In adults, mitral stenosis occurs usually due to a post-rheumatic inflammatory and degenerative disease that fuses the mitral commissures and thickens the chordae. It is one of the most frequently encountered cardiac abnormalities in woman of child-bearing age, accounting for nearly 90% of the cases of rheumatic heart disease associated with pregnancy [2].
Maternal mortality from mitral stenosis is approximately 1%, and rises up to almost 7% in patients with severe impairment [2]. Surgery carries a substantial risk of fetal mortality and morbidity. Valve replacement is associated with high rates of fetal loss (23%) and maternal mortality (2.5%), secondary to complications of coagulation/anticoagulation [2]. Percutaneous balloon valvulotomy is an alternative to surgery and should be considered as a treatment-of-choice in patients with mitral stenosis who remain symptomatic despite adequate medical therapy. The prime aim of current investigation was to evaluate the effectiveness and safety of percutaneous mitral valvulotomy for the treatment of pregnant patients with mitral stenosis.
Materials and Methods
Study design and patient population
We conducted a single-center, prospective study to evaluate the outcomes of percutaneous mitral valvulotomy in pregnant patients with mitral stenosis. Between July 2011 and November 2013, 30 pregnant patients with mitral stenosis underwent balloon mitral valvulotomy (BMV) at our center. BMV was performed in pregnant women with mitral stenosis when they met the following inclusion criteria:
(1) Severe or moderate mitral stenosis with valve area 1.0 cm2 or less with New York Heart Association (NYHA) functional class II, III or IV.
(2) Pliable mitral valve.
(3) Gestational age of 20 weeks after the first trimester of pregnancy.
(4) Absence of more than grade II/IV mitral regurgitation.
(5) Absence of left atrial/left atrial appendage clot.
The patients with more than moderate mitral regurgitation (grade II/IV) at baseline, echocardiographically confirmed presence of left atrial thrombus, severe aortic or tricuspid valve disease that required surgery, recent thromboembolic stroke, acute infection processes, and asymptomatic moderate to severe mitral stenosis were excluded from the study.
All patients underwent detailed transthoracic echocardiographic (TTE) assessment, including 2-dimensional imaging, Doppler studies, and color-flow mapping. The scoring system of Wilkins was used to classify valves into either high or low risk. The suitability of the valve for BMV was assessed by morphology of the mitral valve, presence of calcium in the valve commissures, severity of subvalvar pathology, and presence of mitral regurgitation. Transoesophageal echocardiography (TEE) was performed in patients with atrial fibrillation and in those with a suspicion of left atrial clot on transthoracic echocardiography.
All subjects gave informed consent, and the risk associated with the procedure was explained, including the risks related to radiation exposure to the fetus. The protocol of the study was reviewed and approved by institutional ethics committee (UNMICRC/CARDIO/2013/24). BMV was performed in the fasting state in the catheterization laboratory. To limit fetal radiation exposure, abdominal and pelvic lead shielding of patients was done with lead sheets (thickness 0.5 mm) from the diaphragm to pubic symphysis, and contrast left ventriculography was not performed. Fluoroscopy wasused only when absolutely necessary. The percutaneous Inoue balloon (SYM, Shenzhen Shenyard Medical Device., and Ltd. China) technique was chosen at the discretion of the operator. To reduce the fluoroscopy time we have not measured transmitral gradient and invasive pulmonary artery pressure monitoring on cath study.
Surgical technique and data collection
All BMV procedures were performed under local anaesthesia using the trans-septal, anterograde left-sided cardiac approach. Patients underwent heparinization (100U/kg) after trans-septal puncture. Maximum balloon size possible was determined according to patient’s height. Left atrial pressure was recorded before and after the procedure. Stepwise dilatations of 0.5 mm were done until a successful result was obtained orany evidence of increasing mitral regurgitation.
Echocardiography was performed in the catheterization laboratory to assess the splitting of the commissures. Procedural success was defined as an increase in mitral valve area of 50% over the baseline or a valve area of >1.5 cm2, with no significant increase in mitral regurgitation (>2 grades). Clinical follow-up was accomplished by hospital visits every 3 and 6 months after the procedure until delivery. After BMV, all patients were followed up closely for fetal growth and wellbeing. Clinical and echocardiographic evaluation was performed in all patients at follow-up. After delivery, patients were called for evaluation after 3 and 6 months. The mean follow up time after BMV was 6.73±0.56 months.
