Mucoepidermoid Carcinoma of Floor of the Mouth – A Rarity
Aruna Kumari Maloth1, S.R.K. Nandan2, Pavan G Kulkarni3, Shyam Prasad Reddy Dorankula4, Keerthi Muddana5
1 Senior Lecturer, Department of Oral Pathology, Kamineni Institute of Dental Sciences, Nalgonda, Telangana, India.
2 Professor and Head, Department of Oral Pathology, Kamineni Institute of Dental Sciences, Nalgonda, Telangana, India.
3 Reader, Department of Oral Pathology, Kamineni Institute of Dental Sciences, Nalgonda, Telangana, India.
4 Reader, Department of Oral Pathology, Kamineni Institute of Dental Sciences, Nalgonda, Telangana, India.
5 Senior Lecturer, Department of Oral Pathology, Kamineni Institute of Dental Sciences, Nalgonda, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aruna Kumari Maloth, Senior Lecturer, Department of Oral Pathology, Kamineni Institute of Dental Sciences, Nalgonda-508254, Telangana, India.
E-mail: dr.arunaopath@gmail.com
Mucoepidermoid Carcinoma (MEC) is one of the most commonly occurring malignant salivary gland neoplasm, and contributes 2.8%–15% of all salivary gland tumours. More than half of these cases involve the major salivary glands, primarily the parotid glands and minor salivary glands. Sublingual salivary glands neoplasms are very rare and constitute 0.5% and 1% of all epithelial salivary tumours and approximately 1.5% of the major salivary glands carcinomas. Here we describe a case report of low grade mucoepidermoid carcinoma in the floor of the mouth in a 70-year-old female patient that was mimicking like a ranula clinically.
Malignant salivary gland tumour, Ranula
Case Report
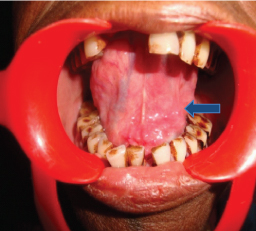
A 70-year-old female patient reported to the Department of Oral Medicine and Radiology with the chief complaint of pain and swelling below the tongue, in the floor of the mouth, on the left side. The swelling was present since one year which was slowly grown to the present size. Intraoral examination revealed a solitary swelling seen on left side in the floor of the mouth measuring about 1x2 cm, round to oval in shape, soft in consistency and was associated with pain since one month [Table/Fig-1]. Extra oral examination revealed a single palpable submandibular lymph node on the left side and it was measuring approximately 1×1 cm in size, roughly spherical in shape, freely mobile, firm in consistency and tender on palpation. A diagnosis of ranula was made based on the clinical features and the patient was advised ultrasonography (USG).
A solitary swelling seen on left side in the floor of the mouth
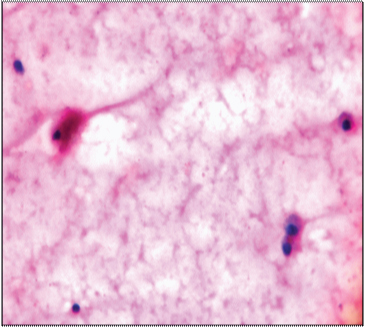
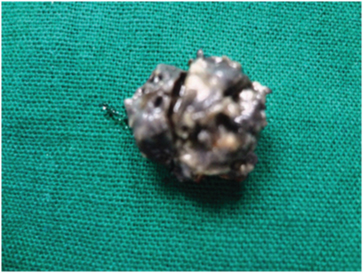
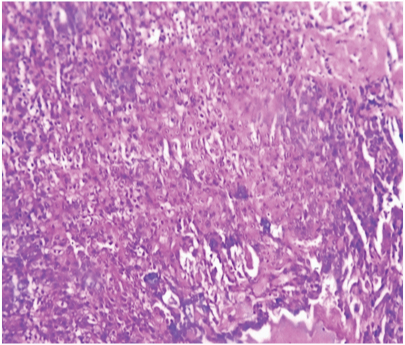
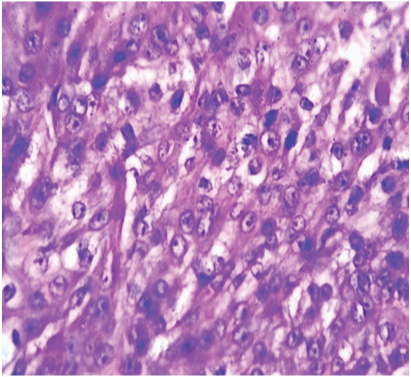
USG revealed solid hypoechoic mass on the left side, anterosuperior to submandibular gland which was suggestive of malignancy. Fine needle aspiration was performed which showed red blood cells, mucin and mucinophages [Table/Fig-2]. Excisional biopsy [Table/Fig-3] was performed and was sent for histopathological examination. On histological examination, Haematoxylin and Eosin stained sections showed prominent mucin filled cystic spaces, minimal cellular atypia and a high proportion of mucous cells along with well formed glandular structures [Table/Fig-4,5]. There was also presence of epidermoid and intermediate cells arranged in form of sheets separated by thin connective tissue septa [Table/Fig-6]. Based on the above histological features a diagnosis of Low Grade Mucoepidermoid Carcinoma was made. As excisional biopsy was performed initially, the patient was advised for excision of the left submandibular lymphnode along with regular follow up.
