Alcoholism represents a serious health issue with major socioeconomic consequences. Members of armed forces are also not immune to alcohol use disorders. It contributes to 15-20% of all psychiatric admission and many medical, surgical and traumatic emergencies [1]. Different alcohol consumption patterns are linked to variety of health, occupational and social problems which compromise the quality of life of patients [2]. Even in American Armed forces alcohol misuse constitutes problem for significant minority [3].
Alcohol problems are more likely to be overlooked in population where alcohol drinking is ubiquitous and socially accepted. Only 20-50% of patients with alcoholism are identified by physicians who are attending medical care [4,5]. Alcohol consumption data based on self reporting is highly unreliable [6,7] due to underestimation of the actual amount, deliberate falsification, or denial [8,9]. Some knowledgeable patients also mask the withdrawal signs and symptoms by surreptitiously taking ubiquitous benzodiazepines.
No exact clinical findings identify alcohol abuse in early stage. WHO collaboration study found that clinical findings are poor early indicator of alcohol related harm [10]. Diagnosis of alcoholism can be facilitated by series of blood tests. These are state markers for heavy drinking which are observed in patients who regularly ingest alcohol over a prolonged period. Markers help clinicians in deciding possible role in clinical problem or disease process. They only enhance clinical suspicion and must be combined with clinical history (including collaboration history from administrative report) and physical examination. Biological markers are also useful in providing motivational input to patient on follow-up. GGT is a membrane bound enzyme that aids in the transport of amino acids. Serum gamma-glutamyl transferase (GGT) is cheap, highly-sensitive and reliable laboratory test which is frequently used to identify hepatobiliary dysfunction and alcohol abuse [11]. Serum gamma-glutamyl transferase (GGT) has been widely used as an index of liver dysfunction and marker of alcohol intake. The half life of GGT is between 14 and 26 days and after stopping drink it returns to normal level in 4-5 weeks [12]. Marcos placed sensitivity and specificity of GGT for alcohol abuse at 40 to 80% for both [13]. Despite this limitation GGT is useful in confirming the clinical suspicion of alcoholism and monitoring abstinence in recovering person [14].
In the above context it becomes important for us to study and gain our experience with a biological marker, widely accepted and even when used alone can conveniently be used in our lab settings to detect problem drinking and monitoring of rehabilitation and evaluation of treatment programmes in cases of alcohol dependence syndrome. So this study was carried out with an aim of seeing if gamma glutamyl transferase (GGT) can serve the practical utility of firmly establishing alcohol dependence/relapse in Armed Forces patients and aid in fair disposals.
Materials and Methods
An approval was obtained from the Armed forces Research Committee before the commencement of the study. Patients were informed about the details of the study and informed consent was obtained from each participant before undertaking the study. It was a prospective study stretched over a period of 12 months. All consecutive admissions of alcohol dependence admitted into psychiatric ward of a zonal hospital satisfying the International Classification of Diseases ICD-10 criteria for alcohol dependence syndrome (F10.2) were included in the study and blood sample were drawn from them next morning to estimate GGT levels. Cases with liver and billiary tract disease, pancreatitis, renal decompensation and on treatment with drugs like phenytoin and phenobarbitone were not included in the study. After the treatment they were placed in low medical category for 12 weeks, to facilitate more frequent monitoring. Thus GGT was repeated at the end of 3 months, 6 months, 9 months and 12 months after the initial treatment. The self-report, units report and ward observations were noted for the assessment. However, psychiatrist’s assessment was the gold standard against which the biochemical marker was evaluated. The period of monitoring in each case was a minimum of six and a maximum of 12 months, depending upon at which point of the study period a particular case reported initially. Total 52 cases were studied. GGT estimation was done by colorimetric method using commercial kits. Cut off for the GGT was worked out using ROC analysis. ROC analysis was used to assess the performance of GGT across the full range of potential cut off values [15] at index admission; 6 months and 12 months follow-up.
ROC curves plot a scales ability to detect the positives (e.g. persons correctly classified as alcohol dependence syndrome) against the rate of false positives (e.g. persons incorrectly classified as alcohol dependence syndrome). Perfect discrimination is indicated by the score of 1.0 and the chance performance by the score of 0.5. Paired ’T’ test was used to assess the significance of difference of mean GGT at the index admission, 3 months, 6 months, 9 months and 12 months follow-up in relapse and the abstinent groups.
