Incidentally Detected Testicular Metastasis in a Case of Prostatic Adenocarcinoma
Sowmiya Sampathrajan1, Garima Garg2, Sweety Gupta3, Shailesh Chandra Sahay4, Sudarsan De5
1 Senior Resident, Department of Radiation Oncology, Pushpanjali Crosslay Hospital, Galaxy Cancer Institute, Vaishali, Ghaziabad, Uttar Pradesh, India.
2 Consultant, Department of Pathology, Pushpanjali Crosslay Hospital, Galaxy Cancer Institute, Vaishali, Ghaziabad, Uttar Pradesh, India.
3 Consultant, Department of Radiation Oncology, Pushpanjali Crosslay Hospital, Galaxy Cancer Institute, Vaishali, Ghaziabad, Uttar Pradesh, India.
4 Senior Consultant, Depatment of Urology, Pushpanjali Crosslay Hospital, Galaxy Cancer Institute, Vaishali, Ghaziabad, Uttar Pradesh, India.
5 Senior Consultant, Department of Radiation Oncology, Pushpanjali Crosslay Hospital, Galaxy Cancer Institute, Vaishali, Ghaziabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sowmiya Sampathrajan, Pushpanjali Crosslay hospital, Galaxy Cancer institute, W-3, Sector-1 Vaishali, Ghaziabad, NCR, Uttar Pradesh- 201012, India.
E-mail: doctorsowmiyapgi@gmail.com
Adenocarcinoma of the prostate is one of the common cancers among elderly men worldwide. However, testicular metastasis detected incidentally after orchiectomy is a rare presentation as most commonly we encounter patients presenting with bone metastasis at the time of primary diagnosis. Here, we describe a recently diagnosed case of prostatic carcinoma that had metastasis in a single testis, incidentally detected in the orchiectomy histopathological specimen, performed for surgical castration and emphasize the importance of routine microscopical examination of the testicular specimens.
Orchiectomy, Prostate, Unilateral
Case Report
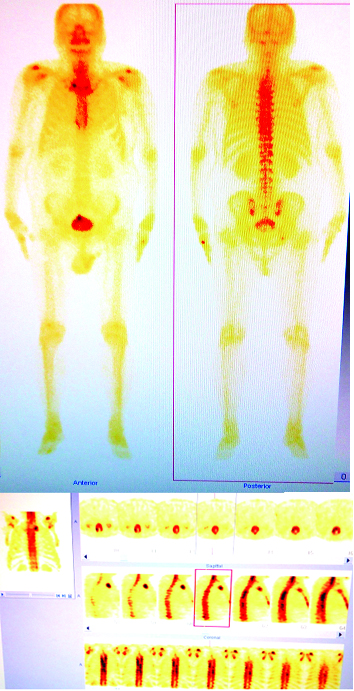
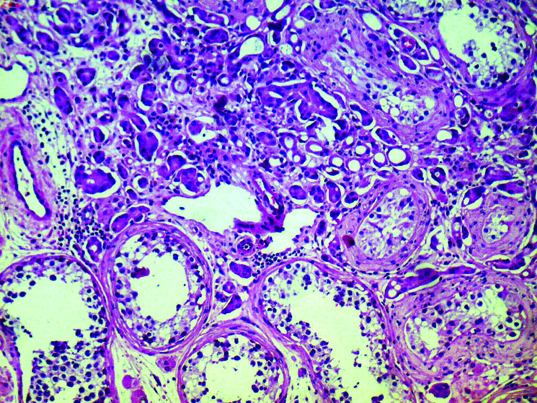
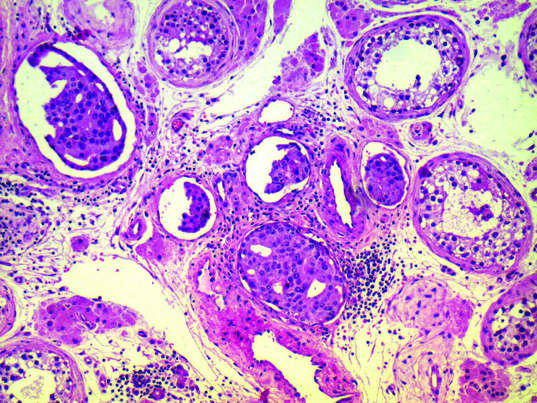
A 63-year-old male presented in the Urology department with symptoms of difficulty in micturition for which he was investigated with Ultrasound Kidney-urinary bladder (USG KUB) and found to have enlarged prostate. Serum prostate specific antigen (PSA) was 225.49 ng/ml at presentation and Tru-cut biopsy from both lobes of prostate reported acinar adenocarcinoma prostate, with tumour involving 65% of submitted tissue with peripheral invasion and Gleason’s score (GS = 4+4) = 8. Magnetic Resonance Imaging (MRI) of Pelvis showed enlarged prostate measuring 49x39 mm with nodular enlargement of central zone and T2W hyper intense signal in peripheral zone without any peri-prostatic extension and a small lymph node 7mm in right external iliac region. He underwent Radionuclide Technetium (99m TC- MDP) bone scan which showed skeletal metastasis involving twelfth dorsal (D12) vertebrae and right ischium [Table/Fig-1]. The patient was advised for androgen deprivation therapy (ADT) and he opted for surgical castration. He underwent bilateral orchiectomy and histopathology reported to be metastatic adenocarcinoma of right testis [Table/Fig-2] and the resection margin of right spermatic cord showed lymphovascular invasion [Table/Fig-3]. The other testis was absolutely normal. His serum PSA started falling, 134.84 ng/ml after 1 month of orchiectomy and he was started on hormonal therapy and palliative radiation to the bony metastatic sites.
