To study the level of the division of abdominal aorta in relation to the lumbar vertebral levels. To propose the change in the upper border of Radiotherapy portals used in the treatment of Cervical Cancers.
Materials and Methods
The study was performed after obtaining clearance from the Institutional Ethical Review board. It was a prospective observational study. The carcinoma of cervix patients treated in Department of Radiation Oncology, MS Ramaiah Medical College hospital, Bangalore, India, from December 2010 to January 2012, who met the inclusion criteria were the subjects of present study.
Inclusion Criteria
All newly diagnosed, histopathologically proven cases of carcinoma of cervix who received Radiotherapy with radical intent were included in the present study.
Exclusion Criteria
Postoperative cases were excluded from the present study.
The diagnoses of all the patients were established based on clinical examination, histopathology and appropriate radiological investigations. Prior informed consent was taken from all patients before enrolling into the study. All the patients underwent aquaplast immobilization in supine position and Contrast Enhanced CT simulation for Radiotherapy Planning. Axial CT sections extending from L1 to mid thigh with slice thickness varying from 3mm to 5mm were taken. The DICOM images were loaded on to Commercial Treatment Planning System, Prowess version 4.71 for Radiotherapy planning.
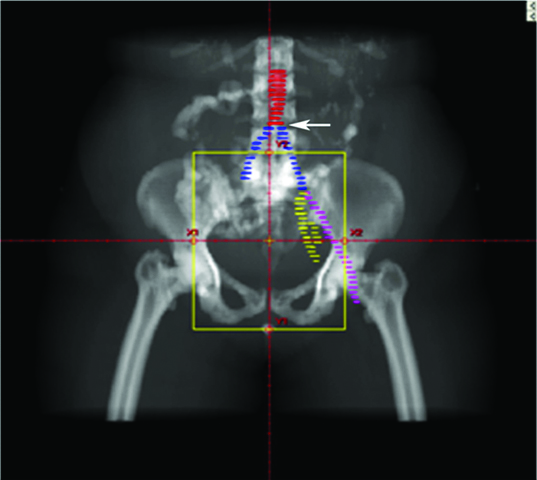
The level at which division of Abdominal Aorta takes place into right and left Common Iliac arteries with respect to vertebral levels was determined [Table/Fig-1]. For the ease of analysis, the level of division was subdivided into three categories namely: (a) L3-L4 intervertebral space; (b) in front of body of L4; and (c) L4-L5 intervertebral space.
Contoured abdominal aorta (red) and common iliac vessels {blue}, arrow mark shows the division of abdominal aorta in relation with vertebral level. The left External iliac artery (Pink) and Internal Iliac artery (yellow) are marked.
Statistical Analysis
Descriptive statistical analysis was carried out in the present study. The number of patients falling into different categories were tabulated and expressed in percentages. The statistical software SPSS V 17.0 and Microsoft excel was used to generate the graphs and tables.
Results
Twenty six patients of Carcinoma of uterine cervix treated with definitive radiotherapy were analyzed. It was observed that 50% of our patients were aged 41-50 years. The mean age was 53.20 ± 10.12 years [Table/Fig-2]. A 54.2% of our patients presented in stage IIIB. 95.8% of the patients were in stage IIB and beyond [Table/Fig-3].
Age distribution of the patients studied
| Age in years | Number of patients (%) |
|---|
| 31-40 | 1 (3.8%) |
| 41-50 | 13 (50%) |
| 51-60 | 7 (27%) |
| 61-70 | 5 (19.2%) |
| Total | 26 (100%) |
Distribution of patients based on the FIGO staging of cervical cancer at the time of presentation
| Stage of disease | Number of patients (%) |
|---|
| II A | 1 (3.9%) |
| II B | 8 (30.7%) |
| III A/B | 2 (7.7%) |
| III B | 15 (57.7%) |
| Total | 26 (100%) |
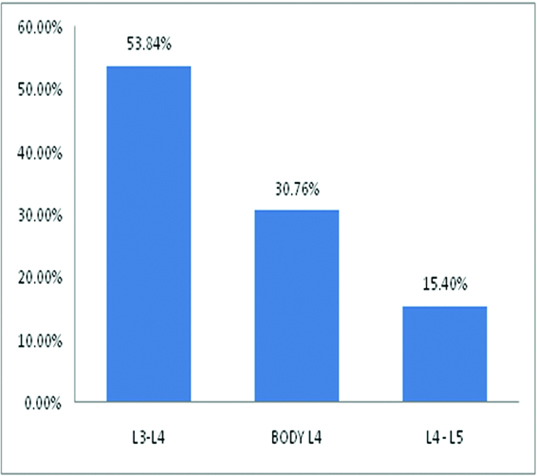
The division of abdominal aorta into common iliac arteries occurred at the level of L3-L4 intervertebral space, in front of Body of L4 vertebra and L4-L5 intervertebral space in 53.84%, 30.76% and 15.40% of the patients respectively [Table/Fig-4].
