Difficulties in Management of a Sessile Subglottic Polyp
H.T. Lathadevi1, S.P. Guggarigoudar2
1 Professor, Department of Ear Nose and Throat, Head & Neck Surgery, BLDE University’s, Sri BM Patil Medical College, Bijapur, Karnataka, India.
2 Professor, Department of Ear Nose and Throat, Head & Neck Surgery, BLDE University’s, Sri BM Patil Medical College, Bijapur, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. H.T. Lathadevi, Professor, Department of Ear Nose and Throat, Head & Neck Surgery, BLDE University’s Sri BM Patil Medical College, Bijapur-586101, Karnataka, India.
E-mail: lathadevi45@gmail.com
Benign laryngeal polyps are usually managed with micro-laryngeal surgery. Occasionally surgery becomes challenging because of size of the polyp or its location. Maintaining the anaesthesia and the airway becomes difficult either during immediate management or during excision. Upper airway obstruction still remains the major indication for tracheostomy in many centers. Nowadays Laryngeal tumour has become the main indication of tracheostomy. Conditions like infections, trauma, benign lesions and prolonged intubation were leading indications previously. Otolaryngologist has to decide a method, often on the spot. Here we are presenting such a case where emergency tracheostomy was the only choice.
Airway obstruction, Stridor, Tracheostomy
Case Report
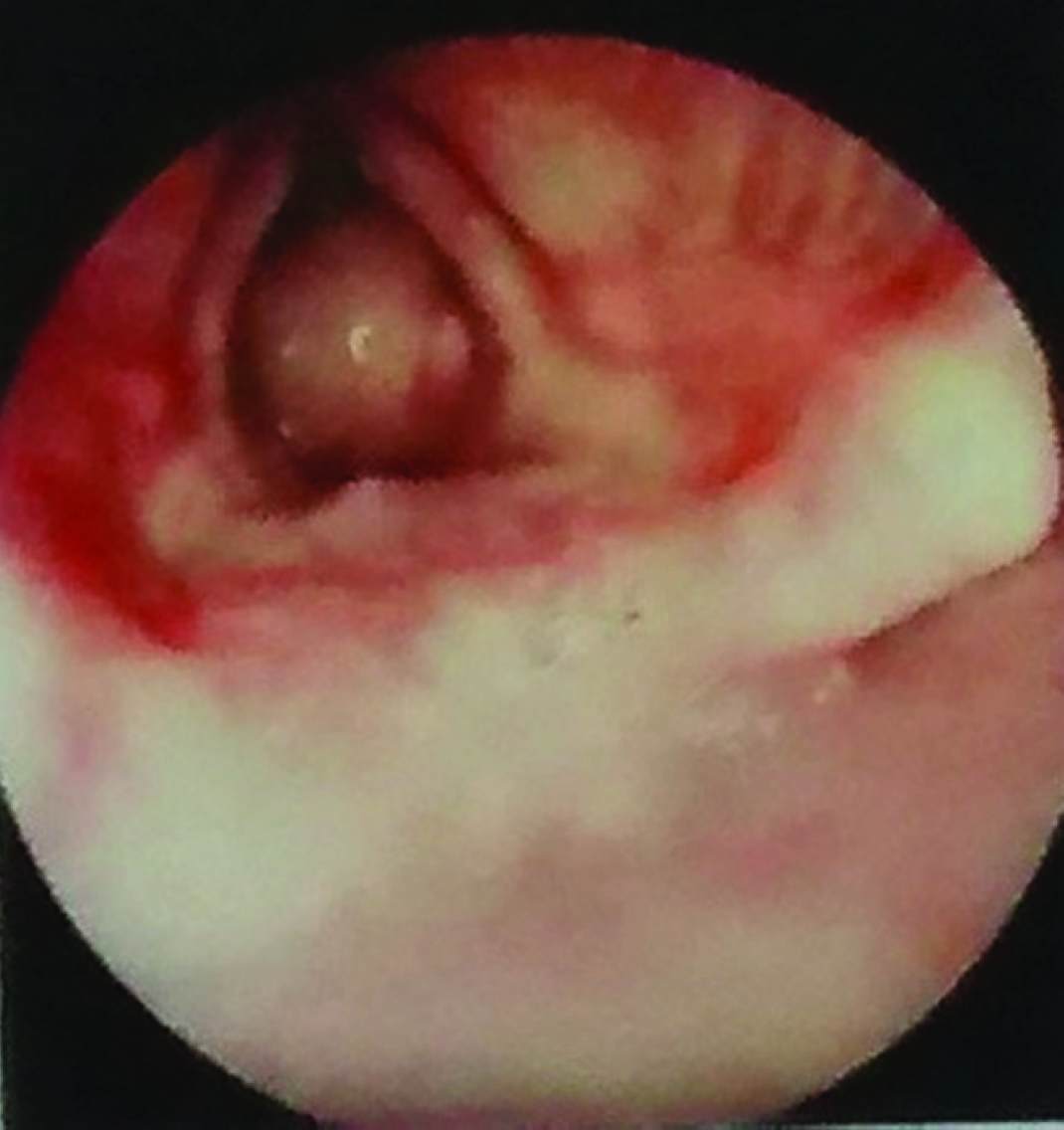
A 35-year-old female patient presented with severe stridor to emergency at our hospital. Patient had mild dyspnea past 30 days which steadily increased to stridor from 3 days. She was seen by a local doctor and was diagnosed as Asthma. She had received antiasthmatic drugs for 15 days with no improvement. On clinical examination, general condition was normal except stridor. Indirect laryngoscopy could not be done. Fiberoptic laryngoscopy revealed a subglottic polyp [Table/Fig-1]. It was huge, sessile & involving the whole of upper part of lumen of subglottis, immediately