FNAC (Showed mucin and mucinophages)
(4x scanner view) (Shows well formed glandular structures)
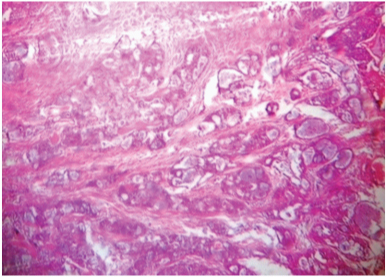
(10x Low power view) (A high proportion of mucous cell)
(40x-High power view) (Epidermoid and intermediate cells arranged in form of sheets separated by thin connective tissue septa)
Discussion
Salivary gland tumours account for less than 5% of head and neck neoplasm [1]. Neoplasms of the sublingual salivary glands are very rare and comprise only between 0.5% and 1% of all epithelial salivary tumours and approximately 1.5% of all carcinomas of the major salivary glands. At diagnosis MEC shows distant metastasis in less than 5% of cases, lungs being the commonest site [2]. Despite their rarity, approximately 80-90% of sublingual gland tumours are frankly malignant. The most common malignant tumour of the sublingual gland is the adenoid cystic carcinoma and mucoepidermoid carcinoma (MEC) is the second most common malignancy [3]. MEC consists of both epidermal and mucous cells in different proportion. It constitutes for less than 10% of all salivary gland tumors, 2/3 arise within the parotid gland and 1/3 arise within the minor salivary glands. MEC may develop at any age but predominantly between the third and sixth decades and women are affected more often than men (3:2). These tumors in the major salivary glands constitutes around 53% and parotid gland is affected most frequently (45%), followed by the minor salivary glands of the palate [4]. In the present reported case the patient was 70-year-old.
MEC was first described by Masson and Berger in 1924. In 1945, Stewart et al., recognized mucoepidermoid of the salivary gland as a separate entity among salivary neoplasm. MEC may arise from pluri-potent reserve cells of the excretory ducts of salivary gland which have the potential to differentiate into squamous, columnar and mucous cells. Although no specific etiologic factors have been identified exposure to ionizing radiation has been reported in some cases [1].
The clinical presentation of MEC of the minor salivary gland is protean and defies concise description. Many lesions present as a bluish or red purple, fluctuant, smooth surfaced mass that is often clinically mistaken as mucocele. The palate was the most common site for minor salivary gland involvement, which accounts for 41.1%. In our reported case floor of the mouth is involved.
Usually the presenting complaint of MEC is an asymptomatic swelling in the floor of the mouth, a mass under the tongue causing some degree of discomfort. Other symptoms include pain, trouble with dental prosthesis retention and tongue numbness. In other cases the tumour may be incidentally discovered by a dentist [5]. In our case patient reported with pain and swelling below the tongue which was mimicking like a ranula.
Macroscopically low grade MEC are small and partially encapsulated and microscopically they are characterized by the presence of more mucous-producing cells than epidermoid and intermediate cells. Hallmark of these tumors are prominent cystic structures lined by mature mucous, intermediate, or epidermoid cells and solid areas are not evident and prominent fibrous stroma often is present. It grows in a well-circumscribed manner, without any small infiltrative islands at the tumor border [6]. All of these features were present in the present case.
MEC displays a widely diverse biologic behaviour and clinical manifestation, which will correlate with tumour stage and grade. High grade MEC is highly aggressive tumour, where as low-grade shows more benign nature even though metastases have also been described in low grade MEC. Mode of metastasis may be lymphatic (cervical lymph node) and haematogenous and most common site for the metastasis is lungs, bones are involved rarely. Others include the liver, brain, skin, ovary/ peritoneum, including other sites [7].
