Head neck cancers (HNC) are the sixth most common cancer worldwide. In presence of the complex anatomy of this region, early diagnosis can sometimes be a challenge. At present for the TNM staging, contrast enhanced CT and MRI are the primary imaging modalities for evaluating T stage of HNSCC. Multiple studies suggest that PET/CT might be superior to conventional imaging (CT or MRI) in initial staging and may alter management and treatment especially when distant metastases are discovered. We present a case of a 35-year-old patient who presented to us with an ulcerative lesion on the left buccal mucosa, which was staged as cT2N0M0, using the conventional radiology. But on subsequent imaging by PET-CT with MR-fusion was upstaged to cT4bN0M0, thus completely changing the management of the patient. With the recent advances in technology leading to fusion of MRI images with PET-CT images have combined the benefits of all three imaging modalities and has led to increased sensitivity towards soft tissue and peri-neural invasion of tumours leading to upstaging of primary oral cavity malignancies, altering their management. Accuracy is increased when the information of multiple imaging modalities are analysed together and has the potential of changing the management plan of patients.
Case Report
A 35-year-old gentleman presented to the outpatient department of Department of Head-Neck Oncology with complaint of a non-healing ulcer over the left buccal mucosa for the last 1.5 months, with a history of decreased mouth opening for the last two years. He also complained of pain at the site, with repeated bouts of left sided headaches, which worsened in the last 15 days. There was no associated history of bleeding or loosening of teeth. Patient gave a history of chewing of areca nut for the last seven years. No other addictions were present.
On examination of the patient, oral cavity examination revealed grade II trismus with inter-incisor distance ~ 2.5 cm, with presence of oral sub-mucous fibrosis. The dental condition was fair. There was a 3×2cm ulcerative lesion present on the anterior left buccal mucosa opposite the left lower canine and first premolar, with involvement of left lower gingivo-buccal sulcus (GBS) and buccal surface of left lower alveolus around the canine and first pre-molar. There were no neck nodes palpable bilaterally. No other significant clinical finding was present [Table/Fig-1].
Clinical photograph of the ulcero-proliferative lesion involving left lower bucco-alveolar sulcus, left lower buccal mucosa and the buccal side of left lower alveolus.

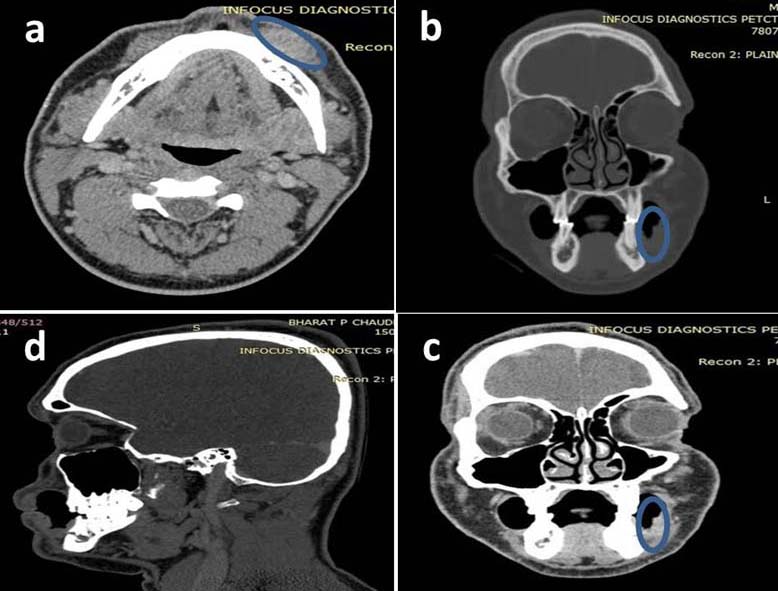
The patient had come with a contrast enhanced computed tomography (CECT) from the base of skull to the clavicle, which showed a 2.8×1.7×0.3cm heterogeneously enhancing soft tissue lesion involving the left anterior buccal mucosa, left lower GBS and the left lower alveolar mucosa in the region of the canine and first premolar, with no involvement of the muscles in the buccal space and no erosion of the mandible. Few sub-centimetric lymph nodes were present in left level Ib, which were reported as being reactive lymph nodes [Table/Fig-2]. The biopsy of the lesion was performed and reported as well differentiated squamous cell carcinoma.
