Tuberculosis (TB) is still the most rampant infectious disease in developing countries including India [1]. Incidence is increasing globally due to retro viral infection [2]. Lymphnodes are the common sites involved in extrapulmonary tuberculosis (EPTB). Incidence of EPTB varies, accounting for 15-20% in immune-competent cases and 50% in immune-compromised cases [3]. Fine needle aspiration cytology (FNAC) is still the prime diagnostic modality for investigation of lymphadenopathy [1]. Diagnosis of tuberculosis is based on the observation of epithelioid cell granuloma, necrosis and acid fast bacilli (AFB). Identification of AFB in Ziehl-Neilsen stained smear (ZN), still remains as gold standard for diagnosis of TB, however in some of the cases, AFB may not be demonstrated causing diagnostic difficulties [1,4,5].
To evaluate the correlation between AFB and ES in necrotic lymphnode aspirates.
Materials and Methods
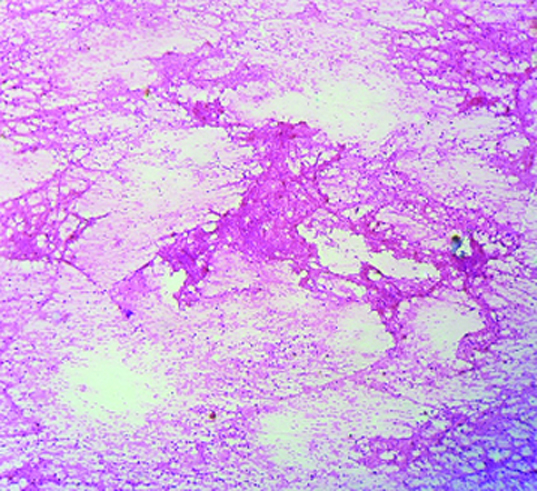
This is a retrospective study conducted in the Department of Pathology Employees’ State Insurance Corporation Medical College and PGIMSR from January 2014 to December 2014. Lymphnodes upon purulent aspiration which were reported as granulomatous lymphadenitis suggestive of tuberculosis were included in the study. Those yielded haemorrhagic aspirates were excluded. The patient’s clinical details were retrieved from case files. All the stained smears (Haematoxylin & Eosin (H&E), May Grunwald Gimsa (MGG) and ZN stain for each case were retrieved from the departmental file and rescreened independently by two pathologists for the presence of eosinophilic structure (ES), granulomas and AFB. In cases where ZN stained smears were not available, H&E and MGG stained smears were decolourised with acid alcohol and re stained with ZN. ‘Eosinophilic structure’ first described by Pandit et al., [4]. Due to the eosinophilic appearance on H&E stain, these structures appear basophilic in MGG stain and bluish in ZN stain. Morphologically they are acellular, homogenous, irregular structure with well defined margins [Table/Fig-1]. Immunohistochemically/cytochemically positive for tubercular antigen [4,5]. Treatment history and response to Anti-tubercular treatment were enquired from RNTCP centre.
Microphotograph of lymphnode aspirate showing eosinophilic structure in the back ground of necrosis. (H&E, 40X)
Statistical Analysis
Statistical analysis was done using Chi-square test.
Results
We retrieved 103 cases of necrotic aspirates. Our cases ranged from 6 to 69 years, the common age group involved was 21-40 years, and with male to female ratio of 0.56:1 (male (36), female (64) cases [Table/Fig-2]). Cervical, axillary and inguinal lymphnodes were involved in 90 cases (87%), 9 cases (8.7%) and 4 cases (3.8%) respectively.
Showing correlation between eosinophilic structure and acid fast bacilli
| Cytology picture | Number of cases | ECG | ES | AFB |
|---|
| ES- and AFB- | 31 | 26 | 0 | 0 |
| ES-and AFB+ | 17 | 14 | 0 | 17 |
| ES+ AFB+ | 40 | 32 | 40 | 40 |
| ES+ AFB- | 15 | 12 | 15 | 0 |
| 103 | 84 (81.5%) | 55 (53%) | 57 (55.5%) |
ES: Eosinophilic structure, AFB: Acid fast bacilli, ECG: Epithelioid cell granulomas
Out of 103 cases, epithelioid granulomas were observed in 84 (81.5%) cases, AFB in 57 (55.5%) cases and ES in 55 (53%) cases. In 30 (29%) cases all the three components were positive i.e ES, AFB and granulomas. In only two cases all there were negative and based on the presence of caseous necrotic material the lesions are diagnosed as tuberculosis.
In relation to ES and AFB, four different cytological pictures were seen.
Eosinophilic Structure Negative (-) & Acid Fast Bacilli Negative (-): This combination was observed in 31 (30%) cases, 26 cases in addition showed epithelioid granulomas.
Eosinophilic Structure Negative (-) & Acid Fast Bacilli Positive (+): This combination was observed in 17 (16.5%) cases, 14 cases in addition showed epithelioid granulomas.
Eosinophilic Structure Positive (+) & Acid Fast Bacilli positive (+): This is the most common combination and was observed in 40 cases (39%). 32 cases in addition showed epithelioid granulomas.