MEC most frequently arise in the parotid gland, and presents as a painless swelling, with or without facial nerve involvement. These tumours can however be found anywhere there are salivary glands. Overall distribution across various glands is as follows major salivary glands: ~50% parotid gland: ~40%, submandibular gland: ~7%, sublingual gland: ~3%. Minor salivary glands: ~50%, palate: most common, retromolar area, floor of the mouth, buccal mucosa, lip, tongue, other: anywhere in the proximal aerodigestive tract, the lacrimal glands and even in the bronchi. In the present case floor of the mouth is involved up to our knowledge only few cases have been reported involving this site [8].
MEC, have a prognosis based upon the clinical stage and histological grade with a good prognosis of MEC in children as majority of them are well differentiated or grade I neoplasm. Low grade MEC has a better 5 year survival rate from 92–100% compare to high grade MEC with 0–43% survival rate [6] with an overall incidence of lymph node involvement ranges from 18–28% [9]. When distant metastases develop in patients with minor salivary gland tumours the average survival is 2.3 years and in those with tumours of the major salivary glands is 2.6 years [10].
Surgery is the main mode of treatment for malignant sublingual gland tumors, and different types of surgical interventions depends on the extent of the primary tumor. For small tumors which are restricted to the floor of the mouth, a wide surgical resection of involved sublingual and also the ipsilateral submandibular salivary gland has to done, as the ductal system is often affected even with limited resection [11]. In our case Low grade MEC in the floor of the mouth was surgically excised along with involved lymphnode.
Conclusion
At times, atypical locations and innocent appearance of the tumour such as the one reported can mislead the clinician and can lead to an erroneous diagnosis. Present case enlightens us about the non confirmatory nature of FNAC and the importance of biopsy as the gold standard in the confirmation of diagnosis. Routine investigations may at times are not conclusive, pressing the need for more specific and advanced laboratory procedures. Recognizing an abnormality is the first and most essential step in the diagnosis of disease entity.
[1]. Bansal A, Shetty DC, Rai HC, Singh HP, Primary intraosseous mucoepidermoid carcinoma of maxillaE-Journal of Dentistry 2011 1(1):14-17. [Google Scholar]
[2]. Ali SA, Memon AS, Shaik NA, Soomro AG, Mucoepidermoid carcinoma of parotid presenting as unilocular cystJ Ayub Med Coll Abbottabad 2008 20(2):141-42. [Google Scholar]
[3]. Sumanth KN, Mainali A, Mucoepidermoid carcinoma: A MimickerJ Nepal Dent Assoc 2009 10(1):31-34. [Google Scholar]
[4]. Phasha Z, Sharma K, Choudhari S, Sulabha AN, Mucoepidermoid carcinoma of palate mimicking vascular lesion: A case reportJournal of dental sciences and research 2013 4(01):9-12. [Google Scholar]
[5]. Guzzo M, Andreola S, Sirizzotti G, Cantu G, Mucoepidermoid carcinoma of the salivary glands: clinicopathologic review of 108 patients treated at the National Cancer Institute of MilanAnn Surgonocol 2002 9:688-95. [Google Scholar]
[6]. Greenberg MS, Glick M, Burket’s Oral Medicine Diagnosis and Treatment 2003 10th edElsevierNew Delhi:235-65. [Google Scholar]
[7]. Asuquo ME, Nwagbara VI, Umana AN, Bassey G, Nnoli MA, Okpara H, Giant Mucoepidermoid Carcinoma of the Parotid Gland: A Case Report and Review of LiteratureJ Clin Exp Oncol 2013 2(1) [Google Scholar]
[8]. Radiopaedia.org/article/mucoepidermoid carcinoma of salivary glands. 11.35, 27th sep:2015 [Google Scholar]
[9]. Spiro RH, Huvos AG, Berk R, Strong EW, Mucoepidermoid carcinoma of salivary gland origin. A clinicopathologic study of 367 casesAm J Surg 1978 136:461-68. [Google Scholar]
[10]. Rapidis AD, Givalos N, Gakiopoulou H, Stavrianos SD, Faratzis G, Lagogiannis GA, Mucoepidermoid carcinoma of the salivary glands. Review of the literature and clinicopathological analysis of 18 patientsOral Oncol 2007 43(2):130-36. [Google Scholar]
[11]. Rinaldo A, Shaha AR, Pellitteri PK, Bradley PJ, Ferlito A, Management of malignant sublingual salivary gland tumoursOral Oncol 2004 40:2-5. [Google Scholar]