Bilateral Krukenberg Tumours Diagnosed Primarily by Transabdominal Sonography- A Case Report
Rudresh Hiremath1, Krishna Prasanthi Padala2, Mahesh3, Gautham Gowda3, Aruna Pailoor4
1 Associate Professor, Department of Radiodiagnosis, K V G Medical College and Hospital, Sullia, Dakshina Kannada, Karnataka, India.
2 Senior Resident, Department of Radiodiagnosis, K V G Medical College and Hospital, Sullia, Dakshina Kannada, Karnataka, India.
3 Senior Resident, Department of Radiodiagnosis, K V G Medical College and Hospital, Sullia, Dakshina Kannada, Karnataka, India.
4 Assistant Professor, Department of Radiodiagnosis, K V G Medical College and Hospital, Sullia, Dakshina Kannada, Karnataka, India.
5 Senior Resident, Department of Radiodiagnosis, K V G Medical College and HospitalSullia, Dakshina Kannada, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rudresh Hiremath, Associate Professor, Department of Radiodiagnosis, K V G Medical College and Hospital Sullia, Dakshina Kannada, Karnataka-574327, India.
E-mail: drrudresh76@yahoo.co.in
Krukenberg tumour, also known as carcinoma mucocellulare, is a metastatic adenocarcinoma of ovaries from different primary tumour sites. Gastric carcinoma is most common primary tumour responsible for approximately 50% of Krukenberg tumours. Discrimination between primary ovarian cancer and metastatic tumours in the ovary is important, because their management is different. Here we present a case of female suffering from gastric carcinoma with bilateral Krukenberg tumours, diagnosed primarily by transabdominal sonography. The patient was referred to higher centre for further treatment and followed up.
Adenocarcinoma of stomach, Lead vessel sign, Ovarian tumours
Case Report
A 39-year-old female was admitted in Department of Gynaecology with complaints of amenorrhea for 4 months, lower abdominal pain since 3 months associated with nausea, night sweats, and loss of weight and appetite. On probing patient also gave history of intermittent vomiting for the last three months. On examination patient was moderately built and poorly nourished. Respiratory system examination showed bilateral pleural effusion with reduced breath sounds. Per abdominal examination showed diffuse lower abdominal tenderness with palpable abdomino-pelvic mass lesions present in right and left iliac fossae. Laboratory investigations showed anaemia. With this clinical scenario patient was referred to department of Radio diagnosis for transabdominal ultrasonography with provisional diagnosis of primary ovarian tumours.
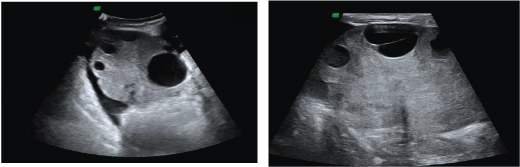
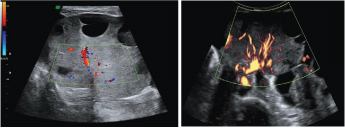
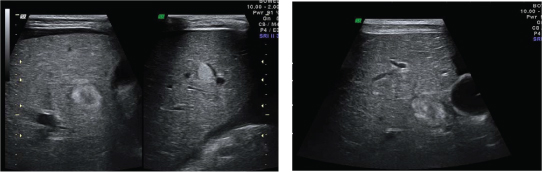
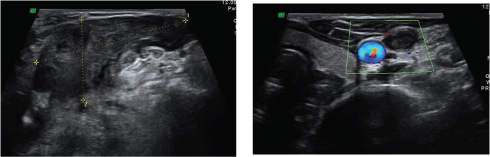
Ultrasound examination revealed, two well defined homogenously hyper echoic predominantly solid abdomino-pelvic mass lesions measuring approximately 7 to 8 cm in diameter with peripherally situated cysts inseparable from the ovaries [Table/Fig-1]. On colour Doppler both mass lesions showed main lead vessel penetrating from the periphery and branching in tree pattern to supply the tumour, known as lead vessel sign [Table/Fig-2]. On hepatic examination there were multiple well defined hyperechoic nodules studded in both lobes of liver suggestive of metastases [Table/Fig-3]. Hepatic metastases with hyperechoic nodules hints the diagnosis more towards gastro-intestinal malignancy, which made us to scrutinize entire gastrointestinal tract of the patient. On gastric examination there was circumferential polypoidal wall thickening of fundus & body of stomach with loss of GUT signature with locoregional lymphadenopathy, pointing the diagnosis towards the gastric malignancy [Table/Fig-4]. On screening the left supraclavicular region a large vascular lymph node was noted infiltrating the adjacent left jugular vein causing jugular vein tumour thrombosis [Table/Fig-5].
