Unusual Morphological Alteration in Sigmoid Notch: An Insight Through CBCT
Anjali Gupta1, Sanchita Kant2, Tushar Phulambrikar3, Manasi Kode4, Siddharth Kumar Singh5
1 Reader, Department of Oral Medicine and Radiology, Sri Aurobindo College of Dentistry, Indore, (M.P.), India.
2 PG Student, Department of Oral Medicine and Radiology, Sri Aurobindo College of Dentistry, Indore, (M.P.), India.
3 Professor and H.O.D., Department of Oral Medicine and Radiology, Sri Aurobindo College of Dentistry, Indore, (M.P.), India.
4 Professor, Department of Oral Medicine and Radiology, Sri Aurobindo College of Dentistry, Indore, (M.P.), India.
5 Reader, Department of Oral Medicine and Radiology, Sri Aurobindo College of Dentistry, Indore, (M.P.), India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanchita Kant, PG Student, Department of Oral Medicine and Radiology, Sri Aurobindo College of Dentistry, Indore, (M.P.), India.
E-mail: sanchitakant@gmail.com
The Temporomandibular Joint (TMJ) is a ginglymo-diarthrodial joint known to be the most complex joint in human body. Growth disturbances, owing to genetic influences or trauma during the intrauterine life or during early developmental age may lead to morphological and functional variations in the mandible resulting in developmental anomaly. We report a rare case of altered sigmoid notch morphology on the right side and condylar hypoplasia on the left side, not related to any clear pathological disorder. Cone Beam Computed Tomography (CBCT) was helpful in evaluating this case. This case of unknown aetiology was thoroughly examined; based on clinical and radiographic findings, we suggest that this case is of congenital origin.
Condylar hypoplasia, Facial malformation, Radiography, Temporomandibular joint
Case Report
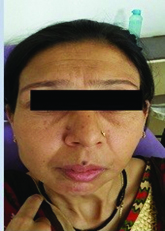
A 35-year-old female reported to the Department of Oral Medicine & Radiology, Sri Aurobindo College of Dentistry, Indore, with the chief complaint of irregularly placed teeth. The irregularity of her teeth had gradually increased over the period of time. Patient gave history of trauma to her chin due to fall from scooter at the age of 10 years. It was not associated with any fracture or bleeding from the involved area. Her family history was negative for any craniofacial abnormalities. On inspection, facial asymmetry was evident [Table/Fig-1].
Clinical photograph of the patient
Extraoral examination revealed hypoplastic right side of the face and deviation of pogonion to the right side. TMJ examination revealed midline shift to right during mouth opening [Table/Fig-2]. The right mandibular condyle was not palpable. No abnormality was detected for rest of the face or auricles. The mouth opening was 18 mm approximately between 11 & 41, which had remained constant with time as long as patient could recollect.
Clinical photograph of the patient during mouth opening

Intraoral examination revealed malaligned anterior teeth with labially displaced 11, 13, 33 and 43. Tooth number 11,12,33 & 43 were in infra-occlusion. Spacing was evident between 21,22 & 21,22,31,32 & 36 were supraerupted. Grade II mobility was observed with 21, 22 along with generalized periodontitis. The lower third molars were missing. Subsequently, provisional diagnosis of Angle’s class II Division 1 malocclusion with generalised periodontitis was made. The differential diagnosis made were trismus secondary to malunion, hypertrophy of coronoid process, tumour of the temporomandibular joint and ankylosis secondary to trauma.
Subsequently an orthopantomogram (OPG) was performed [Table/Fig-3] which revealed horizontally impacted 38 and 48. A radiopacity surrounded by radiolucency was present in relation to periapical region of 38. Also a well defined radiopacity with irregular border was seen at the ramus on the mandibular left side superior to impacted 38. OPG showed flattening of the left condylar head suggestive of toad stool appearance. The sigmoid notch on the right side showed reduced curvature with prominent antegonial notch. Right condylar morphology was altered at the neck with a linear projection from sigmoid notch and altered articular eminence.
