Primary Extra-Gonadal Retroperitoneal Seminoma, Clinically Mimicking Sarcoma
Davsheen Bedi1, Permeet Kaur Bagga2, Amarjit Singh3, Vaishali Verma4
1 Post Graduate Student, Department of Pathology, Government Medical College, Amritsar, Punjab, India.
2 Associate Professor, Department of Pathology, Government Medical College, Amritsar, Punjab, India.
3 Professor, Department of Pathology, Government Medical College, Amritsar, Punjab, India.
4 Post Graduate Student, Department of Pathology, Government Medical College, Amritsar, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Davsheen Bedi, Post Graduate Student, Department of Pathology, Government Medical College, Amritsar-143001, Punjab, India.
E-mail: davsheen28@gmail.com
Extra-gonadal Germ cell tumours (EGCTs) are germ cell tumours that are found in locations other than the gonads. These tumours are seen in young males in the midline, mostly in the mediastinum followed by retroperitoneum, pineal gland, and sacrococcygeal area. While most of these are non-seminomatous, few are seminomatous. We present here a case report of a 25-year-old, mentally retarded male patient, with bilaterally normal testes, who presented with a huge mass in abdomen. The ultrasound and CECT (Contrast Enhanced Computerized Tomography) scan done showed two large retroperitoneal masses, which on FNAC (Fine Needle Aspiration Cytology) suggested germ cell tumour. Surgical resection was done and the subsequent histopathological examination provided the diagnosis of seminoma, which was further confirmed by PAS (Periodic Acid Schiff) staining and Immunohistochemistry for PLAP (Placental Alkaline Phosphatase). Retroperitoneum is a common site for sarcomas, which also present as huge, bulky masses. Thus, EGCTs should be considered in the differential diagnosis of a soft-tissue mass in abdomen, especially arising in the retroperitoneum.