Statistical Analysis
All the statistical calculations were carried out using SPSS program version 20.0 (Chicago, IL, USA). Univariate analysis of continuous data which were expressed as Mean±SD was performed using student’s t-test, whereas chi-square test of categorical data which were expressed as frequency and percentage. A p-value <0.05 was considered significant.
Results
The baseline and demographic characteristics of 30 patients with mitral stenosis who underwent BMV during pregnancy are given in [Table/Fig-1]. Average values of age, height and maternal weight of the patients were 24.80±4.34 years (range 21 to 40), 154.07±6.78 cm and 46.83±7.84 kg respectively. Fourteen (46.66%) patients underwent BMV during the third trimester of pregnancy, whereas 16 patients (53.33%) had the procedure performed in the second trimester. Mean gestational age at the time of procedure was 25.3±3.93 weeks. Two of the 30 patients (6.66%) were in NYHA functional class IV, 14 (46.7%) were in III and the remaining 14 (46.66%) were in NYHA functional class II. Nineteen (63.33%) patients had a Wilkin’s score of <8 (considered to have “standard risk” valves), and 11(36.66%) had a score of >8 (“high risk” valves). Nineteen patients (63.33%) were primigravidae and 11 (36.67%) were multigravidas. The mean pulmonary artery pressure was 68.23 ± 23.28 mmHg, and 29 of 30 (96.66%) patients had moderate or severe pulmonary artery hypertension. Of 30 patients, 26 (86.74%) were in normal sinus rhythm, while 4 (13.33%) patients were having atrial fibrillation.
Baseline and demographic details of 30 patients with mitral stenosis who underwent balloon mitral valvulotomy
| Variables | Mean±SD/No. of Patients (%) |
|---|
| Age (Y) | 24.80 ± 4.34 |
| Height (cm) | 154.07 ± 6.78 |
| Weight (kg) | 46.83 ± 7.84 |
| Gestational age at the time of procedure (weeks) | 25.3 ± 3.93 |
| Pulmonary artery pressure (mmHg) | 68.23 ± 23.28 |
| NYHA functional class II | 14 (46.66%) |
| NYHA functional class III | 14 (46.66%) |
| NYHA functional class IV | 2 (6.66%) |
| Wilkin’s score of <8 | 19 (63.33%) |
| Wilkin’s score of >8 | 11 (36.66%) |
| Primigravidae | 19 (63.33%) |
| Multigravida | 11 (36.67%) |
| Patients with normal sinus rhythm | 26 (13.33%) |
| Patients with atrial fibrillation | 4 (86.66%) |
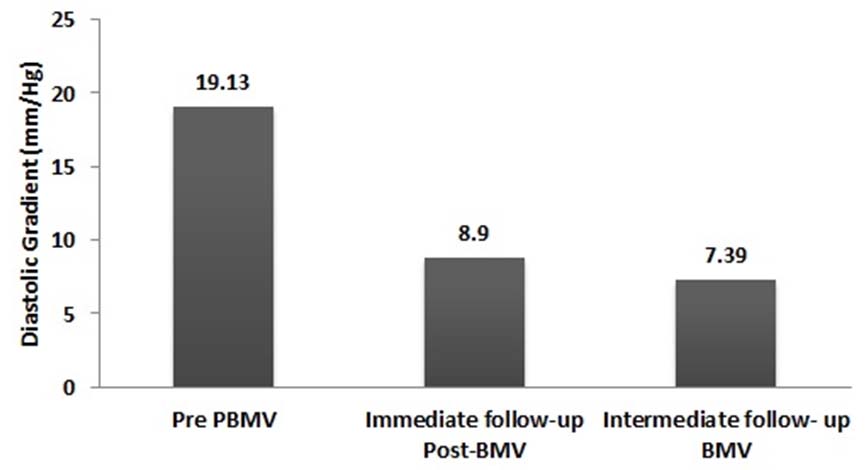
Short-term follow-up information was available in 27 of 30 of the total patient population (90%). Three patients were lost to follow up. The mean follow up duration was 6.72±0.56 months. Follow-up echocardiograms were obtained of 27 patients at a mean follow-up of 6.72±0.56 months. Mean diastolic gradients had decreased significantly after the procedure (p<0.001) but remained very much unchanged at 6-month follow-up compared with post procedure values [Table/Fig-2].