below the level of true cords. There was no space around the lesion to pass any type of endotracheal tube. The lower level of extension into trachea could not be seen or assessed during fiberoptic laryngoscopy. X-ray lateral view of the neck showed a faint shadow of the lesion upto first tracheal ring. The patient refused CT of the neck at that moment of time. She was maintaining SPO2 of 98%. It was decided to do Tracheostomy under local anaesthesia despite the fact that extent of lower level of polyp was not very clear. Almost a medium to low Tracheostomy (between third and fourth tracheal ring) was done with all precautionary measures, and airway secured with portex No. 7.5 tracheotomy tube.
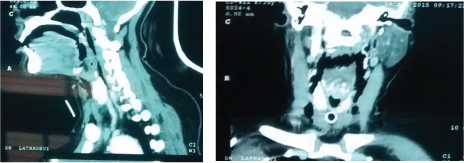
After 2 days CT scan of Neck with contrast was taken which showed a huge polypoid mass of 10X13 mm just below vocal cords, attached to posterior wall of subglottis extending from the level of C4 to first tracheal ring. The mass showed significant enhancement with contrast [Table/Fig-2a&b].
(a) Contrast CT scan of Neck. (b) Contrast CT Neck
Microlaryngeal surgery was done and turned out to be easier as general anaesthesia was through pre-existing tracheal stoma. The polyp was found to be sessile, firm, unyielding and attaching to posterior wall of subglottis. The polyp was excised in bits with minimal bleeding & cautery was done at attached area. Postoperative period was uneventful. Decannulation was done after 3 days.
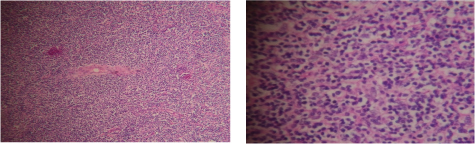
Surprisingly, Histopathological diagnosis given was Nonhodgkins lymphoma (MALT, Mucosa associated lymphoid tissue lymphoma) [Table/Fig-3a&b] which was again submitted for immunohistochemistry for confirmation. Result came as benign subglottic lesion with chronic inflammation with reactive plasmacytosis. The tumour marker Cyclin D1/CD23 was negative and there was no evidence of malignancy. Fibreoptic laryngoscopy on 25th day showed normal laryngeal lumen.