Abdominal soft-tissue tumour, Germ cell tumour, Retroperitoneal soft tissue tumour
Case Report
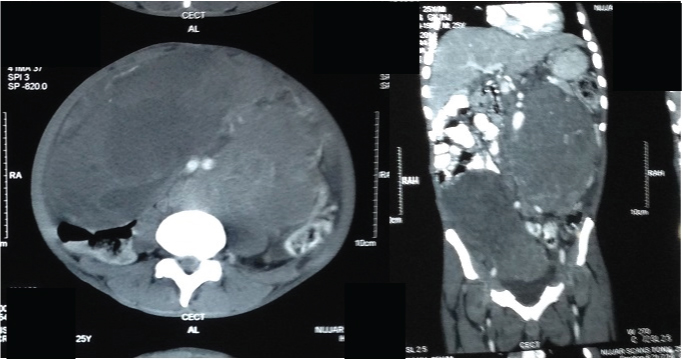
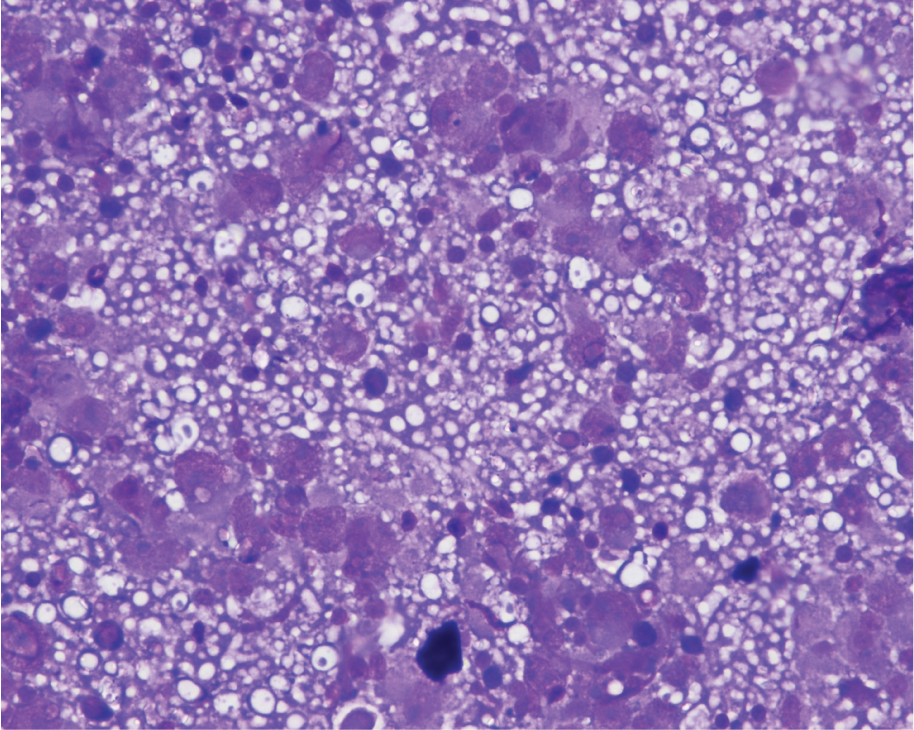
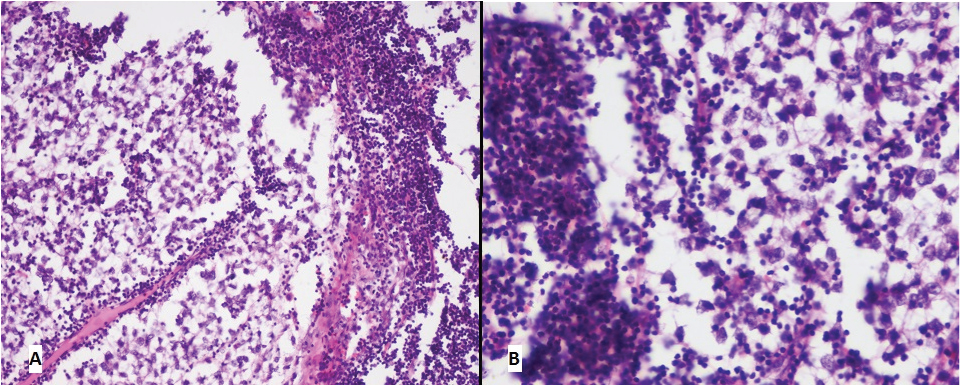
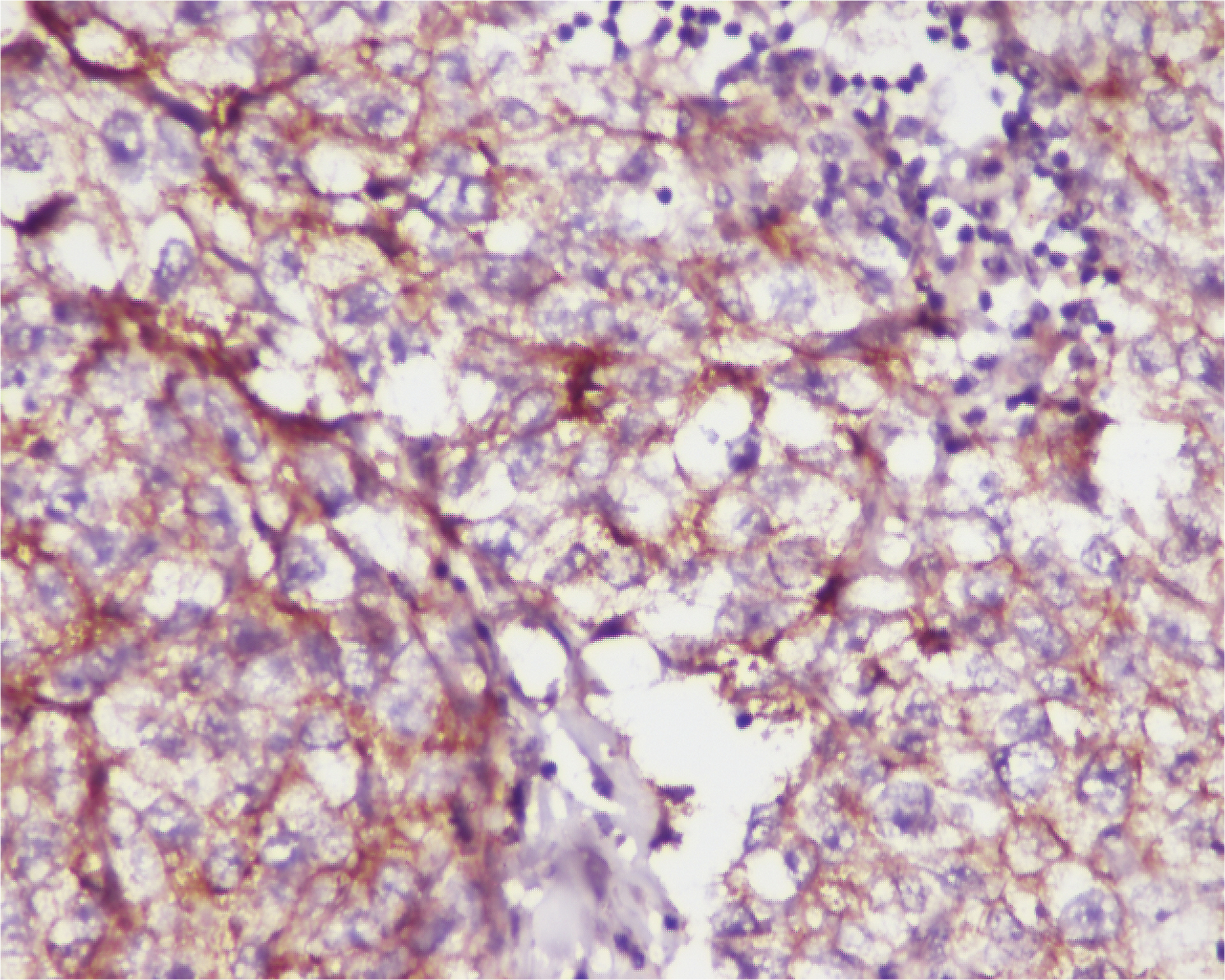
A mentally retarded, 25-year-old male was brought to emergency, with chief complaint of a huge palpable painless mass in abdomen for the past 6 months, extending from epigastrium to the left hypochondrium and left lumbar region. There was no significant family history. Both the testes were present in their normal anatomical position. Ultrasonography revealed a heterogenous mass in abdomen about 20x10cm, extending from epigastrium, crossing the midline and going upto the right pelvic area. Ultrasonography of the scrotum showed normal testes bilaterally. A CECT scan done showed [Table/Fig-1] two heterogeneously hypodense retroperitoneal masses, one measuring 21x16x13.5 cm lying in the pre-vertebral and the left para-vertebral region, extending from the level of pancreas to the pelvic brim, and the other measuring 17x14.5x11.5 cm, extending from umbilicus down into the pelvis on the right side. Also, there was no significant lymphadenopathy visualized on CT scan and none of the organs showed any abnormality or any evidence of metastasis. FNAC done subsequently, showed [Table/Fig-2] against a “tigroid” background, many singly scattered cells having round to oval nuclei, irregular nuclear membrane, and prominent nucleoli with slightly basophilic, scanty cytoplasm and background showing