Long Term Patient Satisfaction of Burch Colposuspension with or Without Concomitant Total Abdominal Hysterectomy
Mustafa Ulubay1, Mustafa Ozturk2, Ugur Keskin3, Ulas Fidan4, Fahri Burcin Firatligil5, Ibrahim Alanbay6, Mufit Cemal Yenen7
1 Assistant Professor, Department of Obstetrics and Gynecology, Gulhane Military Medical Academy and Medical School, Etlik, Ankara/ Turkey.
2 Specialist, Medical Doctor, Department of Obstetrics and Gynecology, Etimesgut Military Hospital, Etimesgut, Ankara/ Turkey.
3 Professor, Department of Obstetrics and Gynecology, Gulhane Military Medical Academy and Medical School, Etlik, Ankara/ Turkey.
4 Assistant Professor, Department of Obstetrics and Gynecology, Gulhane Military Medical Academy and Medical School, Etlik, Ankara/ Turkey.
5 Specialist, Medical Doctor, Department of Obstetrics and Gynecology, Gulhane Military Medical Academy and Medical School, Etlik, Ankara/ Turkey.
6 Associate Professor, Department of Obstetrics and Gynecology, Gulhane Military Medical Academy and Medical School, Etlik, Ankara/ Turkey.
7 Professor, Department of Obstetrics and Gynecology, Gulhane Military Medical Academy and Medical School, Etlik, Ankara/ Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mustafa Ulubay, Assistant Professor, Department of Obstetrics and Gynecology, Gulhane Military Medical Academy and Medical School, Etlik, Ankara/ Turkey.
E-mail: mulubay@gata.edu.tr
Introduction
Urinary incontinence negatively affects the quality of life. Various methods are used in the treatment of stress incontinence. Burch colposuspension (BC) is the classical treatment of urinary incontinence.
Aim
To compare the long-term satisfaction in patients receiving BC with or without concomitant total abdominal hysterectomy.
Materials and Methods
One hundred and twenty patients with stress incontinence underwent burch colposuspension with or without concomitant total abdominal hysterectomy. Ninety-three (77.5%) patients were interviewed by telephone. Of these, 91(75, 8%) patients agreed to participate in the study. The patients were divided into two groups according to the type of the surgical procedure. Group 1(N=48, 52.7%) had received burch colposuspension with concomitant total abdominal hysterectomy. Group 2 (N=43, 47.3%) had received burch colposuspension without concomitant total abdominal hysterectomy.
Results
In Group 1, 41 patients (85%) were satisfied with the surgery and did not complain of urinary incontinence (p<0.05). In Group 2, 37 (86%) patients were satisfied with the surgery (p<0.05).
Conclusion
There were no difference in patient satisfaction between hysterectomy and BC and only BC to treat incontinence.
Colposuspansion operation, Long term results, Urinary incontinence
Introduction
According to the International Continence Society (ICS), urinary incontinence is the inability to control urination [1]. The term urocleusia is used to describe urinary incontinence related to stress, which occurs because of physical exertion, such as sneezing, coughing, laughing, and exercising, which causes an increase in abdominal pressure [1]. Because urinary incontinence often occurs in social situations, it negatively affects the quality of life [2]. It is demonstrated that its frequency in female patients ranged widely between 4.5% and 53% [2]. Recent studies showed that several physiopathological or iatrogenic factors were related to the increased frequency of urinary incontinence, including chronic lung diseases, such as Chronic Obstructive Pulmonary Disease (COPD), in addition to constipation, heavy exercise, obesity, gynecological operations, other invasive approaches (e.g., cancer surgery, bladder length surgeries), and normal delivery [3,4].
Various methods are used in the treatment of stress incontinence. In 1949, Marshall-Marchetti-Krantz first defined the surgical operation as the hanging of the periurethral tissues to the symphysis pubis [5]. Subsequently, in 1961, Burch modified the definition to the hanging of the periurethral tissues to the iliopectineal ligament [6]. In 1978, Tanagho suggested the stabilization of instead of the hanging the paraurethral tissues because of complications during postoperative urination after burch colposuspension [7]. In 1991, Vancaillie [8] developed the laparoscopic colposuspension technique, which can also be performed by robotic methods [9,10]. Currently, although Burch colposuspension (BC) is the classical treatment, sling operations are being used to replace this modality [11].
Urgency, frequency, stranguria, and nocturia, are a long-term problem of colposuspension [12]. In this study, we aimed to compare the ratios of the long-term satisfaction of patients in whom BC and total abdominal hysterectomy operations were performed with those of patients in whom burch colposuspension was performed because of stress incontinence.
