The clinical picture and risk factors are decisive in differential diagnosis. It was proved that patients with metabolic syndrome have increased incidence of malignant tumours. The visceral adipose tissue releases active proteins that promote oncogenesis. We are presenting a case of 34-year-old male with metabolic syndrome suffering from pain in left iliac fossa with accompanying variable stool pattern. At first, the sigmoid diverticulosis was suspected. Patient’s condition after the treatment has improved. The ambulatory, partial colonoscopy revealed a cauliflower-like, balloting, wide-base growth in the sigmoid that narrowed its lumen. The biopsy did not reveal atypical growth characteristics. Because of tumour type and enlarged regional lymph nodes seen in abdomen CT scan, the segmental colon resection and end-to-end anastomosis was performed in the area of sigmoid-rectal junction. Macroscopically, there were no visible metastases in the operation field. The surgery and postoperative period ran without any complications. On histopathological examination, the removed tumour was a well differentiated liposarcoma (WDL) stemming unusually from adipose tissue of colonic submucosa in an obese male. WDL is a hard to diagnose tumour, especially in early stages of its growth. In the presented case, the tumour was completely resected.
Liposarcoma sigmae, Subacute bowel obstruction, Total tumour resection, Young men
Case Report
A 34-year-old male patient, with no addictions, presented with complaints of pain in left iliac fossa with accompanying flatulence and constipation. His stool pattern was regular. He did not report fever, weight loss, or blood in his feces. He was hypertensive and on regular medication (betaxolol, amlodipine, and atorvastatin) for the past 5 years. He fulfilled the criteria of metabolic syndrome, as like his parents. According to guidelines from the National Heart, Lung, and Blood Institute and the American Heart Association metabolic syndrome is diagnosed when a patient has at least 3 of 5 conditions. The patient meets the four following criteria: 1) Blood pressure ≥ 130/80 mmHg (or drug therapy for hypertension); 2) Triglycerydes ≥ 150 mg/dL; 3) HDL-C ≤ 40 mg/dL in men; 4) Waist circumference ≥ 102 cm, but does not meet the criterion fasting glucose ≥ 100 mg/dL.
On examination the patient was in good general condition, circulatory and respiratory function normal. Abdomen slightly flatulent, peristalsis increased, tenderness on palpation of left iliac fossa, peritoneal signs absent. Per rectum examination and laboratory results were within normal limits. In the abdomen ultrasound, a thickened colon wall up to 22 mm was observed on the length of 60 mm of descending colon, signs of liver steatosis, and enlarged spleen (135x80 mm).
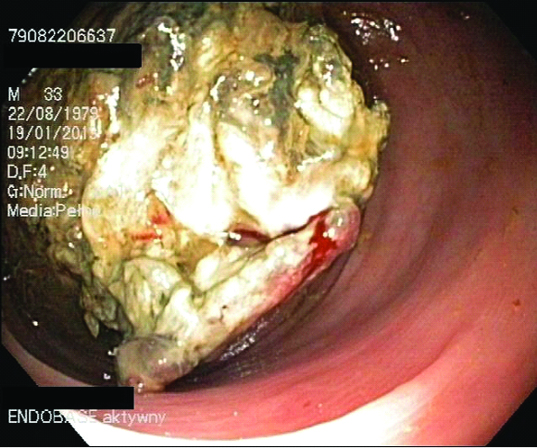
Initially, based on clinical picture and biochemical analyses, sigmoid diverticulosis was suspected, with non specific colitis, tumour of the descending colon and renal colic considered in differential diagnosis. Oral mesalazine 2x1.0 g, rifaximin 2x0.4 g, and alverine 3x0.06 g were ordered, together with low residue diet (Ensure 3x3 spoons), and continued hypertension treatment. Patient’s condition improved, the pains in left iliac fossa regressed, with continued tendency for constipation. Ambulatory colonoscopy was recommended and performed – during the procedure, at approximately 30 cm from anal sphincter, there was a balloting, slightly movable tumour blocking the colon lumen, not allowing the endoscope to be inserted further through the narrowing [Table/Fig-1]. Numerous samples for histopathological examination were taken. Histopathologic findings: tissues necrotic, infiltrated with granulocytes, fragments of nonspecific granulation and little shreds of colonic mucosa with normal continuity and structure. Atypical growth was not observed on examination.