few lymphocytes. Diagnosis of malignant round cell tumour was given with the possibility of germ cell tumour and histopathological examination was advised. After the FNAC report suggested a germ cell tumour, the testes were re-examined clinically to ensure their normal anatomical position bilaterally, and a scrotal ultrasound was also done to rule out any occult primary tumour in the testes. The patient then underwent exploratory laparotomy and both the masses were removed. No lymph nodes were recovered at the time of surgery. Gross examination showed [Table/Fig-3] two large soft tissue masses with nodular surface, one measuring 15x13x10cm and the other 18x16x10cm. Cut surface showed multiple areas of haemorrhage and necrosis. Microscopy [Table/Fig-4a&b] showed tumour cells arranged in nests and separated by thin septae which were infiltrated by lymphocytes. The cells were polygonal with clear cytoplasm, vesicular nuclei and prominent nucleoli. There were no microscopic features suggestive of other non-seminomatous germ cell tumours, neither on H&E sections, nor on immunohistochemistry. Thus, diagnosis of Extragonadal Seminoma was suggested, which was further confirmed by patchy PAS (Per-iodic Acid Schiff) positivity [Table/Fig-5] and Immunohistochemistry for PLAP (Placental Alkaline Phosphatase) positivity [Table/Fig-6]. CD30 was also done to rule out embryonal carcinoma component of mixed germ cell tumour and was found to be negative. Postoperatively, the patient underwent 4 cycles of chemotherapy with BEP (Bleomycin, Etoposide and Cisplatin) each lasting 3 weeks, after which he was followed up for a period of one year and was found to be completely symptom free and without any recurrence.