Results
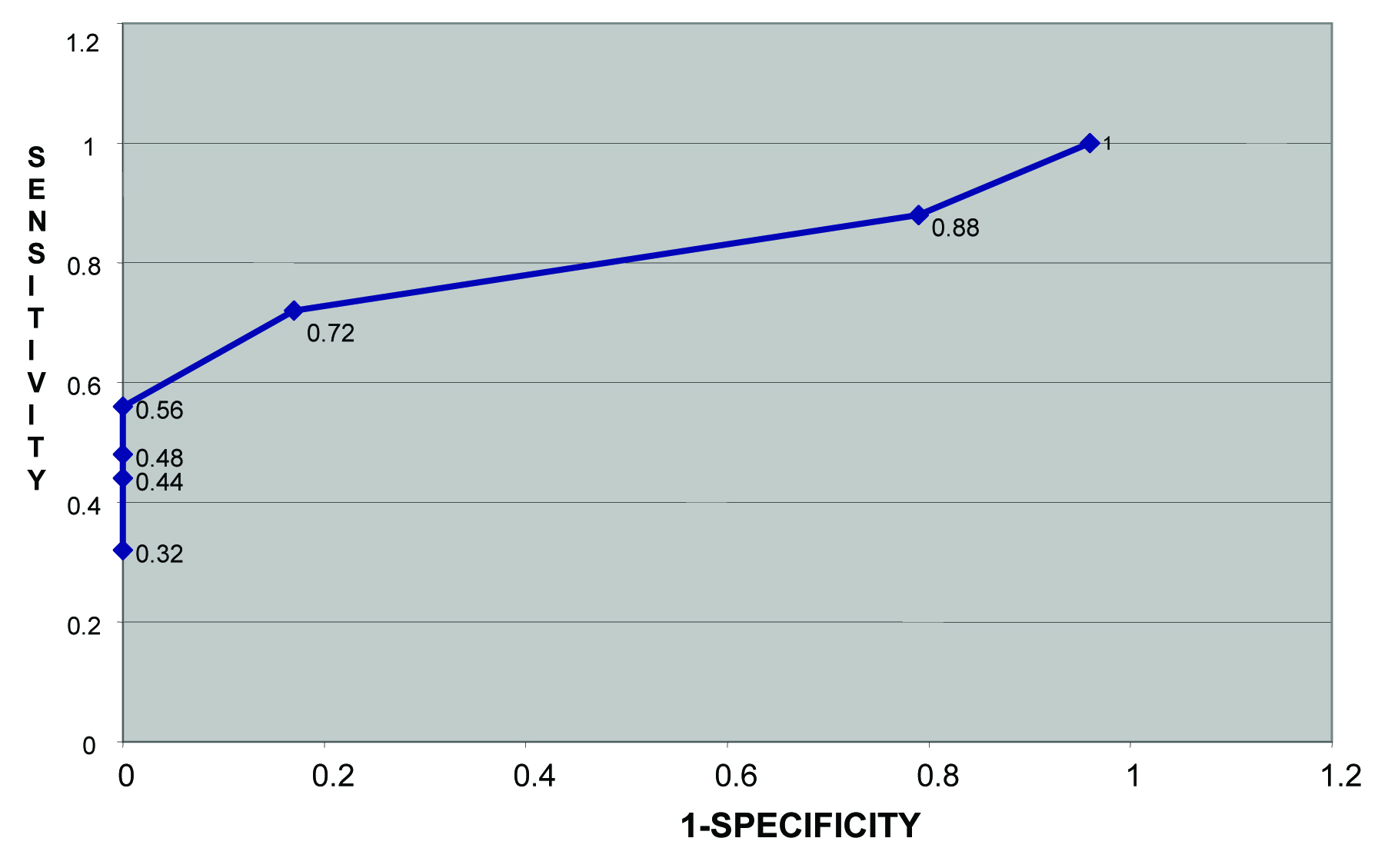
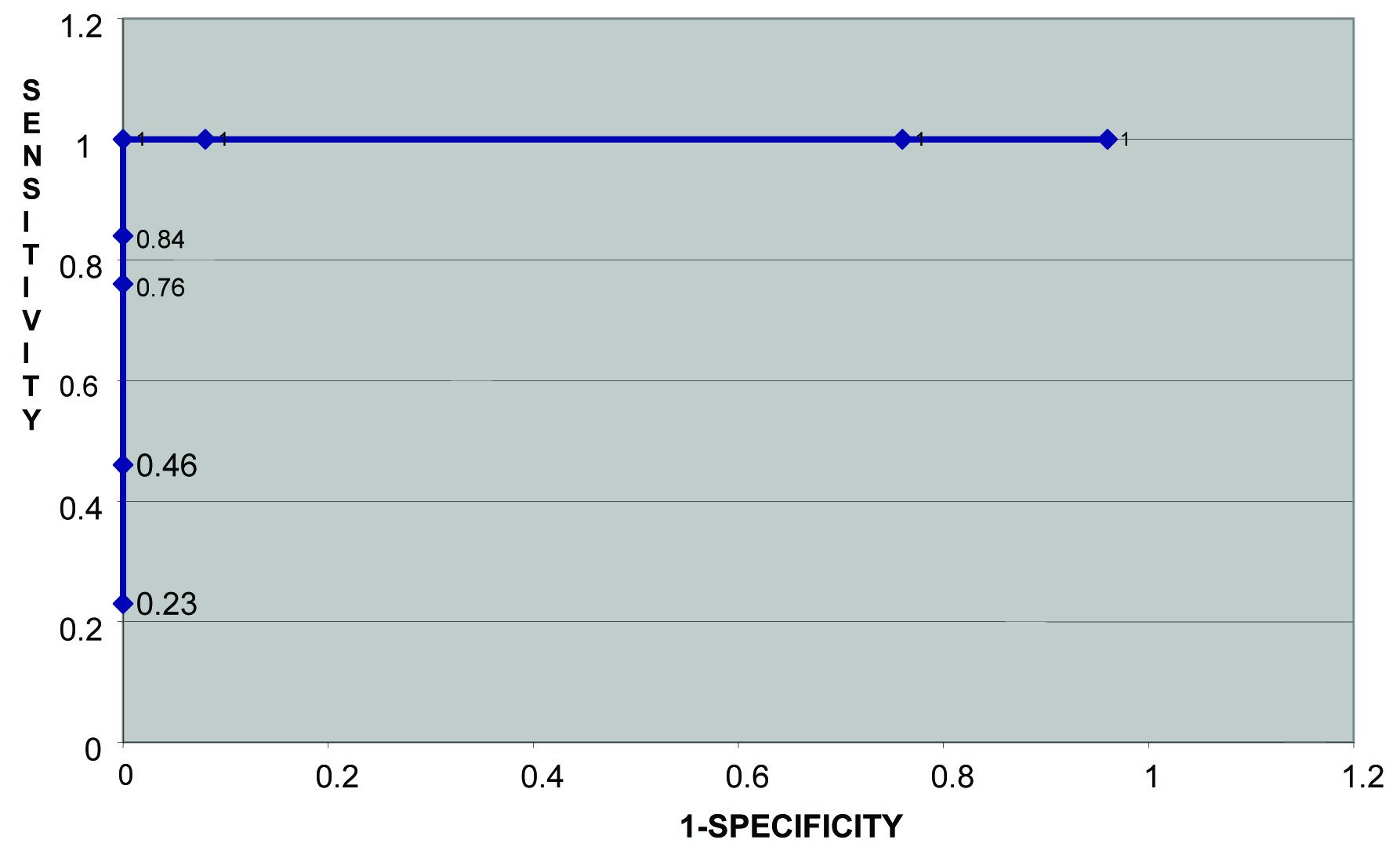
Fifty two cases of alcohol dependence syndrome after initial assessment were followed up at 3, 6, 9 and 12 months interval. All cases were male with mean age of sample 34 years and range 24–45 years. Mean duration of drinking was 9.5 years. As per the clinical judgment number of clinically asymptomatic cases at 0 month, 3 months, 6 months, 9 months and 12 months was 48%, 86% 73%, 65% and 78% respectively. Mean GGT of sample 55.52 IU/L, range 19-455 IU/L and median value was 37 IU / L. The normal values are 0 to 39 IU/L. The cut-off value of GGT was worked out with the help of [Table/Fig-1,2,3,4,5 and 6] which shows the sensitivity/specificity of GGT at the corresponding period on admission, 6 months and 12 months.