Materials and Methods
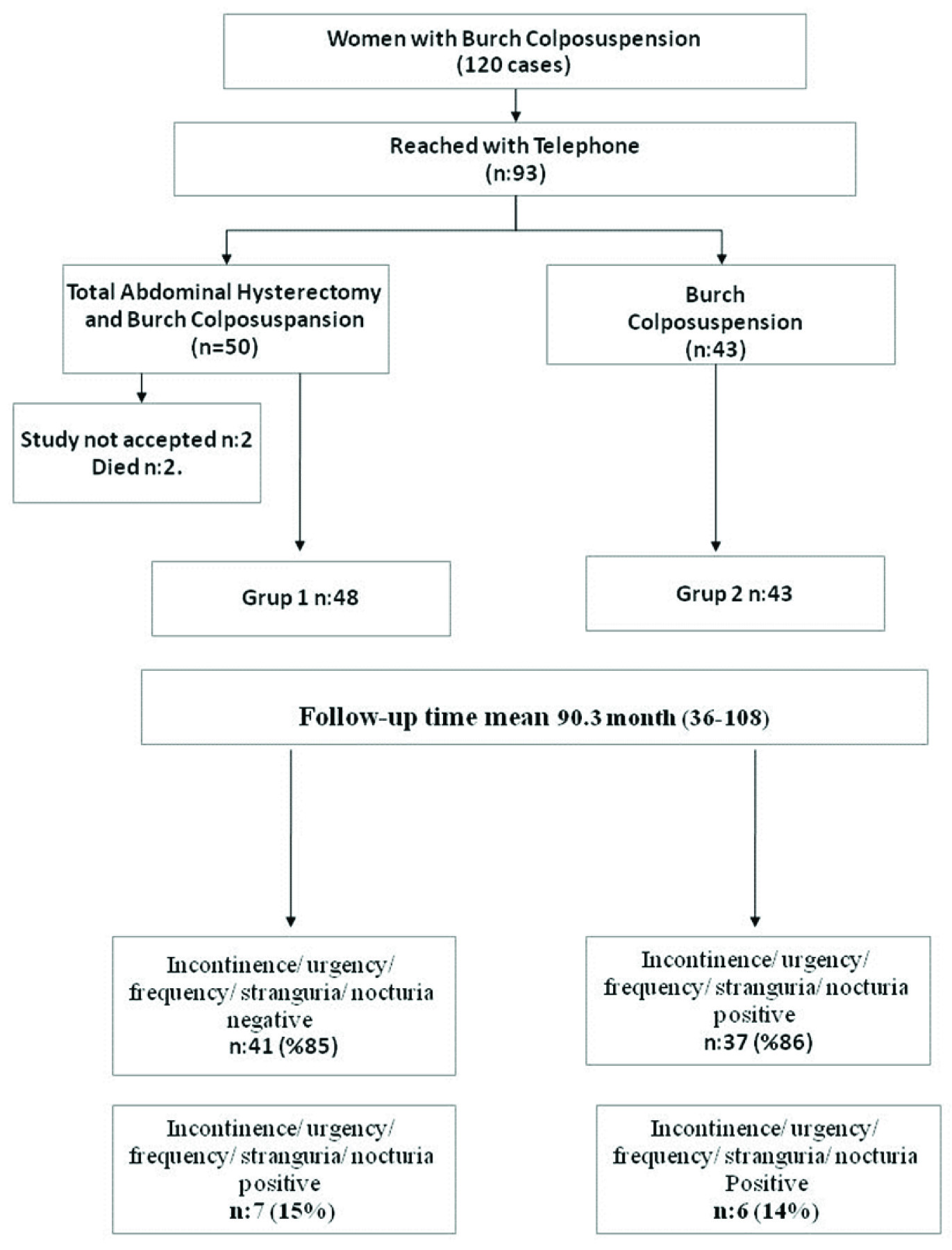
The local ethics committee approved this retrospective study, which included 120 patients with benign gynecological disorders and stress incontinence who underwent BC with or without a concomitant Total Abdominal Hysterectomy (TAH) procedure between January 2004 and January 2012. Ninety-three (77.5%) patients were interviewed by telephone [Table/Fig-1]. After the telephone interviews, 91 (75.8%) patients were divided into two groups, as shown in [Table/Fig-2]. The patients in Group 1 (N = 48, 52.7%) received burch colposuspension with concomitant total abdominal hysterectomy. The patients in Group 2 (N = 43, 47.3%) received burch colposuspension without concomitant total abdominal hysterectomy.