Graphical representation showing the division of abdominal aorta in relation to the level of Vertebrae.
Discussion
The present study was intended to evaluate the level of division of the abdominal aorta into right and left common iliac arteries in relation to the vertebral bony landmarks. Majority of our patients had the division of aorta at the level of L3-L4 intervertebral space. More than 80% of our patients would have received less than the intended dose to common iliac group of lymphnodes, if upper border of Radiotherapy field was kept at the level of L4-L5 intervertebral space as it is followed in Conventional planning technique.
Historically, the upper border of field of Radiotherapy was kept at L4-L5 intervertebral space with assumption that the division of the aorta occurs at this level. The data on level of division of abdominal aorta to common iliac arteries with respect to vertebral bodies is limited to anatomy textbooks and very few articles based on surgical or cadaveric series [4–10]. The present article is the first article which studies the division radiologically based on Computed tomographic scans.
Grays’ Anatomy and Hollinshead’s textbook of Anatomy report that the division takes place at the level of lower border of L4 vertebra [4,5], whereas, Cunningham’s manual of practical Anatomy and Moore clinically oriented Anatomy report it as to occur at the level of L4 vertebral body [6,7]. Bergman et al., says that division of abdominal aorta occurs at the level of L4-L5 interspace in 80% of the cases. Division above this level is very unusual and occurs in 9% of cases [8]. An Indian Study on Cadaveric specimens showed that the division of the abdominal aorta occurs at the level of body of L4 in 54% of the cases [9]. There is only one surgical series reported by Greer et al., which reports that the division of abdominal aorta takes place at the level of L4-L5 intervertebral space [10].
However in our study, 53.84% of aortic divisions occurred at the level of L3-L4 interspace and only 15.4% of the cases had division of aorta at the level of L4-L5 interspace. Our study is on live individuals and is probably more relevant in clinical practice than those on cadaveric series.
There is paucity of data on the consequences of missing common iliac lymph nodes in patients receiving Radiotherapy for carcinoma of cervix. Beadle et al., and Tamaki et al., reported that most of the marginal recurrences after Radiotherapy in treatment of cancer cervix occur in the common iliac nodal area, immediately superior to the Radiotherapy field [11,12]. Our results are the possible explanation for such a pattern of recurrence.
The level of the upper border of the Radiotherapy fields in conventional technique based on bony landmarks should be kept at the level above L3-L4 intervertebral space or at the lower border of L2 vertebra, in order to cover common iliac nodes adequately. However this results in larger volume of bowel in the field of Radiation and more toxicity which can be reduced by using either corner lead shields or conformal blocks. Hence, whenever feasible, it is highly recommended to use Computed tomography based Radiotherapy planning for treating carcinoma cervix patients. The current standard of practice in our hospital is contrast enhanced CT based radiotherapy planning for all patients of carcinoma cervix.
Conclusion
The division of Abdominal Aorta occurs at a higher level than L4-L5 intervertebral space. In majority of the patients studied, division of abdominal aorta occurred at the level of L3-L4 intervertebral space. It is mandatory to treat common iliac group of nodes to adequate dose of radiation in all carcinoma cervix patients, failing which will result in marginal recurrences as shown by literature review. It is highly recommended to do a Computed Tomography based treatment planning for all the patients to individualize the Radiotherapy treatment portal. However, in the institutes where there is no facility for CT based planning, it is proposed to shift the upper border of Radiotherapy treatment portal above the level of L3-L4 intervertebral space.