Mean diastolic gradients before and after ballon mitral valvulotomy (BMV) procedure
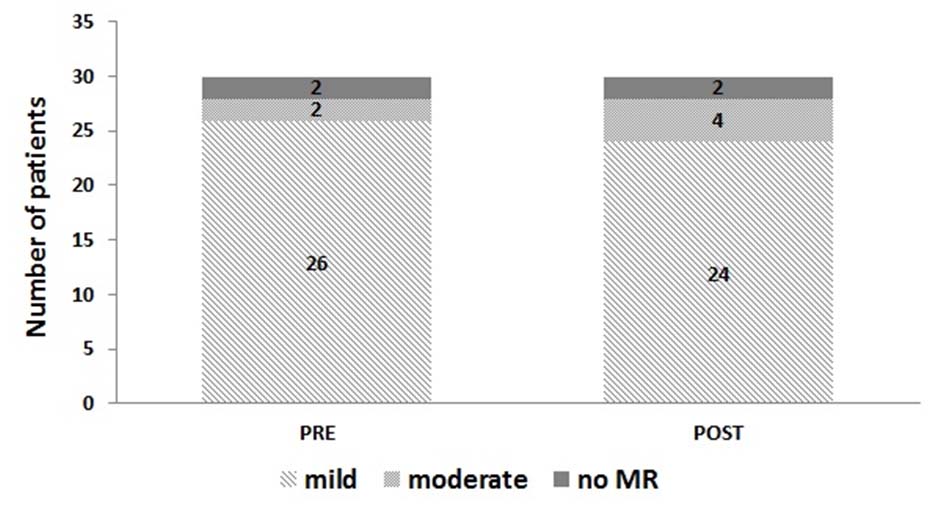
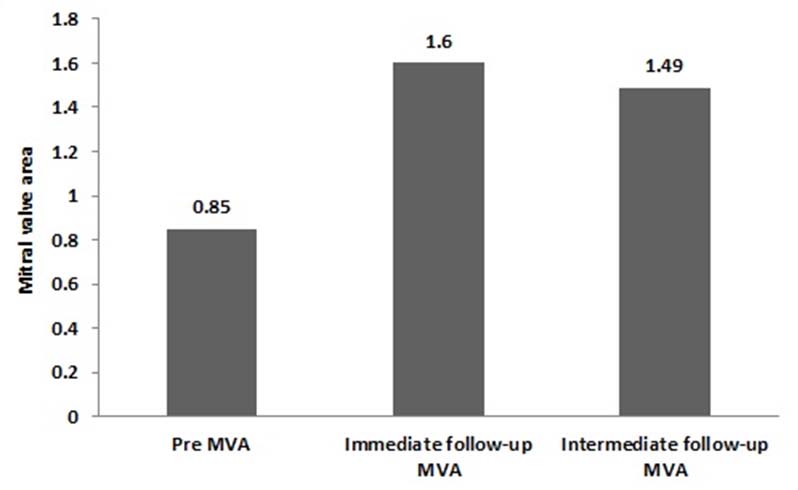
Two patients had an increase in mitral regurgitation by 2 grades [Table/Fig-3]. In one patient, the increase in mitral regurgitation was due to a mild tear in the anterior mitral leaflet close to the medial commissure. In other patient, mitral regurgitation was due to excessive commissural split. The mean mitral valve area was 0.85±0.16 cm2 before BMV and increased to 1.60± 0.27 cm2 (p<0.0001) immediately after BMV [Table/Fig-4]. At about 6-month follow-up, the mean mitral valve area decreased from 1.60 to 1.49.
Status of mitral regurgitation before and after the ballon mitral valvulotomy procedure.
Mitral valve area before and after the ballon mitral valvulotomy (BMV) procedure.
