Postoperative pain is one of the main concerns for the patient undergoing major surgery. It is a challenge to the treating surgeon and attending anaesthesiologist as there are many adverse physiological and psychological effects associated with pain, which can hamper the normal recovery process. Various techniques and drugs have been used for this purpose with variable success. Every technique and drugs has its own advantages and disadvantages.
Transdermal drug delivery systems are simple, non-invasive and compliant method of delivery. They are designed to provide sustained drug release for prolonged period. They are available for analgesics like opioid (fentanyl and buprenorphine) and NSAIDS (diclofenac), antihypertensive like NTG, hormones (estrogen, testosterone), anticholinergics (scopolamine), clonidine, rivastigmine, MAOI selegiline, methylphenidate, cynocobalamine, nicotine etc [1].
Opioid are one of the most commonly used analgesics for postoperative pain and their transdermal patches provide sustained blood levels of the drug for sufficient period. We compared two available opioid transdermal patch for postoperative pain relief in major abdominal surgeries.
Materials and Methods
It was a prospective randomized double blind comparative study involving 60 adult patients undergoing major abdominal surgery under general anaesthesia (GA). Patients of age 20-50 years, undergoing major abdominal surgeries under GA and willing to participate in the study were enrolled. Patients allergic to study drugs, having intolerance to opioid, pregnant and breastfeeding females and having impaired pulmonary function were excluded from the study.
After getting approval from the institutional ethical committee (human), patients were divided into 2 groups randomly. Each group had 30 patients (n=30).
Group A: This group received Buprenorphine patch (10 μg/h), on hairless area of chest, back, flank and upper arm.
Group B: This group received Fentanyl patch of (25 μg/h), on hairless area of chest, back, flank and upper arm.
Drug patches were applied to patients 6 hours before proposed surgery in both groups after noting baseline haemodynamic parameters. At the time of surgery patients were premedicated with inj. Midazolam 1 mg IV, inj. Fentanyl 2 mcg/kg IV and inj ondensetron 4 mg IV. Patients were induced with propofol 2 mg/kg and intubated with vecuronium 0.1 mg/kg. Anaesthesia was maintained with N2O and O2 (60:40), isoflurane and muscle relaxation was maintained with vecuronium. Patients were extubated after reversing neuromuscular blockade with glycopyrrolate and neostigmine (0.01 mg/kg and 0.05 mg/kg respectively).
Sedation and analgesia was assessed using Ramsay sedation scale and visual analogue score respectively for the next 3 days 12 hourly. Haemodynamic parameters and any adverse effects were also noted. Inj diclofenac (75 mg IV) was used as a rescue analgesic in patient complaining of inadequate pain relief.
Statistical Analysis
Power and sample size analysis showed that we need to take minimum of 25 patients in each group to detect statistically significant differences between two groups by keeping α= 0.05 and power of study 95%. The population was divided into two groups. The Observations were compared statistically using student t-test /Fischer-exact test.
Results
The baseline characteristics of the patients are given in the [Table/Fig-1]. The age of both the groups was almost similar and male/female ratio was also similar. Thus, both the groups were comparable in terms of age and sex. The systolic blood pressure (SBP), diastolic blood pressure (DBP), visual analogue scale (VAS) and Ramsay sedation score (RSS) were insignificantly different at Day 1.
Baseline characteristics of the patients
| Characteristics | Group A(n=30) | Group B(n=30) | p-value |
|---|
| Age in years | 39.87±7.41 | 38.80±9.04 | 0.61 |
| Male gender, no. (%) | 22 (73.3) | 24 (80.0) | 0.54 |
| SBP | 136.12±4.68 | 134.11±3.75 | 0.09 |
| DBP | 80.56±3.67 | 81.75±3.46 | 0.20 |
| Heart rate | 81.06±5.12 | 81.11±4.35 | 0.96 |
| VAS | 4.47±0.38 | 4.48±0.61 | 0.94 |
| Sedation score | 1.57±0.47 | 1.41±0.46 | 0.19 |
[Table/Fig-2] depicts the mean values of VAS from Day 1 to Day 3 in both groups. The mean level of VAS was significantly lower in group B as compared to group A at Day 1, 2 and 3.
Change in VAS from Day 1 to Day 3
| Follow-up day | Group A(n=30) | Group B(n=30) | p-value |
|---|
| Day 1 | 4.47±0.38 | 2.48±0.61 | <0.0001* |
| Day 2 | 4.45±0.36 | 3.21±0.60 | <0.0001* |
| Day 3 | 4.37±0.58 | 3.91±0.51 | 0.002* |
*Significant
[Table/Fig-3] depicts the mean values of sedation score from Day 1 to Day 3 in both groups. The mean level of sedation score was significantly lower in Group B than Group A.