Contrast enhanced computed tomography (CECT) along with bony windows axil, coronal and sagittal view of an heterogeneously enhancing soft tissue density involving the left lower BA sulcus, left lower buccal mucosa and the left lower alveolus with no underlying erosion of the mandible. (Blue circle demarcates the lesion)
On the basis of the clinical and the radiological examination and on the basis of the seventh edition AJCC classification [1], the patient was staged as cT2N0M0.
In view of recent onset left sided headache, which was an alarming sign and to complete the whole body metastatic work-up, the patient was advised to undergo PET-CT with MR fusion.
On the next day the patient underwent a whole body PET-CT using a PET-CT Discovery 600 system with 16 slice CT scanner. The patient was injected with 9.0 mCi of FDG intravenously and images were taken after 1 hour. Limited MRI of local region was performed and images of PET-CT and MRI were fused to obtain the final report.
PET-CT with MR fusion reported a heterogeneously enhancing hypermetabolic lesion seen involving left anterior buccal mucosa involving left lower GBS. It measured 3.3×1.9×0.4cm and revealed moderate FDG uptake (SUV max: 6.8). Lesion extended along the outer cortex of the mandible without definitive erosion of the underlying bone. Lesion extended at left mental foramen with perineural extension of the disease along the infra-alveolar nerve upto foramen ovale, which was better appreciated and confirmed on the PET-CT with MR fusion images. No other FDG avid lesion was seen anywhere else in the body [Table/Fig-3].
PET-CT with MR fusion images (Axial and coronal) pre-NACT, showing an FDG avid lesion, 3.3×1.9×0.4cm, with SUV max. of 6.8 involving the left lower BA sulcus and left lower buccal mucosa, abutting the mandible. The MR images were suggestive of perineural involvement of the inferior alveolar nerve from the mental foramen to the foramen ovale (Blue arrow)
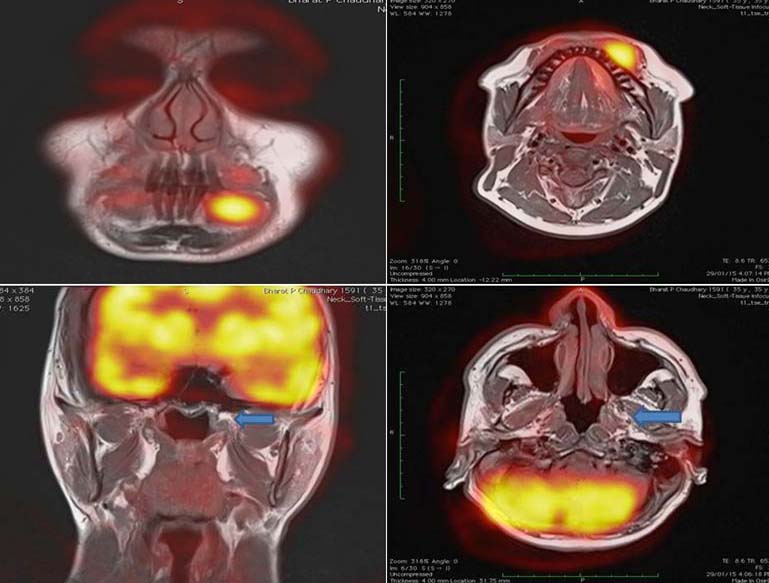
With this imaging the clinical staging of the patient was changed from the initial cT2N0M0, Stage II to cT4bN0M0, Stage IVB, which completely changed the management of the patient. The patient, from being a candidate for an upfront surgical resection, with a five year disease free survival of about 60% became a candidate requiring an adjuvant treatment in form of neo-adjuvant chemotherapy and post-operative Chemoradiation after surgery, with a five year disease free survival falling to about 30-35%.