Orthopantamogram of the patient

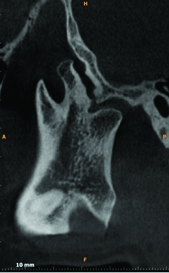
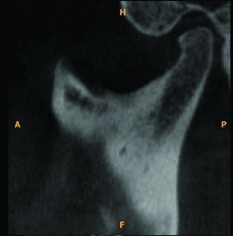
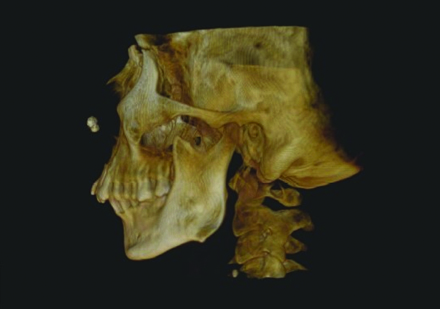
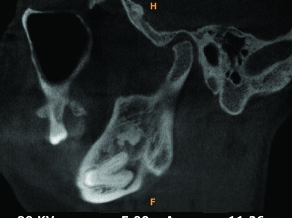
As overlapping of adjacent structures was present at the right TMJ hence, CBCT scan was advised to determine the exact morphology of the right TMJ. The CBCT scan was performed with Kodak CS-9300 using on demand software that provided a 6×6 cm field of view, with 360° rotation. The voxel size was 0.125 cu.mm. The exposure factors were 78 kVp, 17.5-second rotation time, and 3.2 mA. Cone-beam images revealed altered morphology of zygomatic process which was steep on right side measuring approximately 109° with the articular eminence when compared to left side which measured approximately 133° on left side. Also a bony projection was present on right side measuring approximately 16.5 mm from the sigmoid notch extending in anterio-superior direction at a distance of 6.9 mm from coronoid process & 12.1 mm from condyle. The posterior margin of this projection was serrated to reciprocate with the serrated surface of right temporal bone [Table/Fig-4], which was also visualized in the sagittal section [Table/Fig-5].
CBCT scan of the patient revealing altered morphology of right side sigmoid notch in sagittal section
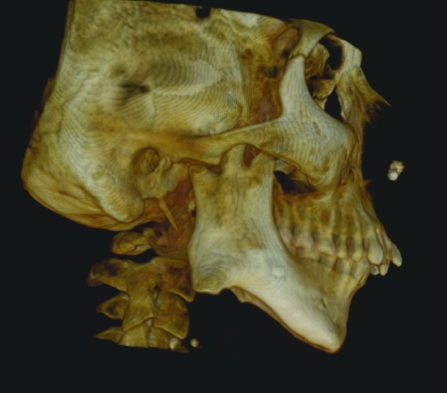
The left condyle measured 19.2 mm mediolaterally [Table/Fig-6,7]. The mediolateral dimesion of right condyle was reduced in size, measuring approximately 16 mm.
CBCT scan of the patient revealing left side sigmoid notch in sagittal section
Thickness of ramus was also different it measured 12.8 mm on left side and the right ramus measured 27.8 mm. An ovoid area of increased radiodensity was observed in ramus on left side superiorly to apex of roots of impacted 38, surrounded by radiolucent capsule [Table/Fig-8] this radiopacity was present at a distance of 1.2 mm from anterior margin of ramus & 11.5 mm from posterior margin measuring 10.3 mm in size.
Sagittal section of left mandibular ramus area demonstrating radiopacity apical to 38
Blood investigations were advised to rule out any bony disorder which revealed a normal serum calcium and alkaline phosphatase level suggesting absence of any bony disorder. Patient was advised for surgical excision of the growth and followed by to Tc- 99m pyrophosphate scan. Patient was also advised for orthognathic surgery for correction of facial deformity followed by orthodontic treatment. However, patient was not willing for any surgical procedure and did not report back to the department.