Change in Sedation score from Day 1 to Day 3
| Follow-up day | Group A(n=30) | Group B(n=30) | p-value |
|---|
| Day 1 | 1.86±0.47 | 1.40±0.46 | 0.0003* |
| Day 2 | 1.78±0.31 | 1.45±0.47 | 0.0022* |
| Day 3 | 1.87±0.28 | 1.43±0.19 | <0.0001* |
*Significant
Haemodynamic variables in both groups (SBP, DBP and HR), shows comparable values in both groups and no significant difference was observed.
The incidence of adverse effects is shown in [Table/Fig-4]. The incidence of nausea, urinary retention and constipation were comparable in both groups (p-value= 1.0000). The total no. of adverse events in both groups did not differ significantly (p-value= 1.0000). None of the patient in both group experienced skin irritation and respiratory depression.
Percentage of patients requiring rescue analgesics with mean dose of rescue analgesic
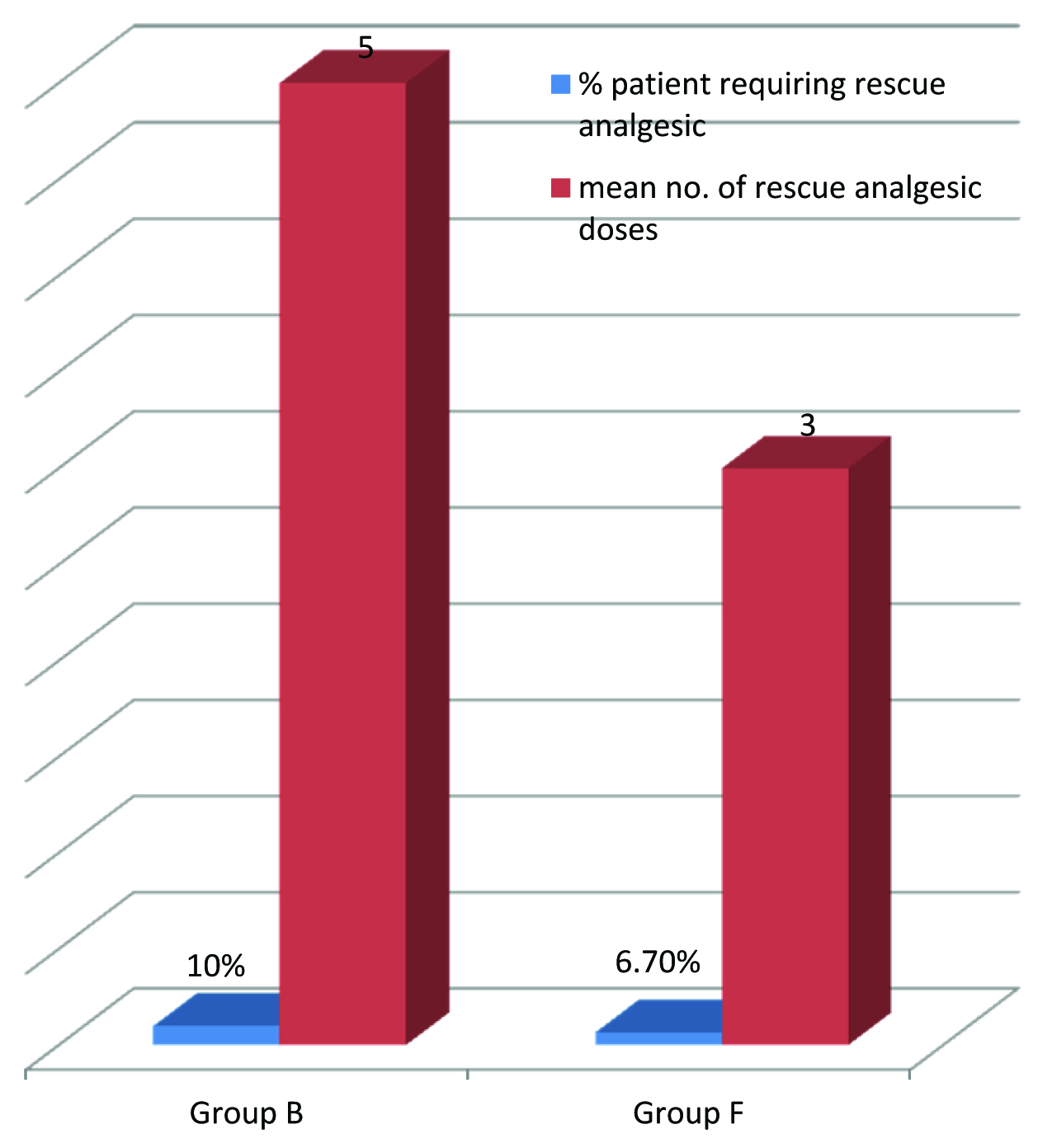
Five out of 30 (16.7%) patients in group A required single dose of rescue analgesic while 0 out of 30 patients (0.00%) in group B required rescue analgesic as shown in [Table/Fig-4]. This difference in rescue analgesic requirement is not quiet statistically significant (p-value 0.0522).
