Nearly all studies analysing thrombocytopaenia as a prognostic marker in ICU patients found an inverse correlation of the platelet count with the risks for a prolonged ICU stay and mortality (mortality rate 31%–46% in thrombocytopaenic patients vs 16%–20% nonthrombocytopaenic patients) [4].
Prolonged and sustained thrombocytopaenia over more than 4 days after ICU admission or a drop in platelet count of >50% during ICU stay is related to a 4 to 6 fold increase in mortality [5].
Platelet transfusions are done to increase the platelet counts but the response to transfusions varies from patient to patient and severity of disease. Few studies have been done to know the prevalence of thrombocytopaenia in ICU and the need for transfusion and response to this transfusion [6]. There is not much data available from developing country like India and no such study has been done in Punjab region of the country.
Present study was conducted at a tertiary care teaching hospital in India to know about the incidence of thrombocytopaenia and relationship with mortality in PICU. Various disease conditions which were associated with thrombocytopaenia were found out and the number of transfusions and rise in platelet counts was calculated.
Materials and Methods
Eleven months records, between October 2013 and August 2014, was screened retrospectively and 275 children (168 boys and 107 girls) in Paediatric Intensive Care Unit (PICU) were included in the study. Besides patient’s demography, source of admission, primary diagnosis, presence or absence of sepsis, bleeding, use of central venous or arterial lines and mechanical ventilation were recorded. Laboratory data collected at admission i.e. Complete Blood Counts (CBC), C- Reactive Protein (CRP), Blood Urea Nitrogen (BUN), serum creatinine, serum bilirubin and coagulation profile was recorded. Daily platelet counts were also recorded in each patient.
Thrombocytopaenia was defined as platelet count below 150x109/L. The severity of thrombocytopaenia was classified as mild (platelet count 100 x 109 to 149 x 109 per L), moderate (platelet count 50 to 99 x 109 per L), severe (platelet count < 50 x 109 per L) and very severe (platelet count < 20 x 109 per L) [7]. Sepsis was defined in patients with documented infection in presence of positive acute phase reactants and raised Total Leukocyte Counts (TLC). Coagulopathy was defined when the Activated Partial Thromboplastin Time (aPTT) was 1.5 times the normal reference range for the laboratory with an associated increase in International Normalised Ratio (INR) more than 1.5. Bleeding was defined as an episode resulting from a drop in Haemoglobin of >2 g/dL within 24 hours, episodes requiring transfusions and any intracranial haemorrhage.
Statistical Analysis
The risk of thrombocytopaenia in a disease and mortality due to thrombocytopaenia was determined by calculating an odds ratio with 95% confidence interval. Any independent risk factor with probability value (p-value) of less than 0.05 was considered statistically significant. Results were also confirmed using χ2 test.
Results
Out of 275 patients [Table/Fig-1], 89 patients had thrombocytopaenia incidence of 32.4%. Male to Female ratio was 1.57:1, {168 boys(61.09%) and 107 girls(38.91%)}, Age range of patients was 1 month to 13 years (156 months) with Mean ± SD (39.278± 44.125 months). The source of admission was mainly from Paediatric wards (46.54%), emergency department (45.45%) Surgical wards (4.36%) and Operation theatre (3.64%). Sepsis was the most common cause (20.36%) for admission while the other causes were Pneumonia (14.91%), Meningitis (10.54%), Diabetic Ketoacidosis (8.36%), Enteric fever (7.27%), Tubercular Meningitis (4%), Infantile Tremor Syndrome (3.27%), Congenital heart disease (4%), Burns (1.82%), Brain Haemorrhage (0.73%), Hepatic abscess (0.73%), Renal (3.27%), Malaria (3.27%), Hepatitis (3.64%), Others (13.82%).
Clinical features of patients in Paediatric Intensive Care Unit (n=275)
| Parameters | Total |
|---|
| Gender (M:F) | 1.57:1,{168 boys (61.09%) and 107 girls(38.91%)} |
| Age | 39.278±44.125 months |
| Admission | |
| Paediatric ward | 128 (46.54%) |
| Surgical ward | 10(4.36%) |
| Operation theatre | 12(3.64%) |
| Emergency | 125(45.45%) |
| Platelet count | |
| 100 to 149 x 109 per L | 22(24.72%) |
| 50 to 99 x 109 per L | 24(27.91%) |
| < 50 x 109 per L | 43 (48.31%) |
| Diagnosis | |
| Sepsis | 56(20.36%) |
| Pneumonia | 41(14.91%) |
| Meningitis | 29(10.54%) |
| DKA | 23(8.36%) |
| Enteric fever | 20(7.27%) |
| TBM | 11(4%) |
| ITS | 9(3.27%) |
| Congenital heart disease | 11(4%) |
| Burns | 5(1.82%) |
| Brain Haemorrhage | 2(0.73%) |
| Hepatic abscess | 2(0.73%) |
| Renal | 9(3.27%) |
| Malaria | 9(3.27%) |
| Hepatitis | 10(3.64%) |
| Others | 38(13.82%) |
| Platelet transfusion | 43(15.64%) |
| Mortality | 54(19.64%) |
Out of these 89 patients, 43 patients (48.31%) had platelet count of less than 50 x 109 per L, 24 had platelet count between 50 to 99 x 109 per L (27.91%), and 22 patients had platelet count between 100 to 149 x 109 per L (24.72%). Total of 43 patients having platelet count of less than 50 x 109 per L received platelet transfusion. These 43 patients were transfused 103 units of Platelets (median number of units per patient was 2, maximum being 10). Platelet dose was approximately 5.5 to 8.5 x 1010 per transfusion. Average rise in platelets was 30.581×103±12.92×103.