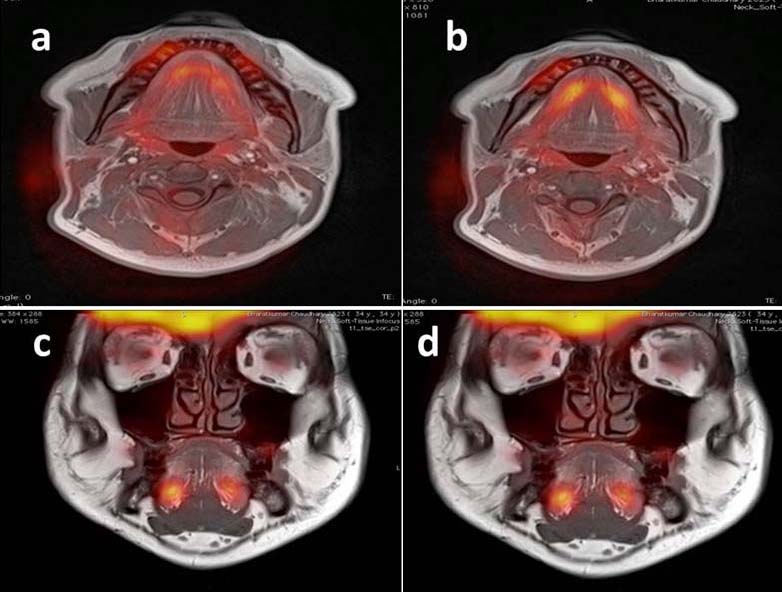
In view of clinically advanced borderline inoperable disease, the patient was initially advised three cycles of neo-adjuvant chemotherapy (NACT) in the form of Inj. Cisplatin + Inj. 5-Flurouracil + Inj. Docetaxel. After three cycles of NACT a repeat PET-CT with MR fusion was done to document the response and to evaluate if the patient was now a candidate for surgery. The repeat PET-CT with MR fusion showed approx. 80% reduction in the tumour burden, with absent peri-neural spread in this scan [Table/Fig-4]. Subsequently the patient was taken up for surgery and underwent left composite resection (Wide excision of left buccal mucosa with left hemi-mandibulectomy with left infratemporal fossa clearance with selective neck dissection (I-III) with reconstruction of the defect by left pectoralis major myocutaneous flap [Table/Fig-5].
PET-CT with MR fusion images (Axial and coronal) after three cycles of NACT, showing almost complete radiological and metabolic response in the primary and in the perineural spread along the inferior alveolar nerve.
Intraoperative specimen of left hemi-mandibulectomy with wide excision left buccal mucosal and left infra-temporal fossa showing an ulcerative lesion involving the left bucco-alveolar sulcus
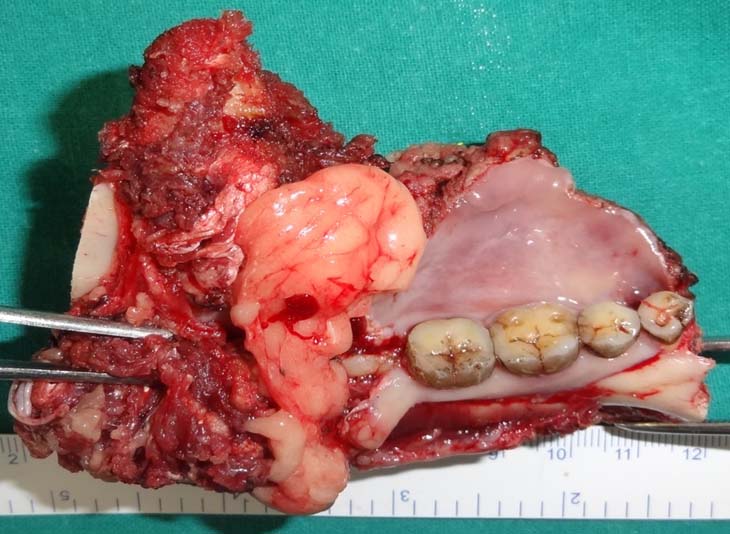
His postoperative biopsy was moderately differentiated squamous cell carcinoma (0.6×0.5cm) with depth of invasion of 0.3cm. No lympho-vascular and peri-neural invasion was seen. 0/22 lymph nodes were positive. The cut end of inferior alveolar nerve at the foramen ovale was negative for malignant cells. The mandibular bone was free of tumour. (yPT1N0M0, Stage 1). The biopsy was positive for cytokeratin on Immuno-histochemistry. A metallic pin was placed as a guide at the proximal cut end of the nerve at the foramen ovale for the post-operative radiotherapy planning [Table/Fig-6].