CECT scan axial (L) and coronal (R) views showing two heterogenous retroperitoneal masses
Photomicrograph of FNAC showing the “tigroid” background (400X, MGG)
Photograph showing gross appearance of the encapsulated mass (L) with multiple areas of haemorrhage and necrosis on cut section (R)

a) Photomicrograph showing the cell nests separated by fibrous septae, infiltrated by lymphocytes (100X, H&E); b) Photomicrograph showing uniform appearing cells with pale to clear cytoplasm, with central vesicular nucleus and a prominent nucleolus (400X, H&E)
Photomicrograph showing patchy Per-iodic acid schiff positivity (400X, PAS)
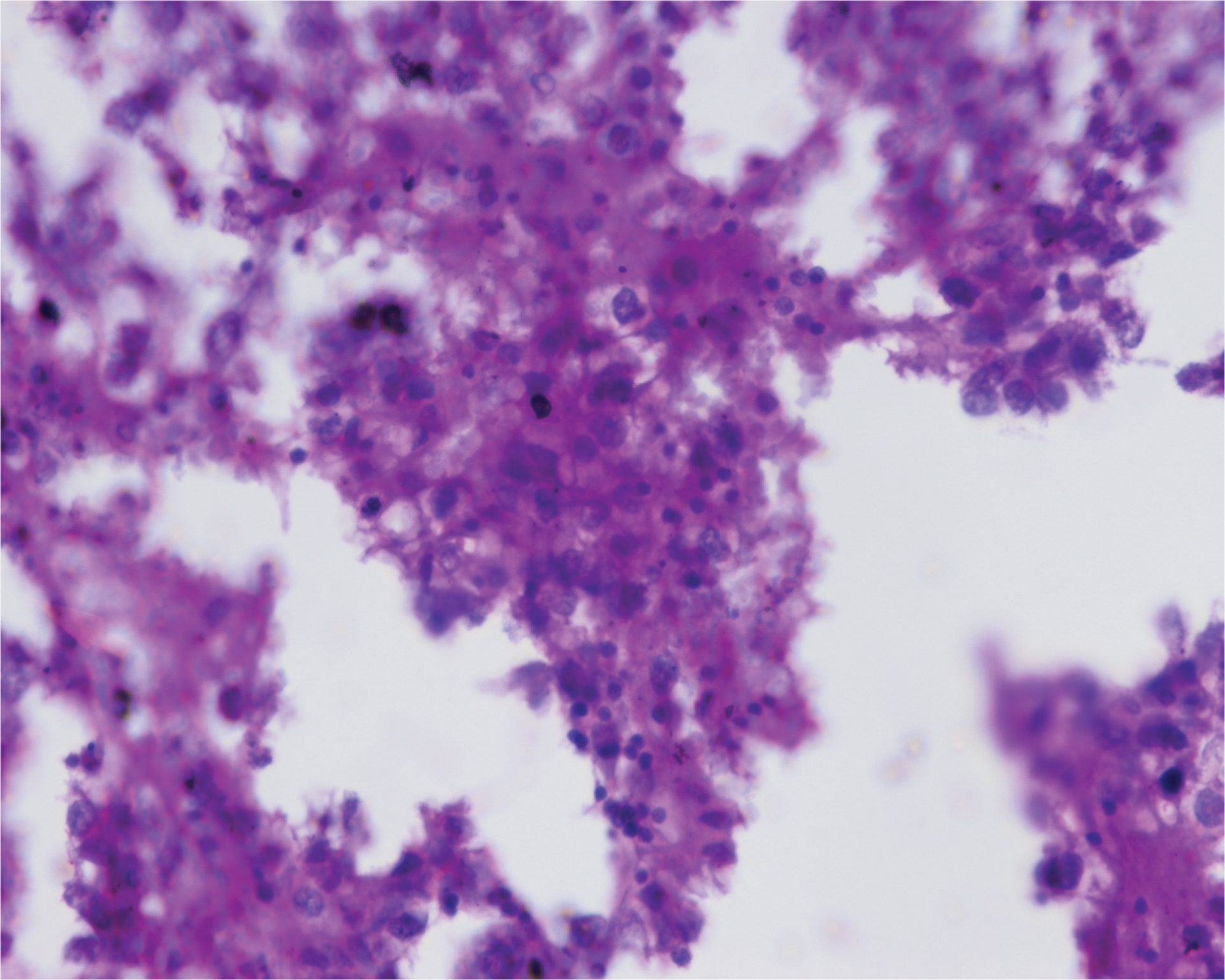
Photomicrograph showing membranous positivity for placental alkaline phosphatase (400X, PLAP)
Discussion
Germ cells tumours in men usually arise from testes, only 1-2% originate from others locations and are called Extra-gonadal Germ cell tumours (EGCTs) [1]. Majority of EGCTs are non-seminomatous, and only 30-40% are seminomatous [2]. Retroperitoneal seminomas are very rare EGCTs, with very few reported cases. They arise due to arrest or misplacement of germ cells during their embryonic migration or can also be gonadal in origin, arising from reverse migration or metastasis from occult or burnt out primary gonadal tumours [3,4]. It commonly affects young males [3,4], as seen in our present case, a 26-year-old male. Two most common sites of EGCTs are mediastinum and retroperitoneum [2–4]. While the mediastinal EGCTs present early with respiratory complaints and chest pain, the retroperitoneal ones present late with tumours reaching large dimensions at presentation [3,4] as was seen in our present case. The aetiology of EGCTs is unknown. In rare cases, they have been associated with Klinefelter’s syndrome [5]. Our patient, though mentally retarded, did not show features of Klinefelter’s syndrome clinically. Tumour markers were not done in this case since clinically testicular germ cell tumour was not suspected. Though not much has been said in literature about FNACs done in EGCTs, in our patient it was done and showed a very typical picture of seminoma with tigroid background having lymphocytes along with atypical cells having vesicular nuclei and prominent nucleoli. Histologically these retroperitoneal seminomas are identical to their gonadal counterparts, and their diagnosis can be further confirmed with cytochemical PAS staining and immunohistochemistry with PLAP, CD117 and podoplanin (D2-40) [3,6,7]. Presence of other germ cell tumours is to be ruled out by negative staining for markers like CD30, AFP and hCG. The differential diagnosis of soft-tissue mass in retroperitoneum includes lymphoma, metastasis and soft-tissue sarcomas, which are more common and need to be ruled out. It is also very important to differentiate the true primary EGCTs from those developing secondary to an occult or a burnt out primary testicular tumour, metastasizing to the peritoneum, thus requiring a complete