Among thrombocytopaenic patients [Table/Fig-2], Sepsis (25.84% vs 17.74% non-thrombocytopaenic patients) was the most common diagnosis while other thrombocytopaenic patients had Pneumonia (19.10%), Meningitis (13.48%), DKA (5.62%), Enteric fever (7.86%), Tubercular Meningitis (3.37%), Infantile Tremor Syndrome (2.25%), Congenital heart disease (5.62%), Burns (3.37%), Brain Haemorrhage (2.25%%), Hepatic abscess (1.12%), Chronic Renal Failure (3.37%), Malaria (2.25%) and Hepatitis (4.49%). There is a statistically significant association between throm bocytopaenia and mortality [Table/Fig-3] {29.21% vs 15.05%in non- thrombocytopaenic patients Odd’s Ratio 2.3288(1.2673-4.2795), χ2 =7.65 p-value=0.0053}.
Diseases in thrombocytopaenic vs nonthrombocytopaenic
| Disease | Throm-bocyto-paenic(n=89) | Percent-age (%) | Non-throm-bocyto-paenic(n=186) | Percent-age(%) | ODD Ratio (95% CI) | p- value |
|---|
| Sepsis | 23 | 25.84 | 33 | 17.74 | 1.6157(0.8818-2.9605) | 0.08 |
| Pneumonia | 17 | 19.10 | 24 | 12.90 | 1.5938(0.807-3.1475) | 0.122 |
| Meningitis | 12 | 13.48 | 17 | 9.14 | 1.5493(0.7055-3.4021) | 0.186 |
| DKA(Diabetic ketoacidosis) | 5 | 5.62 | 18 | 9.67 | 0.5556(0.1994-1.5482) | 0.184 |
| Enteric fever | 7 | 7.86 | 13 | 6.99 | 1.136(0.4368-2.9542) | 0.4844 |
| TBM(Tubercular Meningitis) | 3 | 3.37 | 08 | 4.30 | 0.7762(0.2009-2.999) | 0.499 |
| ITS(Infantile tremor syndrome) | 2 | 2.25 | 07 | 3.76 | 0.5878(0.1196-2.8891) | 0.3986 |
| Congenital heart disease | 5 | 5.62 | 06 | 3.22 | 1.7857(0.53-6.017) | 0.2616 |
| Burns | 3 | 3.37 | 02 | 1.07 | 3.2093(0.5266-19.5604) | 0.1938 |
| Brain Haemorrhage | 2 | 2.25 | 0 | 0 | ∞ | 0.1039 |
| Hepatic abscess | 1 | 1.12 | 01 | 0.53 | 2.1023(0.13-34.033) | 0.5433 |
| Renal | 3 | 3.37 | 06 | 3.22 | 1.0465(0.2556-4.2845) | 0.6014 |
| Malaria | 2 | 2.25 | 07 | 3.76 | 0.5878(0.1196-2.8891) | 0.3986 |
| Hepatitis | 4 | 4.49 | 06 | 3.22 | 1.4118(0.3882-5.1348) | 0.4138 |
| Others | 0 | 0 | 38 | 14.51 | 0 | 0.0001 |
Mortality in various diseases thrombocytopaenic (26) vs non thrombocytopaenic (28)
| Disease | Throm-bocyto-paenic | Percent-age (%) | Non-throm-bocyto-paenic | Percent-age(%) | OR with 95%CI | p- value |
|---|
| Sepsis | 14(23) | 53.85 | 09(33) | 32.143 | 4.1481(1.333- 12.9052) | 0.012 |
| Pneumonia | 03(17) | 11.53 | 06(24) | 21.428 | 0.6429(0.1362-3.0348) | 0.435 |
| Meningitis | 02(12) | 7.69 | 03(17) | 10.714 | 0.9333(0.1309-6.657) | 0.67 |
| DKA | 01(15) | 3.85 | 02(18) | 7.143 | 2 (0.1429-27.99) | 0.539 |
| Enteric fever | 02(07) | 7.69 | 02(13) | 7.143 | 2.2(0.2373-20.3967) | 0.439 |
| TBM | 02(03) | 7.69 | 02(08) | 7.143 | 6.0(0.3351-107.4259) | 0.2787 |
| ITS | 01(02) | 3.85 | 02(07) | 7.143 | 2.5 (0.0998-62.6084) | 0.583 |
| Congenital heart disease | 01(05) | 3.85 | 02(06) | 7.143 | 0.5 (0.0313-7.9942) | 0.5757 |
| All diseases | 26 | 100 | 28 | 100 | 2.3288(1.2673-4.2795) | 0.0053 |
* The no. of patients in bracket is the total number of patients suffering from the disease mentioned in column 1
A significant association was established between mortality in thrombocytopaenic patients of sepsis {OR 4.1481(1.333- 12.9052) p-value 0.012} [Table/Fig-3,4].