Postoperative coronal non-contrast CT scan showing the post-operative hemi-mandibulectomy status with a presence of a metallic pin at the left foramen ovale at the site of cut end of inferior alveolar nerve for guidance for postoperative radiotherapy

Discussion
Head and neck cancers are the sixth most common malignancy in the world. India shares the largest burden of the world head and neck cancer cases, with an estimated 200,000 cases of head and neck cancers occurring each year in India. Nearly 80,000 oral cancers are diagnosed every year in India [2].
Due to a complex anatomy and many areas remain hidden from sight (like oropharynx, base of tongue, paranasal sinuses, subglottis, hypopharynx, etc.) for proper examination using detailed physical examination, rigid or flexible endoscopy and the routine radiological examination. This and the non-specific presentation of malignancy arising from these sites make the early diagnosis very difficult in some cases, leading to a delay in diagnosis and subsequent treatment and poorer prognosis.
In the present case TNM staging of oral cavity malignancies, contrast enhanced CT and MRI are used as the primary imaging modalities for evaluating T stage of head and neck squamous cell carcinoma (HNSCC) due to their superior anatomic resolution and tissue contrast. According to the present guidelines, there are no clear recommendations for the use of PET/CTfor staging of head and neck cancers. In a study by Ha et al., they found that PET/CT upstaged T staging in 2 of 36 patients (5.5%) with subsequent changes in treatment planning [3]. Similarly in a prospective study by Scott and colleagues showed that PET changed T staging in 6 of 71 patients (8.5%) [4]. Similarly in a study by Lonneux et al., to evaluate the impact of PET/CT on the initial staging and management of patients with HNSCC [5]. The group found that PET/CT improved the TNM classification of the disease and altered the management of 13.7% of the patients mainly due to the ability of PET/CT to detect metastatic or additional disease.
For the evaluation of the bony involvement by the tumour and the malignancies involving the larynx, CT remains the imaging modality of choice [6]. For the malignancies of the oropharynx, nasopharynx, oral cavity, assessment of bone marrow involvement and the perineural spread, MRI is the modality of choice [7,8].
Status and extent of mandible or bony involvement by the primary malignancy is one of the most important factors in determining the treatment plan for the malignancy. Superficial mandibular erosion by an early resectable oral cavity cancer can be treated by a marginal (vertical or horizontal) mandibulectomy preserving the mandibular bony arch, whereas a gross involvement of the mandible by the tumour requires a segmental or hemi-mandibulectomy with a composite free flap reconstruction [9]. Traditionally CT is superior to MRI for assessment of the cortical bone involvement by the tumour. Metabolic activity registered by PET in cases of mandible involvement tends to overestimate the involvement by the tumour due to partial volume averaging and misresgistration artefact. The CT portion of the PET/CT and CECT has a better sensitivity for bony involvement [10].