First colonoscopy - a balloting, slightly movable tumour blocking the colon lumen
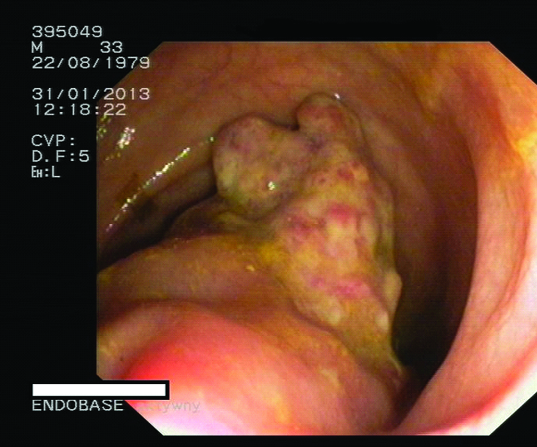
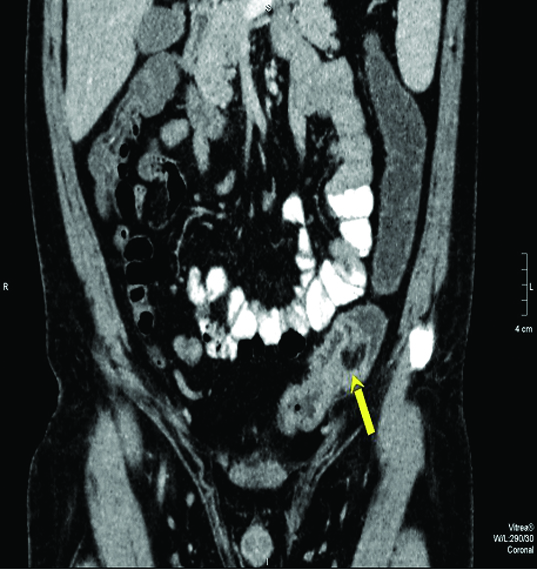
Due to the difference between colonoscopy results and histopathologic findings, immediate observation in gastrological unit was recommended. Second colonoscopy was performed. In the sigmoid there was an exophytic structure stemming from wide, short pedicle, partially amputated with marked decay, providing a better passage. A flat ulceration was visible near the base, numerous samples were again obtained [Table/Fig-2]. Abdomen CT: circular infiltration of descending colon on the length of 65 mm. Its wall irregularly thickened up to 10-17 mm. The tumour was growing cauliflower-like, towards the lumen [Table/Fig-3]. Neighbouring adipose tissue slightly infiltrated, small lymph nodes inside, the largest having 10.6x7.4 mm. In the intestinal mesentery of left iliac fossa there were a few lymph nodes, the largest measuring 16 x 9 mm. Chest x-ray normal.
Second colonoscopy - an exophytic structure stemming from wide, short pedicle, partially amputated with marked decay and near its base
Contrast-enhanced computed tomography of the abdomen showing a circular infiltration of descending colon on the length of 65 mm, wall irregularly thickened up to 10-17 mm (longitudinal section)
The patient qualified for surgery. Tumour resection and end-to-end anastomosis was performed in the area of sigmoid-rectal junction. Macroscopically, there were no visible metastases. The surgery and postoperative period ran without any complications.
Histopathological examination
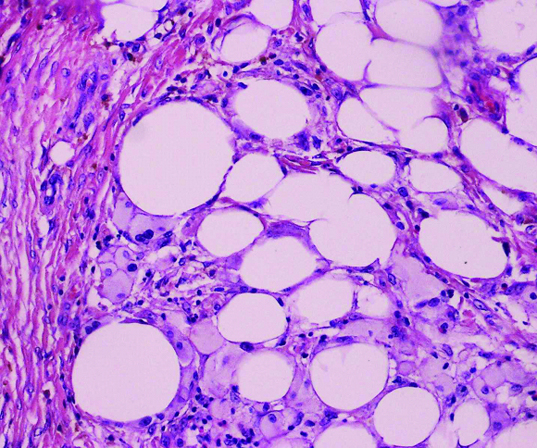
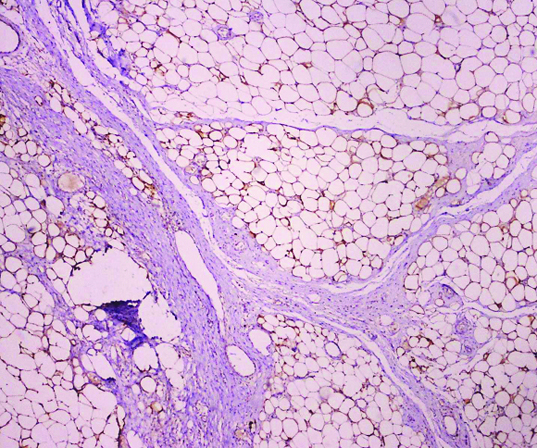
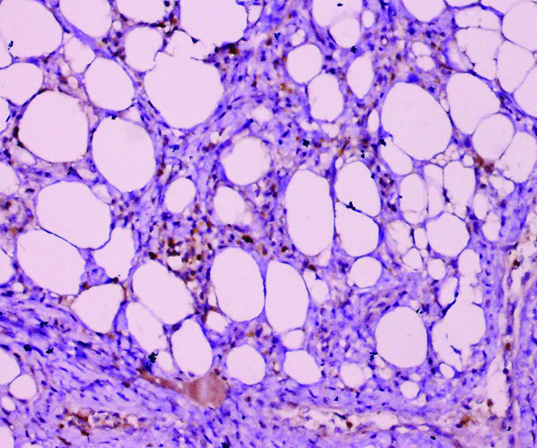
Macroscopically, part of sigmoid colon measuring 22 cm in length with 40x25x25 mm tumour mass located 3 cm from the stump, ulceration in its upper part. Histological findings have confirmed that the tumour did not spread outside the colon wall, which was suggested by CT scans. Microscopically, the tumour consists mainly of adipose tissue segmented by partitions made of connective tissue, with nearby adipocytes having distinct hyperchromatic nuclei [Table/Fig-4]. Atypical cells have positive S-100 antibody