(a) Histopathology previously given as MALT Lymphoma (b) Reactive plasmacytosis
Discussion
Benign laryngeal lesions, especially vocal fold polyps are very common [1] and usually present with hoarseness, vocal fatigue, cough, or foreign body sensation and dysphonia [2]. Laryngeal pathologies may be confused with the symptoms of asthma [3]. The initial dyspnea and wheeze of small sized laryngeal poyps leads to this misdiagnosis. If airway is compromised by mechanical obstruction particularly at subglottis, it manifests with stridor. Subglottic polyps are less common and present with airway obstruction which may become life threatening. Pharyngeal and laryngeal pathology caused by malignancy, extensive scarring or radiotherapy can also lead to such unforeseen situations.
Airway management is difficult in these lesions as anaesthesia & securing the airway is challenging [4]. It is essential for both anaesthetist and otolaryngologist to be aware of different airway methods and have an effective strategy to manage these emergency situations when they arise [5].
Sometimes anaesthesia cannot be given at all and otolaryngologist has to decide about technique of securing the airway in an awake patient. The site of the lesion has to be assessed & decision has to be taken emergently depending on the location, size, site of attachment of the polyp, lower extent of the polyp, saturation of oxygen and also the facilities available.
In the event of a high degree of airway obstruction, endotracheal intubation can be impossible and even dangerous, because it can cause complete airway obstruction [6]. The passage of endotracheal tube requires minimum space around the glottis and subglottis. The exact extent of the lesion and its lower level needs to be established. This can be identified with newer technologies like CT Scan with imaging protocols like 3D and multiplanar reconstruction. Virtual tracheobronchography helps in visualization of better characteristics such as whether the lesion is luminal, external and airway distal to obstruction is patent or closed [7]. In addition to this, the length and diameter of the lesion in relation to the other structures such as vessels are assessed to a much higher degree of accuracy. If the airway allows a small diameter of endotracheal tube, awake fiberoptic intubation [8] with guidewire can be tried. Methods like Laryngeal mask airway [5], High frequency jet ventilation at supraglottic and infraglottic areas have several advantages [9]. When any of these methods are possible, the definitive removal of lesion can also be done at the same setting.
R Pandey et al., reported a case of popping subglottic polyp which was long pedicled which used to pop up during expiration providing some space for intubation [8]. Hence fiberoptic guided awake endotracheal intubation with small sized endotracheal tube during expiratory phase of spontaneous respiration was done. Our case had no patent lumen at subglottic area which made us to think of open tracheostomy. Open tracheostomy maintains airway patency, protects the lungs and permits leakfree ventilation [5]. Ross-Anderson and colleagues have proposed Trans tracheal jet ventilation as an alternative in difficult airway management in adult patients with critical airway and monitor with careful use of automated jet ventilator [9].
Tracheostomy is becoming less and less common as an airway management due to advent of above mentioned better methods. Since the airway is shared by both anaesthesiologist and surgeon, establishing an adequate airway and maintenance of anaesthesia still remains challenging. Alternative airway strategies should be immediately available in case of failure including cardiopulmonary bypass in patients with extensive airway involvement [10]. This is possible only in higher centres where it has become a practice to be ready with a standby Cardiopulmonary Bypass via femoral vessels and then induce fiberoptic bronchoscope guided tracheal intubation. There have been sometimes arguments like “Why use an ox cleaver to kill a chicken?” [11]. Close communication between anaesthetist, surgeon and operation room personnel is essential for optimal care [4].
Our case was a huge polyp of 10x13mm non-pedunculated, snugly fitting the subglottic wall, unyielding to the passage of any instrument. If it had involved Tracheal third or fourth ring, the surgeon would have encountered a totally different situation. Such cases would have been managed better in centres where advanced anaesthetic facilities of jet ventilation and cardiothoracic units are available.
The only last resort of emergency tracheostomy had to be chosen for maintaining O2 saturation as facilities were limited. Fiberoptic bronchoscope with guidewire intubation was available in OT. But it was not considered as there was no room for insertion of small tube beside the lesion. This indicates even during these present times of advanced methods of anaesthesia, emergency tracheostomy still has its own place. Open tracheostomy has a complication rate of 6 to 66% [12]. This rate can increase in any lesion involving larynx or tracheal lumen or displaced trachea. Use of fiberoptic illumination of tracheal lumen [13] or light wand guided Percutatneous tracheostomies have been successfully practiced in difficult cases [14].