Another important factor to be assessed in cases of oral cavity malignancies is the presence of perineural spread. Perineural spread of the tumour occurs due to the spread of the tumour cells along the peripheral nerves below the epineurium of the nerve. This leads to spread of the tumour from the primary site to a distant site, leading to poor prognosis as seen in our case. The patient might not have any symptoms at the time of presentation and the perineural spread might be detected at the time of surgery only [11]. MRI is the imaging modality of choice to detect perineural spread due to its high tissue contrast. But certain features on PET/CT might also point towards perineural involvement by the tumour like abnormal linear or curvilinear hypermetabolic activity along the trigeminal or facial nerves [7].
Prior to treatment planning for a case of head and neck cancer a whole body imaging for detection of distant metastasis is a pre-requisite. A presence of distant metastasis changes the treatment from a curative intent to a palliative treatment. In a study by Gourin et al., approximately 7% to 25% of patients with advanced stage HNSCC had distant metastases at initial presentation [12]. The most common sites of metastasis include lung, bone and abdomen [2]. Contrast enhanced chest CT is commonly used to assess intra-thoracic spread with 73% sensitivity and 80% specificity [13]. Overall PET/CT is more accurate than conventional imaging in detecting metastatic foci [14]. A meta-analysis by Xu et al., revealed sensitivity and specificity of PET/CT around 87.5 % and 95% respectively [15]. Thus in the present scenario, PET/CT is considered to be the imaging modality of choice to detect distant metastasis. But a negative PET/CT does not completely exclude absence of metastasis [15].
However, all imaging modalities have some inherent shortcomings. CT imaging in oral cavity can be greatly affected by dental fillings and amalgam which can degrade the quality of imaging. PET and MRI are less affected by this type of artefact. Various implants like cochlear implants and pacemakers can prevent the usage of MRI; also the image quality can be hampered by motion artefacts. PET imaging alone or PET-CT has a poor sensitivity, with high false positive rates in area of the Waldeyer’s ring in the oropharynx due to the normal lymphoid uptake in this region. Also, Seitz et al., in their study demonstrated that addition of MRI to PET-CT had no additional value in T staging of the oral and oropharyngeal cancers when compared to histopathology, which is the gold standard. This is believed to be due to a limit in the spatial resolution of PET-CT when it comes to detection of small, superficial lesions and also in lesions obscured by dental implant artefacts [16]. One of the major and unique advantages of PET-CT is its ability to demarcate the full anatomical extent of the tumour when the tumour is ill-defined, like in cases with submucosal extension or diffuse infiltration.
With the use of PET-CT with MR-fusion for the preoperative metastatic workup, the benefits of all three imaging modalities could be combined, with an improvement of overall diagnosis of loco-regionally advanced disease and the possibility of systemic metastasis which has the potential of changing the treatment plan for a patient. CT part of the imaging provides sensitive information about the bony involvement, with MRI providing better information about the soft tissue and perineural spread, with the PET imaging helps in delineating the exact extent of tumour along with extent of lymph node involvement and the distant metastasis. Accuracy is increased when the information of multiple imaging modalities are analysed together [17].
Conclusion
CT and MRI have been conventionally used in the pre-operative metastatic work-up of the patient. PET has improved the sensitivity and specificity of primary tumour extent, lymph nodal status and the distant metastasis. The recent advancement in imaging technology with fusion of MRI images along with the PET-CT in PET-CT with MR fusion combines the advantages of all three imaging modalities and improves the diagnosis. Accuracy is increased when the information of multiple imaging modalities are analysed together and has the potential of changing the management plan of patients.