immunohistochemical reaction [Table/Fig-5] and Ki-67 stain resulting from proliferative activity [Table/Fig-6]. Based on those characteristics, the lesion should be classified as a WDL-type tumour. The lesion is of unusual location. Less than 50 such cases of primary mesenteric liposarcoma have been reported to data, and very few cases of liposarcoma of the transverse and the descendens mesocolon have been reported [1].
Histopathological examination findings (H&E; 200X).
Histopathological examination findings – tumour cells were positive for S-100; magnification ×100
Histopathological examination findings – tumour cells were positive for the proliferation marker Ki-67; (200X)
Discussion
Metabolic syndrome is not only a significant risk factor of cardiovascular diseases. Increased incidence of cancer was observed in this group of patients, as based on many cohort analyses [2]. The key role in oncogenesis plays visceral adipose tissue releasing para- and endocrine factors, especially in terms of insulin resistance, secondary hyperinsulinemia, and increased release of insulin-like growth factor [3]. Additionally, transforming growth factor (TGF), IL-6, IL-8 and vascular endothelial growth factor (VEGF) released by adipocytes stimulate angiogenesis, ensuring uncontrolled tumour growth [4]. In the presented case, WDL originating from adipose tissue of descending colon was connected with visceral obesity of the patient. Up-to-date available data does not report WDL location in the colonic wall. Liposarcoma is one of the most often diagnosed soft tissue sarcomas in adults. Usually, well differentiated liposarcoma is observed in the thoracic wall or limbs. Due to the clinical course was why it was proposed to be termed atypical lipomatous tumour (ALT) for liposarcomas originating from thoracic wall and limbs, and WDL for tumours originating from abdominal or mediastinal retroperitoneal space [5]. Histologically, there are three subtypes of liposarcomas: well differentiated liposarcoma, myxoid liposarcoma, and pleomorphic liposarcoma. Initially, to diagnose well differentiated liposarcoma, one should have observed lipoblasts with multiple vacuoles. In case of WDL, cytogenetic examination shows a giant ring and q12-15 marker chromosomes [6].