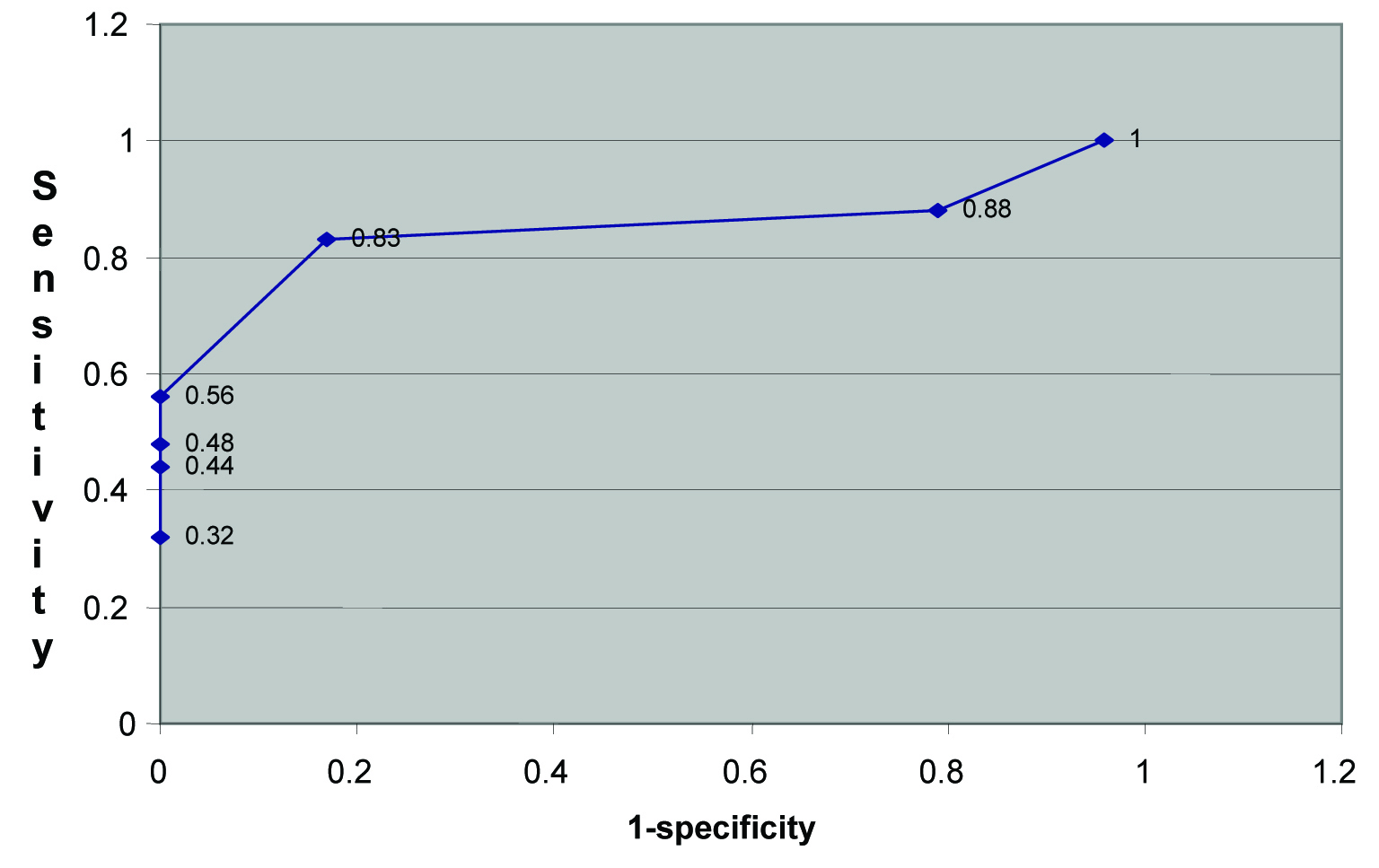
Specificity, Sensitivity and 1-sp at admission
| GGT Level | Specificity | Sensitivity | 1-Sp |
|---|
| GGT 20 | 0.042 | 1 | 0.958 |
| GGT 30 | 0.21 | 0.88 | 0.79 |
| GGT 40 | 0.72 | 0.83 | 0.17 |
| GGT 50 | 1 | 0.56 | 0 |
| GGT 60 | 1 | 0.48 | 0 |
| GGT 70 | 1 | 0.44 | 0 |
| GGT 80 | 1 | 0.32 | 0 |
Specificity, Sensitivity and 1-sp at 6 months
| GGT Level | Specificity | Sensitivity | 1-Sp |
|---|
| GGT 20 | 0.04 | 1 | 0.96 |
| GGT 30 | 0.21 | 0.88 | 0.79 |
| GGT 40 | 0.83 | 0.72 | 0.17 |
| GGT 50 | 1 | 0.56 | 0 |
| GGT 60 | 1 | 0.48 | 0 |
| GGT 70 | 1 | 0.44 | 0 |
| GGT 80 | 1 | 0.32 | 0 |
Specificity, Sensitivity and 1-sp at 12 months
| GGT Level | Specificity | Sensitivity | 1-Sp |
|---|
| GGT 20 | 0.04 | 1 | 0.96 |
| GGT 30 | 0.24 | 1 | 0.76 |
| GGT 40 | 0.92 | 1 | 0.08 |
| GGT 50 | 1 | 1 | 0 |
| GGT 60 | 1 | 0.84 | 0 |
| GGT 70 | 1 | 0.76 | 0 |
| GGT 80 | 1 | 0.46 | 0 |
| GGT 90 | 1 | 0.23 | 0 |
The difference among mean GGT levels on admission, 3 months, 6 months, 9 months and 12 months in clinically symptomatic and asymptomatic group reached statistically significant position (p<0.05) and distinguished relapsed and abstinent group. [Table/Fig-1] shows the sensitivity and specificity at different levels of GGT at first admission. It will be seen from the figure that at the level GGT 50 IU/L specificity is 1 and sensitivity is 0.56. Similarly, the ROC curve on first admission [Table/Fig-1,4] indicates the cut off for GGT at 50 IU/L where 1-sp =0 and sensitivity is 0.56. Similarly, [Table/Fig-2,5] also indicate cut-off levels at 50 IU/L as most appropriate.
In [Table/Fig-3], the sensitivity and specificity at 12 months follow-up are both 1 at GGT levels of 50 – an ideal situation. GGT 50 should be taken as the cutoff point. The ROC curve at 12 months [Table/Fig-3,6] further confirms this view where the point where 1-sp=0 and sensitivity = 1 corresponds to GGT 50.
