 | 21 |
It was found that patients with pericystic collection had significant high rates of difficulty (23.27% vs 80.95%, p = 0.01, 95% confidence interval) and conversion (1.88% vs 33.33%, p = 0.02, 95% confidence interval) compared to patients without collection.
The sensitivity, specificity, positive predictive value and negative predictive value of Pericholecystic collection in predicting conversion of laparoscopic cholecystectomy to open surgery are 70%, 91.76%, 33.33% and 98.11% respectively (as shown in [Table/Fig-11]).
Predicting difficult laparoscopic cholecystectomy and conversion of laparoscopic cholecystectomy based on pericystic collection
| Difficult | | Conversion |
|---|
| p-value | 0.01 | | p-value | 0.02 |
| Sensitivity | 31.48 | | Sensitivity | 70 |
| Specificity | 96.82 | | Specificity | 91.76 |
| Positive predictive value | 80.95 | | Positive predictive value | 33.33 |
| Negative predictive value | 76.72 | | Negative predictive value | 98.11 |
Discussion
Laparoscopic cholecystectomy (LC) being the gold standard treatment of symptomatic cholelithiasis preoperative prediction of the risk of conversion is an important aspect of planning laparoscopic surgery. It is important to predict difficult LC preoperatively so that senior surgeons can be requested to be present during surgery rather than less experienced junior surgeon prolonging the surgery which may lead to intraoperative complications. In preoperatively predicted to be conversion, early decision of conversion can be made so as to avoid unnecessarily prolonging the surgery and to prevent complications. Many studies have attempted form a scoring system to predict difficult LC, but most of them are complex, use large number of determining factors, and they are difficult to use in day today practice [5–8]. And many of these scoring systems cannot be applied preoperatively [5].
The overall conversion rate in our study was 6%. S Kumar et al., conducted a study which included 536 patients who underwent laparoscopic cholecystectomy [9]. The Overall conversion rate in their study was 7.81%. Sharma SK et al., conducted a study on 200 patients undergoing laparoscopic cholecystectomy at Kathmandu medical college [4]. The conversion rate in their study was 4%.
In most of the studies age was considered as a risk factor for conversion [10–16]. We and some other authors did not notice age to be associated with conversion rate [17,18]. In our study the mean age in non converted patients and converted patients are 44.1 years and 62.33 years respectively but statistically they were not different from each other (p=0.22, 95% confidence interval).
Male sex as an independent risk for conversion is controversial. Few series have shown it to be an independent risk factor [13,14,17,19–22]. However, Liu et al., did not notice sex to be associated with conversion [12]. In our study, male sex was found to be a risk factor for conversion (p = 0.034, 95% confidence interval).
Our study data analysis revealed that there was significantly high risk of difficulty and conversion in patients with previous history of more than 2 attacks of acute cholecystitis (p=0.03, 95% confidence interval). Similar result has been concluded in other studies as well [12,13,21,23]. Sanabria et al., found in their study of 628 patients that patients with multiple attacks (ten or more) were significantly associated with conversion, but in our study we found significance with a number of attacks more than two [14]. In our study mean number of attacks in easy, difficult and converted groups were 1.28, 2.33 and 3.66 respectively. Schrenk et al., reported in a study of 300 patients assessing 24 variables for conversion that patients with history of acute cholecystitis within the last 3 weeks were at increased risk of conversion [24].
Many studies have identified raised WBC as a risk factor for predicting conversion [11,15,21,24]. In our study, there was significantly more risk of conversion in patients having TLC >11000/cumm. (p=0.037, 95% confidence interval). This can be probably attributed to persisting acute inflammation with edema of the gall bladder making surgery difficult. The mean TLC in converted group of our study was 12933/cumm compared to 10195/cumm in a study conducted by Sanjeev Kumar et al., [9].
Gall bladder wall thickness has been identified as a risk factor for conversion in almost all the studies. The thickness of gall bladder associated with conversion varies from study to study. It was 3mm [13,25], 4mm [10]. In our study the critical gall bladder wall thickness was 3mm. The mean gall bladder wall thickness in easy, difficult and conversion group was 3, 3.6, 5.6 respectively.
Conclusion
We conclude that the difficult laparoscopic cholecystectomy and conversion to open surgery can be predicted preoperatively based on number of previous attacks of cholecystitis, WBC count, Gall bladder wall thickness and presence or absence of Pericholecystic collection.