High Resolution Ultrasound in Disseminated Soft Tissue, Muscular and Glandular Cysticercosis
Rashmi M Nagaraju1, Bhimarao2
1 Assistant Professor, Department of Radiodiagnosis, P K Das Institute of Medical Sciences, Palakkad, Kerala, India.
2 Senior Resident, Department of Radiodiagnosis, P K Das Institute of Medical Sciences, Palakkad, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rashmi M Nagaraju, Nagambika Nilaya, No 86, Shivapura, Srirampura Post, Manandavadi Road, Mysore- 570008, Karnataka, India. E-mail : rashmi83nagaraj@gmail.com
High frequency, Parasitic infection, Proptosis, Taenia solium
A 20-year-old female [Table/Fig-1] presented with diffuse nodular swellings over entire body and bilateral proptosis since 3 months. The swellings were subcutaneous, firm and mildly tender. Bilateral axial proptosis was noted. Her systemic examination was normal. Laboratory tests showed mild eosinophilia.
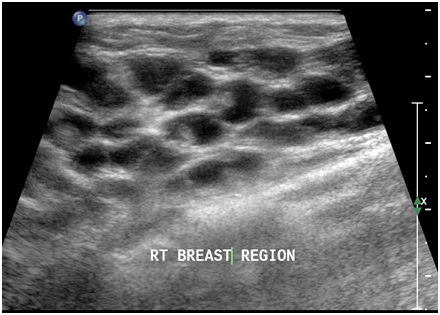
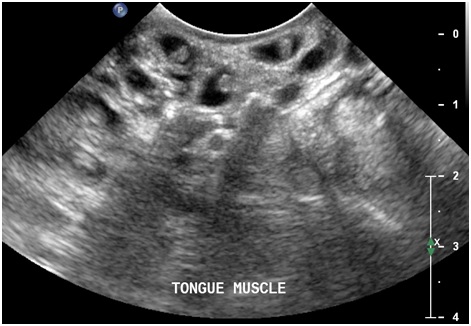
Photograph of the patient showing nodular and oedematous face and neck with nodular swelling in tongue

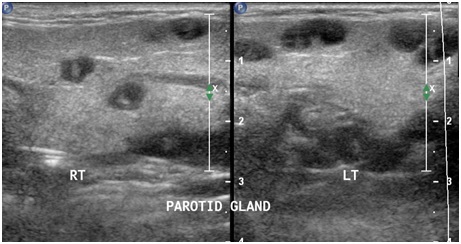
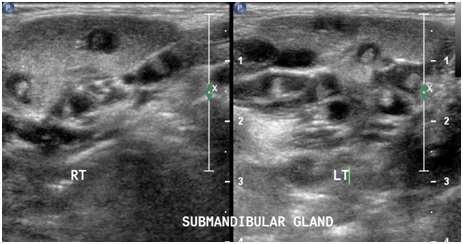
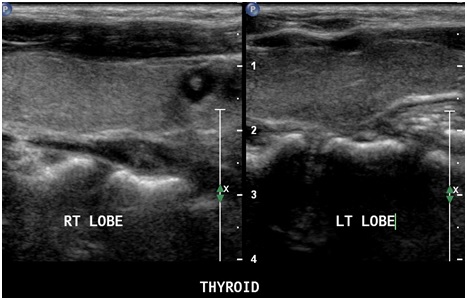
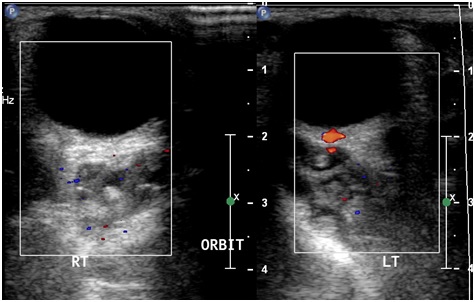
Ultrasound using high frequency linear probe (3 to 9MHz) of Philips IU22 unit, revealed multiple round to oval thin walled anechoic cysts of ~ 8 to 10 mm demonstrating eccentric echogenic nodule, representing scolex. These lesions were diffusely dispersed in subcutaneous tissue, superficial muscular plane of face and neck, bilateral parotid glands [Table/Fig-2], sub mandibular glands [Table/Fig-3] and thyroid gland [Table/Fig-4]. The bilateral extra-ocular muscles were involved with axial proptosis [Table/Fig-5]. Multiple lesions were noted in both breasts [Table/Fig-6], upper and lower limb muscles, anterior abdominal wall & back muscles and tongue muscles [Table/Fig-7] with longitudinal orientation of lesion along the muscle fibers. The solid abdominal organs and cardiac muscles were normal. Plain and contrast CT of brain showed no obvious evidence of neurocysticercosis.