| TAHBC(Group 1 n=68) | BC(Group 2 n=52) |
|---|
| Total patients | 68 (56.6%) | 52 (43.4%) |
| Reached | 50 (73.5%) | 43 (82.6%) |
| Not reached | 16 (23.5%) | 9 (17.3%) |
| Died | 2 (2.9%) | 0 |
| Study accepted | 48 (96%) | 43 (100%) |
| Study not accepted | 2 (4%) | 0 |
In the TAHBC procedure, all patients underwent general anesthesia and endotracheal intubation. A foley’s catheter was inserted into the bladder as a standard procedure. A Pfannenstiel incision was made to access the abdomen. After the hysterectomy procedure was completed, the parietal peritoneum was sutured with 3/0 Vicryl” (Polyglactin 910 Suture, Ethicon Co. USA). The rectus muscles were then separated in the midline. Soft downward pressure behind and lateral to the pubic symphysis provided access to the retropubic space of Retzius. In the dissection of the retropubic space, the bladder neck and Cooper’s ligament were exposed. The bladder neck was identified by the assistant operator’s vaginal palpation of the Foley catheter bulb. In each procedure, two sutures were placed on each side of the urethra (midurethral level) and 2 centimeters above the vagina (not through the vaginal mucosa). Sutures were then placed in both sites in the Cooper’s ligament. The sutures were then tied tension-free, which was helped by placing a gloved hand in the vagina. We used 2/0 Prolene” (Polypropylene Suture, Ethicon Co. USA) non-absorbable surgical sutures. At the end of each surgery, a control cystoscopy was performed to rule out injury to the urinary tract.
In the BC procedure, all patients underwent general anesthesia with endotracheal intubation. As in the TAHBC procedure, a Foley’s catheter was inserted into the bladder. A Pfannenstiel incision was made to access the retropubic space. The rectus muscles were then separated in the midline. Soft downward pressure behind and lateral to the pubic symphysis provided access to the retropubic space of Retzius, care was taken to avoid entry into the peritoneal cavity. In the dissection of the retropubic space, the bladder neck and Cooper’s ligament were exposed. The bladder neck was identified by the assistant surgeon’s vaginal palpation of the Foley catheter bulb. In each procedure, two sutures were placed on each side of the urethra (midurethral level) and 2 centimeters lateral to the urethra (not through the vaginal mucosa). Sutures were then placed in both sites in the Cooper’s ligament. The sutures were tied tension-free, which was helped by placing a gloved hand in the vagina. We used 2/0 Prolene” (Polypropylene Suture, EthiconCo. USA) non-absorbable surgical sutures. At the end of each surgery, a control cystoscopy was performed to rule out injury to the urinary tract.
All patients underwent intraoperative antibiotic prophylaxis with Cefamezin 1000 mg IV flaconsTM (cefazolin) and did not receive additional antibiotics postoperatively. The Foley’s catheter was extracted at 24 hours postoperatively. The patients who agreed to participate in the study were asked to complete a questionnaire by telephone. The questionnaire requested information about demographics, urinary incontinence status, patient satisfaction, and postoperative complications. Patient satisfaction was determined when the patient did not indicate postoperative incontinence.
Statistical Analysis
SPSS software (version 15.0 for Windows evaluation) was used for the data analysis. A Chi-square test was used to compare continuous data between the two groups. A p-value less than 0.05 was considered statistically significant.
Results
The median patient age was 48 (range, 34–70 years), and the mean follow-up time was 88.4 ± 5 (range, 36–108 months). The demographic data of the patients are shown in [Table/Fig-3], and the patients’ satisfaction is shown in [Table/Fig-4].