Discussion
The development of the TMJ mainly occurs after birth with minimal growth during prenatal life. The first evidence of development of TMJ is found at 8th week of gestation, when two separate mesenchymal blastemas appear at the site of future mandibular condyle and glenoid fossa location [1,2]. At birth, thick fibrous connective tissue covers the articular surfaces of the glenoid fossa and the mandibular condyle. With time this tissue is replaced by fibrocartilage and the fossa deepens with the development of mandibular condyle under the influence of functional forces [3]. Growth disturbances, owing to genetic influences or trauma during the intrauterine life or during early developmental age may lead to morphological and functional variations in the mandible resulting in developmental anomaly [1]. The developmental anomalies of the TMJ are classified as aplasia, hypoplasia, hyperplasia and bifidity [4].
The normal morphological appearance of sigmoid notch is S-shaped, concavity, but in our patient there was a bony overgrowth present, masking the concavity of sigmoid notch. Although our patient had a history of trauma, but the CBCT section revealed that condyle was normal at its own position so the projection at the sigmoid notch could have been developmental. Had it been due to displacement of the condyle, the morphology of the mandibular condyle on right side should have been altered. Also, the length of the ramus was normal on right side which is normally affected in cases of condylar trauma or fracture as it being the growth centre. Furthermore, our patient did not have any associated facial malformations suggestive of any syndrome. Condylar hyperplasia is a well-known phenomenon however, sigmoid notch alteration has never been reported in a PUBMED search up till now. Thus it can be concluded that it is a projection from the sigmoid notch in our case, which is developmental in origin & not traumatic being the first case of its kind case reported in history. These modifications may be attributed to the adaptations happening during the growth.
A suitable treatment plan requires an accurate diagnosis. The conventional imaging modalities used to assess the mandible includes various radiological methods like orthopantamogram, lateral & posterior-anterior cephalogram etc., to assess the macroscopic aspects [5]. These modalities assess changes in morphology of mandible however they allow only two-dimesional visualization of the mandible. More recently CBCT has been proposed as promising radiographic technique in the field of TMJ imaging [6,7]. In our case OPG was not able to define the changes at the sigmoid notch, it was the CBCT finding which allowed the visualization of the sigmoid notch alterations. Thus, it signified the role of CBCT in accurate diagnosis of bony morphology.
Conclusion
In conclusion, we report a rare case of altered sigmoid notch morphology on the right side and condylar hypoplasia on the left side, not related to any clear pathological disorder. This case of unknown aetiology was thoroughly examined, based on clinical and radiographic findings; we suggest that this is a case of congenital origin. In this context, our case is an important addition to the literature.
[1]. Carini F, Scardina GA, Caradonna C, Messina P, Valenza V, Human temporomandibular joint morphogenesisItal J Anat Embryol 2007 112(4):267-75. [Google Scholar]
[2]. Ozturk S, Sengezer M, Isik S, Gul D, Zor F, The correction of auricular and mandibular deformities in auriculo-condylar syndromeJ Craniofac Surg 2005 16(3):489-92. [Google Scholar]
[3]. Kaneyama K, Segami N, Hatta T, Congenital deformities and developmental abnormalities of the mandibular condyle in the temporomandibular jointCongenit Anom (Kyoto) 2008 48(3):118-25. [Google Scholar]
[4]. Canger EM, Celenk P, Aplasia of the mandibular condyle associated with some orthopaedic abnormalitiesDentomaxillofac Radiol 2012 41(3):259-63. [Google Scholar]
[5]. Sano T, Otonari-Yamamoto M, Otonari T, Yajima A, Osseous abnormalities related to the temporomandibular jointSemin Ultrasound CT MR 2007 28(3):213-21. [Google Scholar]
[6]. Machado GL, CBCT imaging - A boon to orthodonticsSaudi Dent J 2015 27(1):12-21. [Google Scholar]
[7]. Krishnamoorthy B, Mamatha N, Kumar VA, TMJ imaging by CBCT: Current scenarioAnn Maxillofac Surg 2013 3(1):80-83. [Google Scholar]