Whatever the advancements in the field of airway management and anaesthesia has taken place, Tracheostomy remains as one of the most important standard procedure for airway emergency management, especially in a developing country where patients will not present till they are in an acute and critical condition [15].
Conclusion
Upper airway obstruction due to benign laryngeal lesions, particularly at subglottic level can pose challenging situations for airway management. Apart from newer advanced techniques, emergency open tracheostomy has to be one of the preferred airway methods. Finally, both the surgeon and the anaesthesiologist collectively have to evaluate and decide the relevant airway management.
[1]. Hegde MC, Kamat P, Bhojwani K, Peter R, Polisetti RB, Benign lesion of Larynx. A Clinical studyInd J Otol Laryngol H&N Surg 2005 57(1):35-38. [Google Scholar]
[2]. Sidrah MA, Soliman MS, Airway obstruction: A rare complication of Benign Vocal fold polypsAnn otol rhinol laryngol 2008 117(2):106-09. [Google Scholar]
[3]. Felek S, Celik H, Pulat H, Tastan E, Gıant Vocal Cord NoduleThe Internet Journal of Head and Neck Surgery 2006 1(1):1-6. [Google Scholar]
[4]. Harshad PL, Vinayak P, Nagraj MC, Tejesh CA, Anaesthesia management in a child with laryngeal papilloma causing near complete airway obstructionSaudi J Anaesthesia 2015 (1):86-88. [Google Scholar]
[5]. Divatia JV, Bhowmickm K, Complications of endotracheal intubation and other airway management proceduresIndian J Anaesth 2005 49(4):308-18. [Google Scholar]
[6]. Pang L, Feng YH, Ma HC, Dong S, Fiberoptic bronchoscopy-assisted endotracheal intubation in a patient with a large tracheal tumourInt Surg 2015 100(4):589-92. [Google Scholar]
[7]. Patil VP, Airway emergencies in CancerInd J Crit Med 2007 11(1):3 [Google Scholar]
[8]. Pandey R, Harg R, Kumar A, Darlong U, Case Report: Airway management of a patient with popping pedunculated subglottic laryngeal polypActa Anaesth Belgica 2009 60:251-53. [Google Scholar]
[9]. Ross Anderson DJ, Ferguson C, Patel A, Transtracheal jet ventilation in 50 patients with severe airway compromise and stridorBr J Anaesth 2011 106(1):140-44.doi: 10.1093/bja/aeq278. Epub 2010 Oct 14 [Google Scholar]
[10]. Crastnopol P, Platt N, Phillips WR, Mesbah M, Henry EI, Aaron RS, Resection of solitary tracheal papilloma using cardiopulmonary bypassN Y State J Med 1967 67:1166-69. [Google Scholar]
[11]. Guangsuo W, Shaolin L, Zongquan S, Surgical Management of tracheal compression caused by mediastinal goiter: Is Extracorporeal circulation is a Requisite?J Thoracic Dis 2009 1(1):48-50. [Google Scholar]
[12]. Friedman YF, Ides J, Mizock B, Samuel J, Patel S, Appavu S, Comparision of percutaneous and surgical tracheostomiesChest 1996 110:480-85. [Google Scholar]
[13]. Abbas BM, Howes WJ, Hung OR, Light guided tracheal puncture for percutaneous tracheostomyCan J Anaesth 2000 47:919-22. [Google Scholar]
[14]. Agro F, Salvinelli F, Gheradi S, Casde M, The light wand: A useful alternative aid in difficult tracheostomyCan J Anaesth 2002 49:1000-1. [Google Scholar]
[15]. Adedeji T, James T, Olasun AO, Julius ID, Indications and outcomes of tracheotomy: An experience in a resource-limited environmentJ health research and Rew 2014 1(2):40-43. [Google Scholar]