Demographic data of the patients
| TAHBC(Group 1 n:48) | BC(Group 2 n:43) | Total |
|---|
| Age (year) | 49.7 (44-70) | 46 (34-60) | 48 (34-70) |
| Marital status |
| Married | 44 (92%) | 39 (91%) | 83 (91%) |
| Single | 0 (0%) | 0 (0%) | 0 (0%) |
| Divorced | 4 (8%) | 4 (9%) | 8 (9%) |
| Delivery status |
| Caesaerean | 11 (23%) | 20 (46%) | 31 (34%) |
| Vaginal delivery | 37 (77%) | 23 (54%) | 60 (66%) |
| Nulligravida / nullipara | 0 (0%) | 0 (0%) | 0 (0%) |
| Education |
| Illiterate | 9 (19%) | 2 (4.5%) | 11 (12%) |
| Primary education / high school | 21 (44%) | 24 (56%) | 45 (50%) |
| University | 18 (37%) | 17 (39.5%) | 35 (38%) |
| Chronic disease |
| Cardiac disease | 16 (33%) | 10 (23%) | 26 (29%) |
| Pulmonary disease | 8 (17%) | 4 (9%) | 12 (13%) |
| Other | 24 (50%) | 10 (23%) | 34 (37%) |
| Non | 0 (0%) | 19 (45%) | 19 (21%) |
| Weight (kg) | 71 (50-130) | 64 (50-120) | 69 (50-130) |
| Height (cm) | 157 (150-175) | 158 (150-175) | 157 (150-175) |
| TAHBC(Group 1 n:48) | BC(Group 2 n:43) | p |
|---|
| Follow-up time (month) | 90.3 (36-108) | 88.4 (36-108) | NS |
| Incontinence/urgency/ frequency/ stranguria/ nocturia (-) | 41 (85%) | 37 (86%) | NS |
| Incontinence/ urgency, frequency/ stranguria/ nocturia (+) | 7 (15%) | 6 (14%) | NS |
In group 1, the mean patient age was 49.7 (range, 44–70) years, and the mean follow-up time was 90.3 (range, 36–108) months. In group 2, the mean patient age was 46 (range, 34–60) years, and the mean follow-up time was 88.4 (range, 36–108) months.
The evaluation of the patients in Group 1 showed that 41 patients (85%) were satisfied with the surgery and did not complain of urinary incontinence (p <0.05). The remaining seven patients were not satisfied with the surgery. Four patients complained of continued incontinence, and three patients complained of continued partial incontinence [Table/Fig-1].
The evaluation of the patients in Group 2 showed that 37 patients (86%) were satisfied with the surgery (p <0.05). Six patients indicated that they were not satisfied with the operation, and they complained of continuing incontinence [Table/Fig-1].
Discussion
Urinary incontinence is a common occurrence that negatively affects the quality of life [2]. Stress incontinence is a type of urinary incontinence that is commonly seen in elderly and middle-aged female patients. Its development is caused by weakness in the pelvic base weakness and urethral hypermobility [1]. Because of the increase in the elderly population and the extension of the average life span, the number of cases of urinary incontinence is gradually increasing. Moreover, the extended life span of patients after surgery has increased the importance of the long-term success of the burch colposuspension procedure.
In the treatment of stress incontinence, in addition to medical treatment, various surgical methods that are performed vaginally or suprapubically have been suggested [13]. The main purpose underlying the use of these methods is to correct the distorted urethral angle by locating the urethra in a high retropubic position [14].
In the extant literature, one study compared the satisfaction of patients who had received BC with TAHBC. However, few studies have considered the long-term satisfaction of patients. Most studies used short pursuit periods (<5 years) [15]. However, other studies showed that the rates of failure and relapse after BC increased over time [15]. In a study by Alcalay et al., the pursuit period was 10 to 20 years. In this study, the rates of BC success were evaluated at 69% [16]. In another study performed by Meltomaa et al., the long-term success rates were similar in patients who received abdominal hysterectomy with burch colposuspension and patients who received only burch colposuspension, at 81% and 77%, respectively [17]. Short-term cure rates of 73% to 92% were reported [18]. The effectiveness of this surgical technique persisted over a long term. 5 to 10 years after their surgery, approximately 70% of patients were still continent [12]. In the present study, the results showed that the levels of patient satisfaction with TAHBC and BC were 84% and 86%, respectively.
Eight risk factors that can cause failure after BC were demonstrated [19] : 1) diagnosis not according to ICS standards; 2) incorrect surgical procedure or surgical mistake; 3) previous surgical approaches that caused shortening of the vagina walls and urethra; 4) low preoperative urethral closure pressure (<20 cm H2O); 5) presence of detrusor hyperactivity; 6) preoperative negative ped test; 7) hypoestrogenism related to age; 8) denervation developed during delivery. In our study, postoperative satisfaction was not indicated in seven patients in Group 1 and six patients in Group 2. The patients were called regarding a control examination. The evaluation found incorrect surgical procedures in five patients and hypoestrogenism related to age in two patients who had received TAHBC, which were considered the factors causing failure. In the patients who received BC, detrusor hyperactivity in three patients and incorrect surgical procedure in three patients were the causes of patient dissatisfaction. Nevertheless, the satisfaction rates of 78 patients were evaluated at 85.7%, which indicated that these patients were satisfied with the operations they received.
Limitations
Shortcomings of study; Small sample size limits ability to comment on lack of differences identified in efficacy.
Balancing the limitations with your study’s strengths, we described the long-term outcomes and we provided a helpful report of efficacy and safety for a surgical approach (the Burch) that’s not dead and perhaps making a resurgence given current mesh controversy.