Cysticercal cysts in both parotid glands
Cysticercal cysts in both submandibular glands
Cysticercal cyst in right lobe of thyroid
Cysticercal cysts in extra ocular muscles of both eyes
Cysticercal cysts in right breast parenchyma
Cysticercal cysts in tongue muscles
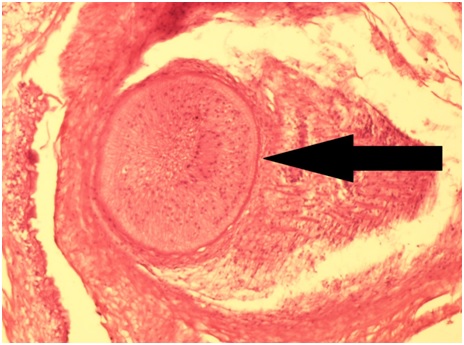
Excisional biopsy revealed encysted cysticercal larva with adjacent inflammatory exudate [Table/Fig-8]. Oral albendazole therapy with anti-inflammatory agents were commenced and follow up after 3 months showed significant decrease in the size & number of lesions with resolution of generalized oedema and tenderness.
Histopathology (H&E staining) showing encysted cysticercal larva with adjacent inflammation
Cysticercosis is the commonest parasitic infection of the soft tissues worldwide [1], caused by larval forms of pork tapeworm Taenia solium with humans being intermediate/definitive host [2]. Till date approximately 50 cases of disseminated cysticercosis have been reported involving various organ systems [3]. Glandular [4,5] (parotid, submandibular and thyroid gland), breast [6] and tongue muscle [7] involvement is extremely rare with only few isolated case reports showing solitary lesions.
High-frequency USG is a simple non invasive modality for the characterization of such cases [8]. The common USG appearances of soft tissue cysticercosis includes intramuscular abscess with eccentrically situated typical cyst with scolex within /typical cysticercosis cyst with scolex within/irregular cyst with no scolex [8]. On MRI it is seen as cystic lesion appearing hyperintense on T2W, hypointense on T1W images with eccentric hypointense scolex [9].
Histopathology is required for confirmation, which shows portions of Cysticercus cellulosae. At times, the larval parts may not be seen in the specimen, but an inflammatory reaction with eosinophils and histiocytes may be seen [9,10].
Treatment of soft tissue cysticercosis depends on the location [1]. They can be surgically excised if solitary or associated with abscess. Antihelminthic medications such as albendazole or praziquantel are used for uncomplicated cases. These cases are followed up with USG after three weeks to look for resolution.
[1]. Kraft R, Cysticercosis: An emerging parasitic diseaseAm Fam Physician 2007 75:91-6.:98 [Google Scholar]
[2]. Baily GG, Cysticercosis. In: Cook GC, Zumla A, editorsManson’s Tropical Disease 2003 21st edLondonWB Saunders:1584-95. [Google Scholar]
[3]. Bhalla A, Sood A, Sachdev A, Varma V, Disseminated cysticercosis: a case report and review of the literatureJ Med Case Reports 2008 2:137 [Google Scholar]
[4]. Goyal P, Ghosh S, Sehgal S, Mittal D, Singh S, Solitary cysticercosis of parotid gland diagnosed on FNACAPSP J Case Rep 2014 5(1):11 [Google Scholar]
[5]. Gupta S, Sodhani P, Clinically unsuspected thyroid involvement in cysticercosis: a case reportActa Cytol 2010 54(5 Suppl):8536 [Google Scholar]
[6]. Smriti A, Om Prakash T, Sujata P, Ritu B, Cysticercosis of Breast – A Case ReportPol J Pathol 2006 57(1):53-64. [Google Scholar]
[7]. Dhar M, Ahmad S, Srivastava S, Shirazi N, Dissemniated cysticercosis: Uncommon presentation of a common diseaseAnn Trop Med Public Health 2013 6:317-20. [Google Scholar]
[8]. Deepti N, Srinath MG, Ashok K, Soft tissue cysticercosis - Ultrasonographic spectrum of the diseaseIndian Journal of Radiology and Imaging 2011 21(1) [Google Scholar]
[9]. Jhankaria BG, Chavhan GB, Krishnan P, Jhankaria B, MRI and ultrasound in solitary muscular and soft tissue cysticercosisSkeletal Radiol 2005 34:722-26. [Google Scholar]
[10]. Bothale KA, Mahore SD, Maimoon SA, A rare case of disseminated cysticercosisTrop Parasitol 2012 2(2):138-41. [Google Scholar]