[1]. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, Cancer Staging Handbook from AJCC Cancer Staging Manual 2010 7th edNew YorkSpringer:39-126. [Google Scholar]
[2]. Head and Neck Cancer in India. Available from: http://www.veedaoncology.com/PDF-Document/Head-Neck%20Cancer%20In%20India.pdf [Google Scholar]
[3]. Ha PK, Hdeib A, Goldenberg D, Jacene H, Patel P, Koch W, The role of positron emission tomography and computed tomography fusion in the management of early-stage and advanced-stage primary head and neck squamous cell carcinomaArch Otolaryngol Head Neck Surg 2006 132:12-16. [Google Scholar]
[4]. Scott AM, Gunawardana DH, Bartholomeusz D, Ramshaw JE, Lin P, PET changes management and improves prognostic stratification in patients with head and neck cancer: results of a multicenter prospective studyJ Nucl Med 2008 49:1593-600. [Google Scholar]
[5]. Lonneux M, Hamoir M, Reychler H, Maingon P, Duvillard C, Calais G, Positron emission tomography with [18F]-fluorodeoxyglucose improves staging and patient management in patients with head and neck squamous cell carcinoma: a multicentre prospective studyJ Clin Oncol 2010 28:1190-95. [Google Scholar]
[6]. Zbären P, Becker M, Läng H, Pre-therapeutic staging of hypopharyngeal carcinoma. Clinical findings, computed tomography, and magnetic resonance imaging compared with histopathologic evaluationArch Otolaryngol Head Neck Surg 1997 123:908-13. [Google Scholar]
[7]. Paes FM, Singer AD, Checkver AN, Palmquist RA, De La Vega G, Sidani C, Perineural spread in head and neck malignancies: clinical significance and evaluation with 18F-FDG PET/CTRadiographics 2013 33:1717-36. [Google Scholar]
[8]. Ng SH, Chan SC, Yen TC, Chang JT, Liao CT, Ko SF, Staging of untreated nasopharyngeal carcinoma with PET/CT: comparison with conventional imaging work-upEur J Nucl Med Mol Imaging 2009 36:12-22. [Google Scholar]
[9]. Politi M, Costa F, Robiony M, Rinaldo A, Ferlito A, Review of segmental and marginal resection of the mandible in patients with oral cancerActa Otolaryngol 2000 120:569-79. [Google Scholar]
[10]. Goerres GW, Schmid DT, Schuknecht B, Eyrich GK, Bone invasion in patients with oral cavity cancer: comparison of conventional CT with PET/CT and SPECT/CTRadiology 2005 237:281-87. [Google Scholar]
[11]. Liebig C, Ayala G, Wilks JA, Berger DH, Albo D, Perineural invasion in cancer: a review of the literatureCancer 2009 115:3379-91. [Google Scholar]
[12]. Gourin CG, Watts TL, Williams HT, Patel VS, Bilodeau PA, Coleman TA, Identification of distant metastases with positron-emission tomography-computed tomography in patients with previously untreated head and neck cancerLaryngoscope 2008 118:671-75. [Google Scholar]
[13]. Brouwer J, de Bree R, Hoekstra OS, Golding RP, Langendijk JA, Castelijns JA, Screening for distant metastases in patients with head and neck cancer: is chest computed tomography sufficient?Laryngoscope 2005 115:1813-17. [Google Scholar]
[14]. Yoo J, Henderson S, Walker-Dilks C, Evidence-based guideline recommendations on the use of positron emission tomography imaging in head and neck cancerClin Oncol (R CollRadiol) 2013 25:e33-66. [Google Scholar]
[15]. Xu GZ, Zhu XD, Li MY, Accuracy of whole-body PET and PET-CT in initial M staging of head and neck cancer: a meta-analysisHead Neck 2011 33:87-94. [Google Scholar]
[16]. Seitz O, Chambron-Pinho N, Middendorp M, Sader R, Mack M, Vogl TJ, 18 F-Fluorodeoxyglucose-PET/CT to evaluate tumour, nodal disease, and gross tumour volume of oropharyngeal and oral cavity cancer: comparison with MR imaging and validation with surgical specimenNeuroradiology 2009 51:677-86. [Google Scholar]
[17]. Gu DH, Yoon DY, Park CH, Chang SK, Lim KJ, Seo YL, CT, MR, (18) F-FDG PET/CT, and their combined use for the assessment of mandibular invasion by squamous cell carcinomas of the oral cavityActa Radiol 2010 51:1111-19. [Google Scholar]