Eosinophilic Structure Positive (+) & Acid Fast Bacilli Negative (-): This is combination was observed in 15 (14.5%) cases, 12 cases also showed epithelioid granulomas [Table/Fig-2].
Chi-square test showed a highly significant statistical association between ES and AFB with p-value of 0.001.
Out of 103 cases, treatment history was available for 37 cases. Ten patients completed the treatment regimen, 9 were symptom free and one patient showed recurrence. Twenty seven cases are still on treatment with improvement in clinical symptoms.
Discussion
In the era of newer diagnostic modalities, FNAC is still considered as first line investigation in TB lymphadenopathy [6]. The cytodiagnosis of tuberculosis lymphadenitis is based on observation of epithelioid cell granuloma and caseous necrosis [4,5]. As there are many aetiologies for granulomatous lymphadenitis like sarcoidosis, leprosy, catstractch disease, brucellosis and others. A definitive diagnosis of TB relays on identification of AFB in ZN stain [7].
AFB positivity depends on both bacterial and tissue factors. Intactness of the bacteria is essential, along with tissue factors like presence of granulomas, necrosis, oxygen concentration and pH of the lesion [8]. AFB positivity varies in different reported series. Metre and Jayram reported 66% positivity, Gupta et al., reported 75.6%, Parsoon et al., 67.6%, Pandit et al., 85.7%, Das et al., 86%, and Arora et al., 100% [4,5,9–12]. AFB positivity in our study was 55.5%. In AFB negative cases aetiological diagnosis of TB can be established by other tests like Polymerized Chain Reaction, fluorescent microscopic examination and culture, but they are expensive and time consuming [12–14]. On other hand, screening of FNAC smears for ES helps in aetiological diagnosis of TB, which is simple, easily available and economical.
Pandit et al., described the morphological features of ES, as degenerated granulomas, which are acellular, associated with caseous necrosis, immunohisto/cytochemically shows presence of mycobacterial antigen and they are confined to tuberculosis necrotic lesions [4]. ES appears as pink, homogenous, acellular, irregular structure with well defined margins on H&E stain, basophilic in Leishman stain and bluish in ZN stain [4,5]. Formation of granuloma is an example of delayed type hypersensitivity reaction. Upto 3 weeks of infection, mycobacterial bacilli are phagocytosed by macrophages and it is unable to kill the organism, leading to unchecked bacterial proliferation within the macrophage. After 3 weeks, TH1 immune response against mycobacterial TB is mounted upon antigen presentation by macrophage, the TH1 cells secrete interferon γ and other cytokines leading to conversion of macrophage into epitheloid cells and giant cells thus forming granuloma. As the accumulation of granulomas increase, tissue destruction takes place leading to caseous necrosis [7].
With respect to ES and AFB four different stages occurs in granulomas. Initial stage, which is observed in people with good immunity, where ES and AFB are negative (ES-, AFB-), however granulomas are observed. As the granulomas degenerate producing caseous necrosis, mycobacterium is demonstrated in the lesion (ES-, AFB+). Later further degeneration of granulomas leads to acellularity leading to ES formation (ES+, AFB+). Necrosis decreases the pH and creates anaerobic environment leading to death of organism (as they are strict aerobe) producing stage of AFB negativity however ES are still demonstrable (ES+, AFB-). Still further anaerobic condition increases both ES and AFB disappear leading to ES- and AFB- [5]. ES-AFB – stage is quite interesting, as it is observed in both the ends of spectrum. Presence of Granulomas in the initial phase and caseous necrotic material in the last stage helps in the diagnosis.
Pandit et al., in his study on 70 tuberculosis smears observed, AFB positivity in 85.7% and ES positivity in 44% (31 cases) . He also had observed that ES were positive for tubercular antigen by immunocytochemistry and concluded that ES can be considered as degerative granulomas and its presence indicate the tuberculosis aetiology of the lesion, but they did not correlate between ES and AFB [4]. In another similar study by Prasoon et al., on 108 cases he classified the cases into ES+ AFB+ (63cases), ES+ AFB- (22cases), ES+ AFB-(10 cases) and both negative in 13 cases. AFB and ES positivity was observed in 67.59% and 78.7% respectively. There was a significant statistical association between AFB and ES with p-value of 0.00113, they also suggested that ES can be used in place of AFB in diagnosis of TB [5]. In the present study AFB positivity was observed in 55.5% and ES positivity in 53% and it was statistically significant with a p-value of 0.001. It is evident from the review of literature and also from our study that ES is having same diagnostic accuracy as that of AFB and their identification in AFB negative cases helps in considering the lesion has tubercular origin.
Conclusion
As TB is rampant in under-developed and developing countries, where expenditure on health policies are minimal and sophisticated diagnostic modalities unreachable to majority of rural population. Observation and documentation of ES in AFB negative granulomatous lymphadenitis will help in aetiological diagnosis of the lesion as TB, hence pathologist should explore for this and it should be included in routine cytology reporting of tuberculosis lymphadenitis.
ES: Eosinophilic structure, AFB: Acid fast bacilli, ECG: Epithelioid cell granulomas