Transabdominal ultrasound of ovarian masses with curvilinear and linear transducers depicting homogenously hyper echoic solid masses with peripherally placed cysts
Colour Doppler of ovarian masses showing lead vessel sign
Transabdominal sonography of right lobe of liver showing hyper echoic nodules suggestive of metastases
Transabdominal sonography of stomach with linear and curvilinear transducers showing circumferential wall thickening of fundus and body of stomach with loss of GUT signature
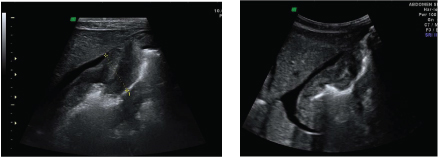
Sonography of left supraclavicular region with linear transducer depicting metastatic lymph node with left IJV tumoural thrombosis
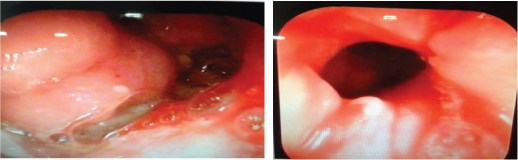
Finally on combining all the findings possibility of gastric malignancy with locoregional nodal, hepatic, bilateral ovarian and left supraclavicular nodal metastasis was considered and patient was referred for endoscopy. On endoscopic examination polypoidal growth was noted in the fundus and body of stomach [Table/Fig-6]. Endoscopic guided biopsy was performed which showed adenocarcinoma of stomach.
Gastric endoscopy revealing polypoidal mass lesion in the fundus and body of stomach
The patient was referred to higher centre for further treatment. Surgical resection of the primary and the metastatic ovarian tumours was done followed by chemotherapy. Histopathological diagnosis of adenocarcinoma of stomach was made.
Discussion
Krukenberg tumours accounts for 1 to 2% of all ovarian neoplasms. Krukenberg tumours are metastatic adenocarcinoma of ovaries arising primarily from the gastric carcinoma. Estimated incidence of these tumours is approximately 0.16 per 100000 per year [1]. Most of these tumours are diagnosed along with the primary neoplasm, however in 20-30% cases after surgical removal. Presence of Krukenberg tumours at the time of imaging poses extremely poor prognosis for the patients with survival rate ranging from 12 to 23.4 % [2].
The condition was first described by Friedrich E Krukenberg, German pathologist [3,4]. Histopathologically these tumours are characterized by the presence of signet ring cells and pseudosacroma proliferation of ovarian stroma [5]. Majority of Krukenberg tumours originate from gastric malignancy, however primary from bowel (11%), breast (4%), biliary system (3%), caecal appendix (3%), pancreas, cervix, urinary bladder and renal pelvis also accounts for it [6]. About 80% of Krukenberg tumours are bilateral and range in size from 5 to 20 cm. Ovaries affected by these tumours retains its shape, irrespective of the size.
Three pathways have been postulated by various pioneers for spread of primary ovarian malignancy to ovaries, they are lymphatic, haematic and peritoneal [6]. Paucity of tumour deposits over the ovarian surface and absence of peritoneal infiltrates discards the peritoneal pathway of spread [6]. Rich lymphatics draining gastric mucosa and submucosa initiating retrograde lymphatic spread to ovary is mostly accepted theory [7].
An ovarian mass may be the initial manifestation of a primary tumour located elsewhere, the primary tumour being detected only following the diagnosis of the metastatic tumour [8].
Transabdominal sonography of abdomen and pelvis is primary imaging and screening modality for females with gynaecological complaints. Diagnosing unilateral or bilateral ovarian masses or tumours is cakewalk for all radiologists but defining them as primary or secondary is a brain teaser.
On ultrasound Krukenberg tumours shows varied echogenicity ranging from purely solid to purely cystic. Most frequently these tumours will be homogenously hyperechoic solid masses with few cysts within. There will be large lead vessel penetrating the mass from the periphery and nourishing the tumour by branching in tree pattern, known as lead vessel sign, with high speed and low resistance on spectral Doppler. This colour Doppler sign is more frequently detected in solid ovarian metastases from the stomach, the breast, and lymphoma compared with primary invasive ovarian carcinomas [2]. Sonography and colour Doppler imaging are determinant in rising the suspicion of a metastatic tumour, thus leading to a search for a possible primary tumour in the stomach [2].
According to the study conducted by Testa et al., sonographic features of Krukenberg tumours is portrayed by the origin of primary tumours [9]. These metastatic ovarian tumours will be solid with well defined margins if primary is from stomach, lymphoma, breast & uterus, where as those derived from colon, rectum, biliary tract are multicystic, heterogenous with irregular borders [9].