Discussion
Transdermal drug delivery system (TDS) provides safe, convenient and sustained method of drug delivery. It is a preferable alternative to parentral and oral drug delivery methods as it avoids painful skin punctures and multiple dosing. TDS allows sustained delivery of drug to plasma without first pass metabolism. Many drugs which have a high first pass metabolism are given through TDS such as Buprenorphine, Clonidine, Estradiol, Fentanyl, Granisetron, Lidocaine, Methylphenidate, Nicotine, Nitroglycerin, Oxybutynin, Rivastigmine, Rotigotine, Scopolamine, Selegiline, Testosterone, Influenza virus vaccine, etc [1]. TDS allow continuous drug delivery and sustained plasma levels thereby avoiding peaks and turphs in the plasma levels of the drug. It also decreases the incidence of breakthrough pain by providing sustained pain relief and thereby decreasing the requirement of rescue analgesics. Due to slow release of drug and avoiding sudden peaks in plasma drug levels, TDS also decreases the incidence of adverse effects associated with drugs. However, not all side effects are decreased as shown in some studies that the gastrointestinal side effects associated with oral and transdermal opioids are comparable [2].
TDS are not extensively used to control postoperative pain due to their slower onset (6-24 hours), unpredictable absorption especially during hypothermia as seen in postoperative period, interpatient variability, high cost, availability of limited number of drugs and physician’s familiarity with injectable analgesics. But with newer TDS many of the above problems are attenuated.
Fentanyl is a synthetic opioid with potent analgesic activity. Fentanyl has low molecular weight and high lipid solubility therefore it is suitable for delivery via the transdermal therapeutic system (TTS). These systems provide drug at constant rate ranging from 25 to 100 micrograms/h [1]. However, risk of respiratory depression makes fentanyl TTS relatively contraindicated in this setting. At the start of fentanyl TTS treatment, drug first accumulates within skin tissue and then gradually released in systemic circulation which results in a significant delay (17 to 48 hours) before maximum plasma concentration is achieved. The duration of onset of analgesia is noted to be 1.2 to 40 hours and peak effect reaches to 1.2 to 40 hours. Analgesia lasts upto three days [3]. The adverse events of fentanyl TTS therapy (as with other opioid agents) nausea (36.0%), somnolence (30.2%), vomiting (25.6%), diarrhoea (19.8%), constipation (16.3%), pyrexia (12.8%) and insomnia (10.5%). and respiratory depression (4%) [4].
Slow onset and large patient to patient variability of TTS fentanyl, along with the relatively short duration of analgesia and a high incidence of respiratory depression made anaesthesiologist reluctant to use it for acute postoperative pain. In comparison with oral morphine, TTS fentanyl causes fewer gastrointestinal adverse events [3].
Buprenorphine is a semi-synthetic opioid analgesic. It is a partial agonist at the mu opioid receptor. TDS provides pain relief for one week [5]. Ceiling effect to analgesia was not seen within the therapeutic dose range. Buprenorphine can be used with full mu-agonists without fear of antagonism. Buprenorphine has no immunosuppressant activity at analgesic concentration as seen with fentanyl and morphine. Unlike morphine and fentanyl, there is no immunosuppressive activity with buprenorphine at therapeutic analgesic doses [6]. Systemic adverse effects included nausea, vomiting and constipation. Local adverse events are erythema and pruritis. The new buprenorphine TDS appears to be an important new modality for administering analgesia in patients with non-acute pain [7,8].
The high efficacy, tolerability and patient compliance of both buprenorphine and fentanyl make both these two opioid valid therapeutic options for the treatment of neuropathic pain in patients with AIDS [3].
In our study, we compared the two opioid TDS in postsurgical patients for 3 days to determine their safety and efficacy, as from the above discussion we can see that fentanyl TDS is considered relatively contraindicated in postsurgical patients. The haemodynamic variables in both groups were comparable and did not show any clinically significant deviation from the baseline values. Although, there are isolated case reports of bradycardia with the use of fentanyl TDS, we did not found any adverse haemodynamic events in our study in either group [9].