Radionuclide (99m Tc – MDP) Bone scan showed skeletal metastases involving D12 vertebra and right Ischium with degenerative changes of few other areas
Malignant glands and single cells seen infiltrating in between the seminiferous tubules (200X magnification); H&E
Extensive lymphovascular invasion seen (200X magnification); H&E
Discussion
The most commonly encountered metastatic sites in a case of prostatic adenocarcinoma are bone (84%), distant lymph nodes (10.6%), liver (10.2%), and thorax (9.1%) [1]. Testicular metastases are very rare, and most of them are incidental findings in 2–4% of orchiectomy specimens performed for hormonal management of advanced prostate carcinoma [2]. The first case of prostate carcinoma metastasizing to the testis was reported by Semans in 1938 [3]. Prostatic carcinoma metastasizing to the testis is commonly accepted as a sign of advanced disease and it is usually accompanied by multiple metastases to other organs, and unfortunately it is a silent phenomenon [4]. However, the prognostic significance of metastasis with testicular localization is still unknown. Our’s is a case of newly diagnosed prostatic cancer with silent testicular metastasis.
Most of the patients with testicular metastases tend to be older (in the sixth or seventh decade of life) than the patients with primary testicular germ cell neoplasms. Metastasis has been reported to be unilateral mostly but also bilateral in a small proportion of cases [5]. In Korea, Kim et al., had reported a case of prostate cancer with solitary metastases to the bilateral testis [6]. Patients generally present with testicular swelling with or without pain during the course of treatment of primary prostatic carcinoma as reported by Kusaka et al., in which the patient developed testicular mass four years after primary treatment with radiotherapy and hormonal therapy [7,8]. However, in our case, the patient was asymptomatic and he neither had any testicular mass nor pain and secondary testicular metastasis was incidentally detected in the orchiectomy specimen at the time of diagnosis of primary prostatic adenocarcinoma.
Prostatic cancer usually spreads to the testis via lymphatic or venous routes or through direct extension via vas deferens, and seldom invades the interstitium through the seminiferous tubules [9,10]. Probable route of spread to the testis in our case could be via lymphatics as lymphovascular invasion was evident both in the testis and in the resected margin of spermatic cord. Also, whole testicular tissue should be prepared and examined microscopically because macroscopic dissection of the testis may not show the metastatic lesion in all cases [11]. A review of 26 non-incidental cases of testicular metastases revealed that the prostate was the most common primary site (11 cases). Seven of the 11 patients developed clinically apparent testicular masses [12]. Other most common primary sites of metastases to testis are from lung, skin (malignant melanoma), colon and kidney in order of decreasing frequency.
Conclusion
Hence, all testicular specimens removed for early or delayed hormonal therapy of prostate cancer should be subjected to routine microscopic histologic examination. This may not change the line of management but can have an impact on prognosis as they tend to behave aggressively and further studies may be needed to analyze any role of adding local radiation in such cases of testicular involvement with lymphovascular invasion of the resection margins.
[1]. Gandaglia G, Abdollah F, Schiffmann J, Distribution of metastatic sites in patients with prostate cancer: A population-based analysisProstate 2014 74(2):210-6.doi: 10.1002/pros.22742. Epub 2013 Oct 16 [Google Scholar]
[2]. Haupt B, Ro JY, Ayala AG, Zhai J, Metastatic prostatic carcinoma to testis: Histological features mimicking lymphomaInt J Clin Exp Pathol 2009 2:104-07. [Google Scholar]
[3]. Semans JH, Carcinoma of the prostate with metastases to the testesJ Urol 1938 40:524 [Google Scholar]
[4]. Kırkali Z, Reid R, Deane RF, Silent testicular metastasis from carcinoma of the prostateBr J Urol 1990 66:205-07. [Google Scholar]
[5]. Richie JP, Walsh PC, Retik AB, Stamey TA, Vaughan ED, Neoplasm of the testis Campbells urology 1992 PhiladelphiaWB Saunders:1222-1263. [Google Scholar]
[6]. Kim SO, Choi YD, Jung SI, Oh KJ, Im CM, Kang TW, Prostate cancer with solitary metastases to the bilateral testisYonsei Med J 2011 52:362-64. [Google Scholar]
[7]. Kusaka A, Koie T, Yamamoto H, Testicular Metastasis of Prostate Cancer: A Case ReportCase Rep Oncol 2014 7:643-47. [Google Scholar]
[8]. Kwon SY, Jung HS, Lee JG, Solitary Testicular Metastasis of Prostate Cancer Mimicking Primary Testicular CancerKorean J Urol 2011 52:718-20. [Google Scholar]
[9]. Pienkos EJ, Jablokow VR, Secondary testicular tumoursCancer 1972 30:481-85. [Google Scholar]
[10]. Sinngh M, Samaratunga C, Wright C, Guaydalini I, Prostatic carcinoma metastasizing to the testis- an unusual pattern of spreadBr J Urol 1995 75:803-04. [Google Scholar]
[11]. Baykal K, Yildirim S, Inal H, Metastasis of Prostate Adenocarcinoma to TestisInt J Urol 1997 4:104-05. [Google Scholar]
[12]. Ulbright TM, Young RH, Metastatic carcinoma to the testis. A clinicopathology analysis of 26 nonincidental cases with emphasis on deceptive featuresAm J Surg Pathol 2008 32:1683-93. [Google Scholar]