Liposarcoma most often occurs in middle-aged individuals a 34-year-old male in this case. Available data on patients with diagnosed WDL in retroperitoneal space indicates that local tumour growth is very advanced at the time of diagnosis, and symptoms reported by the patient are nonspecific [7]. Vague abdominal symptoms and increased abdominal circumference resulting from large tumour mass are the most common complaints observed in 60-80% of cases. Moreover, other associated symptoms are acute or subacute intestinal obstruction, early satiety or gastrointestinal bleeding [8]. It is said that the most valuable imaging in diagnosis of WDL is magnetic resonance, with 100% sensitivity and 83% specificity [9]. In our patient, the local tumour growth into the lumen of descending colon caused abnormal passage of feces therein. There were pains in the left iliac fossa, flatulence and constipation. Initial tests included abdomen ultrasound (a thickened, irregular wall of descending colon). Bioptic samples obtained from the tumour during colonoscopy did not suggest a neoplastic process. Hence, imaging was complemented with abdomen CT. Cauliflower-like tumour growth, and enlarged nearby lymph nodes suggested surgical treatment. It was important that in this patient, the resection was successfully performed within the area of healthy tissues. Completeness of tumour resection affects chances recurrence and life expectancy. These are also decided by histological malignancy and location. The prognosis is most favourable in ALT, as those tumours can be removed within wide margin of healthy tissues, and the worst in case of poorly differentiated liposarcoma, because in spite of aggressive surgical treatment, local recurrence occurs in approximately 80% of patients and distant metastases are observed in 18% of cases, most often in liver and lungs [10]. Successful complete resection of retroperitoneal liposarcoma may increase the 5-year survival rate from 16.7 to 58% [11]. Repeating recurrences, may lead to renal failure, circulatory and respiratory insufficiency, or sepsis depending on localization. Intramuscular liposarcomas histologically resembling normal subcutaneous adipose tissue, even when deeply localized, are not prone to recurrence, as opposed to those localized within skeletal muscles. Both radio and chemotherapy do not improve survival rates in patients with poorly differentiated liposarcoma. In the presented case, although WDL was removed within wide margin of healthy tissues, endoscopic surveillance was exercised.
Conclusion
Obese patients require particular oncologic supervision. WDL is a neoplasm hard to diagnose in early stage of its growth. There are no known reports of its localization in colon. In the patient with diagnosed metabolic syndrome, the tumour stemmed from submucosal adipose tissue of sigmoid colon, into its lumen, causing symptoms of subacute bowel obstruction. Therefore, it was possible to diagnose the lesion at the stage allowing its complete resection.
[1]. Sachidananda S, Krishnan A, Ramesh R, Kuppurao S, Primary multiple mesenteric liposarcoma of the transverse mesocolonAnn Coloproctol 2013 29(3):123-25. [Google Scholar]
[2]. Mazzarella L, Why does obesity promote cancer? Epidemiology, biology, and open questionsE cancer medical science 2015 9:554 [Google Scholar]
[3]. Rosenquist KJ, Massaro JM, Pedley A, Long MT, Kreger BE, Vasan RS, Fat quality and incident cardiovascular disease, all-cause mortality, and cancer mortalityJ Clin Endocrinol Metab 2015 100(1):227-34. [Google Scholar]
[4]. Ebadi M, Mazurak VC, Evidence and mechanisms of fat depletion in cancerNutrients 2014 6(11):5280-97. [Google Scholar]
[5]. Evans HL, Soule EH, Winkelmann RK, Atypical lipoma, atypical intramuscular lipoma, and well differentiated retroperitoneal liposarcoma: a reappraisal of 30 cases formerly classified as well differentiated liposarcomaCancer 1979 43:574-84.[PMID: 421182] [Google Scholar]
[6]. Fletcher CD, Akerman M, Dal Cin P, de Wever I, Mandahl N, Mertens F, Correlation between clinicopathological features and karyotype in lipomatous tumours. A report of 178 cases from the Chromosomes and Morphology (CHAMP) Collaborative Study GroupAm J Pathol 1996 148:623-30.[PMID: 8579124 PMCID: PMC1861666] [Google Scholar]
[7]. Wiewiór M, Pardesla M, Kobielski A, Particular case of giant recurrent retroperitoneal liposarcomaWiad Lek 2006 7-8:577-78. [Google Scholar]
[8]. Neuhaus SJ, Barry P, Clark MA, Hayes AJ, Fisher C, Thomas JM, Surgical management of primary and recurrent retroperitoneal liposarcomaBr J Surg 2005 92:246-52.[PMID: 15505870] [Google Scholar]
[9]. Gaskin CM, Helms CA, Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty massesAJR Am J Roentgenol 2004 182:733-39.[PMID: 14975977] [Google Scholar]
[10]. Qiao MZ, Li CL, Analysis of prognostic factors associated with primary retroperitoneal sarcomaBull Cancer 2007 94(1):E5-7. [Google Scholar]
[11]. Lee SY, Goh BK, Teo MC, Chew MH, Chow PK, Wong WK, Retroperitoneal liposarcomas: the experience of a tertiary Asian centerWorld J Surg Oncol 2011 9:12doi: 10.1186/1477-7819-9-12. PubMed PMID: 21284868 [Google Scholar]