The VAS scores, which were used to quantify the pain, were significantly reduced from day 1 to 3 in group B as compared to group A. On comparing with the baseline values, we found that the VAS was not significantly reduced in group A and it seems that buprenorphine TDS is not effective in decreasing pain but we must keep in mind that buprenorphine TDS has not allowed VAS to increase after surgery which normally happens. Thus we can see that buprenorphine TDS is effective in attenuating postsurgical pain. While in group B, VAS is significantly decreased from the baseline and also it is significantly lower than group A from day 1 to 3, suggesting that fentanyl TDS is more effective in controlling postsurgical pain. Therefore, we can conclude that both TDS were effective in controlling postoperative pain. However, fentanyl was better in this regard. Five patients in group A required single dose of rescue analgesic within first 4 hours after surgery and no further rescue analgesic was required. While in group B, no rescue analgesic was required. This further consolidates our conclusion that fentanyl TDS is better analgesic than buprenorphine TDS. Buprenorphine TDS has manufacturer recommended duration of action of 7 days while fentanyl TDS has duration of action of 72 hours. Therefore, buprenorphine TDS provides longer pain relief as compared to fentanyl TDS but the latter is more effective analgesic.
Although sedation scores were significantly higher in group A as compared to group B on Statistical analysis but they were below 2 throughout the treatment period. All patients were calm, comfortable and easily aruosable throughout the study and none of the patient showed excessive sedation or respiratory depression. On comparing with the baseline sedation scores, we found that sedation scores were not changed in group B as compared to baseline but they are higher in group A. So, we conclude that buprenorphine TDS provides more sedation than fentanyl TDS but this difference is not clinically significant.
Twenty percent patient in fentanyl group and 16.7% patients in buprenorphine group experienced some adverse effects. Nausea and vomiting were main side effects of the drugs. The incidence of nausea and vomiting were 6.7% and 10% in buprenorphine and fentanyl group respectively which was significantly lower than observed in other studies [4,6]. Besides opioid, many other factors may lead to nausea and vomiting such as female sex and abdominal surgery. Thus, the genesis of nausea was multifactorial. Other adverse effects included constipation and urinary retention which were known adverse effects of opioid. TDS has same adverse effects as seen with other routes and they are easily manageable [8]. Transdermal buprenorphine has ceiling effect on respiratory depression. Adverse events seen with transdermal buprenorphine are headache, dizziness, somnolence, constipation, dry mouth, nausea, vomiting, pruritis, erythema, and application site pruritis and application site reactions. Transdermal buprenorphine has generally proved safe and effective in clinical trials in chronic non-malignant pain. The convenience of once-weekly administration and no need for dosage adjustments in the elderly or those with compromised renal function are additional benefits.
None of the patient in our study suffered allergic reaction or skin irritation to the drug patch; however these problems were noted in other studies [10,11,12].
Buprenorphine TDS was also shown to be an effective analgesic against chronic, severe pain in this study population. Patients treated with this new formulation of buprenorphine showed improved duration of sleep and reduced need for additional oral analgesics [13]. Our study proved its usefulness in postoperative pain also.
Fentanyl TDS is not extensively studied in postsurgical patient due to fear of respiratory depression. However, it has been used in cancer and chronic pain [14,15]. In our study, we showed that it is not as serious problem as thought. The use of fentanyl TDS in suitable patient is as safe and effective as other opioid.
Considering the cost of the transdermal patches, fentanyl patch is available at INR 1450 (Duragesic TM 25 mcg) while buprenorphine patch is available at INR 890 (Buvlor TM 10 mcg). Fentanyl TDS works for 3 days while buprenorphine TDS works for 7 days. So, buprenorphine TDS is cheaper than fentanyl TDS.
Limitations
The limitations of our study includes comparison in lower abdominal surgery only, use of subjective VAS scale for analgesia, follow up only for 3 days and not measuring plasma levels of drug.
Conclusion
Thus, we can conclude that both buprenorphine and fentanyl TDS were effective in controlling postsurgical pain and fentanyl is better in this regard. Because fentanyl TDS has better analgesia with less sedation. However, on considering cost effectiveness, buprenorphine TDS is better as it is cheaper and can be used for 7 days. So, we recommend both TDS for postoperative analgesia. Buprenorphine is more cost effective and of longer duration and should be preferred. However, if greater analgesia is required then fentanyl TDS is better.
*Significant
*Significant