Mortality in thrombocytopaenic patients vs non thrombocytopaenic patients
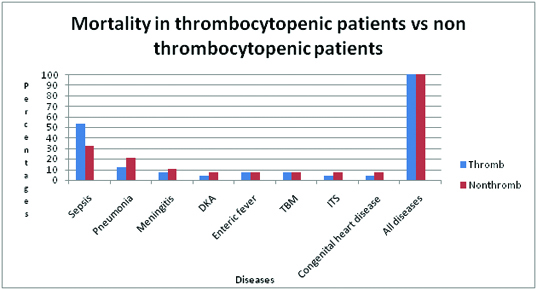
No statistically significant association was found between thrombocytopaenia and mortality in Pneumonia, Meningitis, DKA, Enteric fever, Tubercular Meningitis, Infantile Tremor Syndrome, Congenital heart disease, Burns, Brain Haemorrhage, Hepatic abscess, Chronic Renal Failure, Malaria, Hepatitis as number of patients per each disease is very less.
Discussion
The incidence of thrombocytopaenia and relationship between thrombocytopaenia on admission in PICU and mortality in critically ill patients was analysed in this study. The age range of our patients was 39.278±44.125 months which is comparable to other studies [2,3,8]. In our study the source of admission was from Paediatric wards (46.54%), Emergency department (45.45%), Surgical wards (4.36%), Operation theatre (3.64%) and which is comparable to the study by Yilmaz et al., where admissions were mainly from hospital wards (70.2%) [2], Emergency Department (26.6%) and Operation room (3.2%) while the study by Agarwal et al., had main source of admission from Emergency Room 79.7% [3].
The reason for difference in source of admission in our study may be because in our institution emergency patients are shifted to paediatric ward directly if the bed is not available in PICU.
In our study incidence of thrombocytopaenia was 32.4% (89) which is lower than study by Mussa et al., and Yilmaz et al., where it was 44.61% and 59.57% respectively while it was slightly higher than study by Agarwal et al., where incidence was 25% [2,3,8]. This difference in incidence may be because other studies were prospective and patients were monitored for longer duration of time.
Incidence of moderate thrombocytopaenia (platelet count 50 to 99 x 109 per L) in our study was 27.91% which is comparable to other studies [2,3,8].
Mortality in thrombocytopaenic patients was higher (29.21% vs 15.05%) and statistically significant {OR 2.3288 (1.2673-4.2795), χ2 =7.65 p-value=0.0053} which is in consonance with other studies [2,9].
Mortality was significantly higher in thrombocytopaenic septic patients {(53.85% vs 32.143% in non thrombocytopaenic patients OR 4.1481(1.333-12.9052) p-value 0.012} which is comparable to other studies [2,3,8].
The reason for more mortality in Septic patients may be because of Multiple Organ Dysfunction (MODS) as MODS criteria for hematologic dysfunction is thrombocytopaenia i.e. platelet count < 80,000/mm3 or decline of 50% in the platelet count from the highest value recorded over the last 3 days. We could not find any statistically significant relation between mortality and thrombocytopaenic patients with Pneumonia, Meningitis, DKA, Enteric fever, Congenital heart disease, TBM and ITS as number of patients in these groups is very less. From this study it can be inferred that thrombocytopaenia can be used as an independent predictor of overall mortality in PICU especially in cases of thrombocytopaenic septic patients. Only one study in PICU and few studies in NICU have been done in India but none has been done in this region of the country [3,9,10].
Limitation
The limitations of this study are that it includes small number of patients in certain groups and it does not allow great precision in the estimation of odds ratio and we may have missed some important risk factors. So the results need to be validated in a larger cohort.
Conclusions
From this study it can be concluded that mortality rate is higher in thrombocytopaenic patients and among the thrombocytopaenic patients, Sepsis is the most common diagnosis.
* The no. of patients in bracket is the total number of patients suffering from the disease mentioned in column 1