Presence of bilateral mixed solid and cystic ovarian masses are not specific for Krukenberg tumour, as many primary ovarian neoplasm depict same morphology.
Contrast enhanced ultrasonography (CEUS) documented the presence of contrast enhancement in the arterial phase followed by wash-out in the late venous phase in both the ovarian mass and primary tumour like gastric wall that is the typical CEUS behaviour of malignant lesions of the liver and other abdominal organs [10].
The presence of lead vessel sign in the ovarian masses and hyperechoic hepatic metastases in the current case scenario made us to scrutinize the gastrointestinal tract for the primary neoplasm and aided in the diagnosis of gastric carcinoma. Thus, the sonographic observations of Krukenberg tumours are important.
There are similar case reports with classical Sonographic findings and Doppler characteristics of lead vessel sign [11,12]. In a retrospective study conducted by Testa et al., in 67 patients with metastatic ovarian tumours, primary was from gastric adenocarcinoma [9]. According to most of the cases listed in the literature diagnosis of the primary tumour was done only after the resection and definitive pathological diagnosis of metastatic lesion of the ovary.
Conclusion
Presence of bilateral ovarian tumours with lead vessel sign in relatively young patient should alert every radiologist to scrutinize the gastrointestinal tract thoroughly for primary tumours. Krukenberg tumour is an uncommon metastatic tumour of the ovary and may cause diagnostic confusion with primary ovarian tumours. Distinction from the latter is of great importance as misclassification of Krukenberg tumour as a primary ovarian tumour may lead to suboptimal treatment of the patient.
[1]. Kiyokawa T, Young RH, Scully RE, Krukenberg tumours of the ovary: a clinicopathologic analysis of 120 cases with emphasis on their variable pathologic manifestationsAm J Surg Pathol 2006 30:277-99. [Google Scholar]
[2]. Testa CA, Licameli A, Legge AD, Mascilini F, Pelagalli M, Scambia G, Colour Doppler Sonographic features of Krukenberg tumour in pregnancyJ Ultrasound Med 2009 28:695-98. [Google Scholar]
[3]. Vakili SM, Sharbatdaran M, Noorbaran A, Siadati S, Moslemi D, Shafahi S, A Case of Colon Cancer with Breast Metastasis and Krukenberg TumourInt J Hematol Oncol Stem Cell Res 2014 8(1):46-50. [Google Scholar]
[4]. Zuleta MG, Benito FL, Almonacid C, Friedrich Krukenberg of Krukenberg’s Tumour: Report of a series of casesRev Col Gastroenterol 2012 27(2):113-18. [Google Scholar]
[5]. Irving JA, Lerwill MF, Young RH, Gastrointestinal stromal tumours metastatic to the ovary: a report of five casesAm JSurg Pathol 2005 29(7):920-26. [Google Scholar]
[6]. Parkin DM, Bray F, Ferlay J, Pisani P, Global cancer statistics, 2002CA Cancer J Clin 2005 55(2):74-108. [Google Scholar]
[7]. Das S, Sahu D, Wani M, Reddy PK, A curious discourse of Krukenberg tumour: a case reportJ Gastrointest Oncol 2014 5(6):E117-20. [Google Scholar]
[8]. Antila R, Jalkanen J, Heikinheimo O, Comparison of secondary and primary ovarian malignancies reveals differences in their pre- and perioperative characteristicsGynaecol Oncol 2006 101:97-101. [Google Scholar]
[9]. Testa AC, Ferrandina G, Timmerman D, Savelli L, Ludovisi M, Van Holsbeke C, Imaging in gynaecological disease, 1: Ultrasound features of metastases in the ovaries differ depending on the origin of primary tumourUltrasound Obstet Gynaecol 2007 29:505-11. [Google Scholar]
[10]. Tombesi P, Di Vece F, Ermili F, Fabbian F, Sartori S, Role of ultrasonography and contrast-enhanced ultrasonography in a case of Krukenberg tumourWorld J Radiol 2013 5(8):321-24. [Google Scholar]
[11]. Rajshri PD, Kishor HS, David NV, Krukenberg Tumour of the ovary- A CASE reportIndian Journal of Medical Case Reports 2014 3(2):36-39. [Google Scholar]
[12]. Zhang J, Cheng X, Han C, Li Z, Wang M, Zhu Y, Krukenberg tumour in a pregnant patient with severe preeclampsiaExperimental and Therapeutic Medicine 2014 7(6):1476-80. [Google Scholar]