Discussion
A marker should easily be able to indicate chronic ingestion (screening marker) and acute ingestion (relapse marker) of alcohol. A screening marker should display high sensitivity and specificity and should distinguish between safe social drinking and problem drinking. The marker should not be elevated by non alcohol induced organ damage and should be non invasive. A marker used to depict relapse should be sensitive at any consumption above safe levels. No such marker exists in present.
GGT is inexpensive, easy and convenient test which can be routinely performed after phlebotomy when blood is drawn for assessing liver function test and other metabolic parameters. It remains the most commonly used marker for indicating acute alcohol-induced liver damage [16]. Though, carbohydrate deficient transferring is more sensitive and specific than GGT in detecting relapse and recovery from alcohol use disorder but is more complex, costly and has long turnaround time than GGT [17]. The major limitation of GGT is that it is affected by liver disease of any cause and several medications including antiepileptic drugs and anticoagulants can give false positive result [18]. Diagnostic accuracy of GGT can be enhanced by combination with other traditional markers (AST, ALT, and MCV) [19]. There have been few Indian publications examining the effectiveness of GGT estimations either singly, or more particularly, serially, in assessing relapse and recovery in patients with established alcohol dependence. In the peripheral hospitals of Armed forces distributed in North, Northeast or Western borders GGT will be easy, convenient and readily performed.