clinical examination and scrotal ultrasound. An occult primary may be suggested by clinical finding like undescended testes, or ultrasonographically by scar tissue in the testes, or micro calcifications, or any hypoechoic shadows [4]. In the present case also both the testes were found to be in their normal anatomical position on clinical examination and the scrotal ultrasound showed none of the above features, thus suggesting the primary nature of the extra-gonadal seminoma. In case an occult/burnt out primary is found, its removal is important for a complete treatment of the patient. Seminomas, with a 5-year survival rate of 90%, respond well to chemotherapy and radiotherapy, only some requiring debulking surgeries [2,8]. Thus, retroperitoneal seminomas have a good prognosis as compared to that of the other more common retroperitoneal tumours likes metastasis, sarcomas and lymphomas. Therefore, the clinicians and surgeons should keep in mind the possibility of a retroperitoneal seminoma, while encountering large abdominal/ retroperitoneal masses.
Conclusion
Extragonadal retroperitoneal seminomas are a rare entity, having an excellent prognosis with appropriate management. These should be considered in the differential diagnosis of a male patient presenting with a soft tissue mass in the retroperitoneum, even with normal bilateral testes.
[1]. Walsh PC, Retik AB, Darracott VE, Wein AJ, Neoplasms of the tesitsIn: Campbell’s Urology 2002 8th edLondonWB Saunders [Google Scholar]
[2]. Bokemeyer C, Droz JP, Horwich A, Gerl A, Fossa SD, Beyer J, Extragonadal seminoma: An international multicenter analysis of prognostic factors and longterm treatment outcomeCancer 2001 91(7):1394-1401. [Google Scholar]
[3]. McKenney JK, Heerema-McKenney A, Rouse RV, Extragonadal germ cell tumors: a review with emphasis on pathologic features, clinical prognostic variables, and differential diagnostic considerationsAdv Anat Pathol 2007 14(2):69-92. [Google Scholar]
[4]. Costanza C, Alba F, Alfredo T, Loredana L, Rocchina C, Mariella C, A Case Report of Retroperitoneal Seminoma and Literature ReviewJ Nucl Med Radiat Ther 2013 4(1):148Available form: http://www.omicsonline.org/2155-9619/2155-9619-4-148.digital/2155-9619-4-148.html [Google Scholar]
[5]. Aguirre D, Nieto K, Lazos M, Pena YR, Palma I, Kofman-Alfaro S, Extragonadal germ cell tumors are often associated with Klinefelter syndromeHum Pathol 2006 37(4):477-80. [Google Scholar]
[6]. Bahrami A, Ro JY, Ayala AG, An overview of testicular germ cell tumorsArch Pathol Lab Med 2007 131(8):1267-80. [Google Scholar]
[7]. Yu H, Pinkus GS, Hornick JL, Diffuse membranous immunoreactivity for podoplanin (D2-40) distinguishes primary and metastatic seminomas from other germ cell tumors and metastatic neoplasmsAm J Clin Pathol 2007 128(5):767-75. [Google Scholar]
[8]. Gutierrez-Delgado F, Tjulandin SA, Garin AM, Long term results of treatment in patients with extragonadal germ cell tumoursEur J Cancer 1993 29:1002-05. [Google Scholar]