Conclusion
Our study showed high satisfaction rates in both groups in which BC was performed because of stress incontinence. We detected that there is not difference in patient satisfaction between hysterectomy and BC and only BC to treat incontinence.
[1]. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Standardisation Sub-committee of the International Continence Society. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence SocietyNeurourol Urodyn 2002 21(2):167-78. [Google Scholar]
[2]. Hampel C, Wienhold D, Benken N, Eggersmann C, Thüroff JW, Definition of overactive bladder and epidemiology of urinary incontinenceUrology 1997 50(6A Suppl):4-14.discussion 15-17 [Google Scholar]
[3]. Milsom I, Ekelund P, Molander U, Arvidsson L, Areskoug B, The influence of age, parity, oral contraception, hysterectomy and menopause on the prevalence of urinary incontinence in womenJ Urol 1993 149:1459-62. [Google Scholar]
[4]. Drouin J, Tessier J, Bertrand PE, Schick E, Burch colposuspension: Long-term results and review of published reportsUrology 1999 54:808-14. [Google Scholar]
[5]. Marshall WF, Marchetti AA, Krantz KE, The correction of stress incontinence by simple vesicourethral suspensionSurg Gynecol Obstet 1949 88:509-18. [Google Scholar]
[6]. Burch JC, Cooper ’s ligament urethrovesical suspension for urinary stress incontinenceAm J Obstet Gynecol 1968 100:764-72. [Google Scholar]
[7]. Tanogho EA, Colpocystourethropexy. The way we do itJ Urol 1976 116:751-53. [Google Scholar]
[8]. Vancaillie TG, Schuessler W, Laparoscopic bladder neck suspensionJ Laparoendosc Surg 1991 1:169-73. [Google Scholar]
[9]. Khan MS, Challacombe B, Rose K, Dasgupta P, Robotic colposuspension: two case reportsJ Endourol 2007 21(9):1077-79. [Google Scholar]
[10]. Payne TN, Dauterive FR, A comparison of total laparoscopic hysterectomy to robotically assisted hysterectomy: surgical outcomes in a community practiceJ Minim Invasive Gynecol 2008 15(3):286-91. [Google Scholar]
[11]. Schimpf MO, Rahn DD, Wheeler TL, Patel M, White AB, Orejuela FJ, Society of Gynecologic Surgeons Systematic Review Group. Sling surgery for stress urinary incontinence in women: a systematic review and metaanalysisAm J Obstet Gynecol 2014 211(1):71.e1-71.e27. [Google Scholar]
[12]. Eriksen BC, Hagen B, Eik-Nes SH, Molne K, Mjolnerod OK, Romslo I, Longterm effectiveness of the Burch colposuspension in female urinary stres incontinenceActa Obstet Gynecol Scand 1990 69:45-50. [Google Scholar]
[13]. Asıcıoglu O, Gungorduk K, Besimoglu B, Ertas IE, Yıldırım G, Celebi I, A 5-year follow-up study comparing Burch colposuspension and transobturator tape for the surgical treatment of stress urinary incontinenceInt J Gynaecol Obstet 2013 125(1):73-77. [Google Scholar]
[14]. Alan C, Seçkin B, Demirkesen O, Cetinel B, Erten K, Ors AO, Results of the anti-incontinence surgery in female patientsGulhane Med J 2007 49:106-09. [Google Scholar]
[15]. Kjølhede P, Long-term efficacy of Burch colposuspension: a 14-year follow-up studyActa Obstet Gynecol Scand 2005 84(8):767-72. [Google Scholar]
[16]. Alcalay M, Monga A, Stanton SL, Burch colposuspension: a 10–20 year follow upBr J Obstet Gynaecol 1995 102:740-45. [Google Scholar]
[17]. Meltomaa SS, Haarala MA, Taalikka MO, Kiilholma PJ, Alanen A, Mäkinen JI, Outcome of Burch retropubic urethropexy and the effect of concomitant abdominal hysterectomy: a prospective long-term follow-up studyInt Urogynecol J Pelvic Floor Dysfunct 2001 12(1):3-8. [Google Scholar]
[18]. Petri E, Retropubic cystourethropexies. In Textbook of female urology and urogynaecology 2001 1 editionLondonMartin Dunitz;Cardozo L, Staskin D:513-24. [Google Scholar]
[19]. Amaye-Obu FA, Drutz HP, Surgical management of recurrent stress urinary incontinence: A 12-year experienceAm J Obstet Gynecol 1999 181:1296-307. [Google Scholar]