The cut-off values of GGT levels for diagnosis of alcoholism has been worked out with the help of [Table/Fig-1,2,3,4,5 and 6]. The level GGT 50 IU/L specificity is 1 and sensitivity is 0.56 is the most appropriate cut off point as when one wants to be very sure of the diagnosis, one should have negligible false positive result which can only be assured with a test with 100% specificity. Anton in 497 males using 54 U/l as cut off reported sensitivity as 65% and specificity as 89% in cases of dependence [20]. Rinck et al., reported in 242 males sensitivity and specificity of 53.5% and specificity of 97.5 % in cases of dependence at cut off levels of 54 units /L [21]. Sillanaukee and Olsson observed that GGT presented a sensitivity of 59% and a specificity of 91% for identifying alcohol abuse [22].
In ROC [Table/Fig-1] at lower cut off levels of 40 IU/L sensitivity rises but specificity falls. However, it would be inappropriate in armed force scenario as it would adversely affect the service, promotion and pension prospects of the individual. In a suspected case of alcoholism a false positive test due to lower specificity can have adverse social and stigmatizing consequences [23–25].
The clinician must weigh the relative importance of the sensitivity and the specificity of a biological marker and interpret the test result in that context. Benefit of doubt should always go to the individual. Implications of possible errors should always be considered. Since false positive result must be avoided in doubtful cases of alcoholism, cut off levels with high specificity is more desirable. No doubt some cases of alcoholism will be missed at higher level but increasing the sensitivity by lowering the cut off value of marker will increase the false positive results by decreasing the specificity. As the implications for being labeled as alcoholic are serious, it is preferably to have test and cut off levels at high specificity in case of alcohol dependence syndrome.
In the present study GGT levels significantly distinguished the relapse and abstinent group at index admission (p<0.5). This also depicted suitability of GGT in evaluating relapse and recovery in assessing success of treatment programme. The treatment outcome of alcohol dependence syndrome in present study at six months and twelve months follow up was higher at 73% and 78% of success rate. This could have been due to the regular review of the cases at 3 months intervals and the improved education of the recovering alcoholic through objective corroboration of the biological marker. Both these factors would have helped patient to remain motivated towards the abstinence. It would be interesting to see if these results can be replicated in multicentric study.
The majority of studies on biochemical markers for detection of alcohol use disorders have been done in Europe, North America and Australia [15]. It is difficult to compare these studies due to different study design and subject characteristics as well as varied assay methods, threshold used to define excessive drinking and test cutoffs. In Armed forces setting a multicentric study needs to be undertaken to examine performance of the GGT as a marker in different ethnic and racial groups to measure baseline variations as GGT levels are influenced by body mass index and age [26] unaccounted in current study.
Cases were diagnosed as alcohol dependence syndrome based on criteria laid by ICD 10. Psychiatrist assessment was the gold standard against which the GGT as a screening test was evaluated. The need of biological marker was a felt need as diagnosis of alcohol dependence has serious implications on the soldier’s job, pension and promotion and there is always a threat of litigation. A biological marker with reasonably good specificity and sensitivity will help to objectively corroborate relapse in alcohol dependence and will aid in fair disposal of cases. GTT in isolation - nor any single parameter for that matter - can confirm or refute - they can only aid in diagnosis. Ultimately each case has to be determined on its merits based on the clinical profile. The present findings at a particular cut off value of GGT have given a particular sensitivity and specificity. However, the 95% CI indicates the precision of these estimates - the wide interval indicates that a larger sample size in future studies should resolve these issues.
Limitations
Our study had certain limitations. It was purely an exploratory and descriptive study. No hypothesis testing was involved. Therefore, no a prior sample size calculations were undertaken on inputs such as Type I and Type II errors. The sample size was determined by the total number of patients of alcohol dependence reporting during the study period. The findings however, have been reported with 95% CI, given the fixed sample size obtained in the study.
Conclusion
Though not ideal GGT can serve as biological marker in establishing alcohol dependence syndrome in armed forces to aid in fair disposal of cases. It helps in providing motivational inputs to patients. Clinician should pay due consideration to clinical profile, ward observation and unit or administrative report as the diagnosis of alcohol dependence syndrome has serious implications towards service prospects of a soldier.