About 83.4% of patients had fluoroscopy time between 2 to 6 minutes, while five (16.66%) patients had fluoroscopy time more than 8 minutes [Table/Fig-5]. The mean fluoroscopy time of the whole group was 3.97 minutes. We did not calculate radiation exposure in any of the patient. Short term follow up information was available in 27 of 30 of the total patient population (90%). Three patients were lost to follow up. The mean follow up duration was 6.72±0.56 months.
Analysis of fluoroscopy time.
| Fluoroscopy time (min) | No. of patients (%) |
|---|
| <2 | 01 (3.33%) |
| 2-4 | 12 (40.0%) |
| 4-6 | 12 (40.0%) |
| 6-8 | 05 (16.66%) |
There were no abortions, still births or neonatal deaths. Mean birth weight was 2.52± 0.35 kg (range: 1.25 to 3.25). Seven (23.33%) babies were having birth weight less than 2.5 kg. Intermediate-term follow up data were available for 27 children (90%) with mean follow up duration of 6.72±0.56 months. There were no clinically evident congenital malformations in any of the patients. All children had normal mental development with normal development milestones.
Discussion
Our data are comparable to other reports of BMV in pregnancy [3–14]. Nercolini et al., obtained a success rate of 95%, which was defined by increase in final mitral valve area >1.5 cm2 [4]. Farhat et al., showed no technical failure in all 44 pregnant patients with 100% success rate [8]. In our study, mitral valve area increased significantly from 0.85± 0.16 cm2 to 1.60±0.27cm2. Further, the pre-procedure mitral valve area as were comparable to most reports from India [3,7,9].
Two patients in our series had increases in mitral regurgitation by 2 grades (6.66%); one patient had a mild tear in the anterior mitral leaflet close to the medial commissure. Other had mitral regurgitation due to split of commissural. Other investigators also reported severe mitral regurgitation in the range of 1.1% to 9.1%. In our study, all the patients had symptomatic improvement as assessed by NYHA class except one patient who required emergency surgery because of severe mitral regurgitation. The excellent symptomatic improvement after BMV in pregnancy has also been reported by other authors [7–10].
The Inoue balloon technique seems to shorten the fluoroscopy time and therefore appears to be very attractive in this particular setting. The fluoroscopy time in old series was relatively higher than recent studies. Ribeiro et al., reported mean fluoroscopy time of 16±14 minutes in 17 pregnant patients [15]. Patel et al., reported a shorter fluoroscopy time without measurement of invasive haemodynamic [16]. The fluoroscopy time was 9.2±3.4 minutes in our patients. In recent case series from south India by Sivadasan pillai, et al, the mean fluoroscopy time was 5.4±5.8 minutes (range 1.8 to 29). This was similar to our study [14].
Although the amount of radiation exposure was not measured in our series, some studies have measured very low amount of radiation exposure (0.1-0.5mSv), far lower than that legally admitted for pregnant women subject to radiation exposure (i.e., 5 mSv) [17,18]. It is noteworthy that the 27 infants in this study had normal growth and mental development at an intermediate follow-up of 6 months. Other reports have also shown normal long-term effects of balloon mitral valvoplasty [14,19]. All children were found to have maintained normal growth development, and speech on follow up. There were no reports of maternal death and vascular complication in our study. Similarly there is no procedure related to mortality reported to any of the series [3,14].
All patients in our study had persistent relief of symptoms, although there was a gradual reduction in mitral valve area at follow-up. The mean mitral valve area was 1.49±0.23 cm2 at follow-up compared with the post procedure valve area of 1.60±0.26 cm2 (p<0.05). However, the loss in mitral valve area did not translate into symptomatic deterioration, because NYHA class remained almost the same at follow-up. In similar context, Mangione et al followed 30 patients for a period of 5.33±3.12 years and found that mitral valve area decreased significantly from 2.01±0.21 to 1.75±0.24 cm2 [6]. They also noted an absence of symptomatic deterioration. There was no significant reduction in mitral valve area on follow-up in our study, which could be explained by short duration of mean follow up of 6.72±0.56 months.
Conclusion
We can conclude that during pregnancy BMV technique is safe and effective in patients with severe mitral stenosis. This results in marked symptomatic relief along with long term maternal and fetal outcomes.